Abstract
Background:
Atypical teratoid/rhabdoid tumor (AT/RT) is a rare pediatric central nervous system malignancy with poor outcome. AT/RT is infrequently located in the spinal cord.
Clinical presentation:
A 16-month-old boy presented with progressive urinary retention and weakness of the lower extremities. Magnetic resonance imaging of the spine revealed an intradural extramedullary mass occupying the spinal canal at the level of T10-L3. The tumor was successfully resected by using neuroendoscopy. Histopathology demonstrated rhabdoid cells with eccentric nuclei and eosinophilic cytoplasmic hyaline inclusions. Immunohistologically, the tumor cells showed positive for epithelial membrane antigen, vimentin and neuron-specific enolase, and negative for integrase interactor 1. After surgery, the patient showed significant improvement in sitting and other neurological signs but presenting with flaccid neurogenic bladder. Intrathecal chemotherapy under European Rhabdoid Registry (EU-RHAB) protocol with Doxorubicin, Carboplatin, Etoposide, Ifosfamide, Vincristine, Cyclophosphamide and Actinomycin-D was given. However, recurrent intradural extramedullary tumor at the level of T11-L2 developed in 3 months.
Conclusion:
We report a young Asian case of AT/RT in thoracolumbar spine with recurrent tumor shortly after complete surgical resection of the tumor.
Similar content being viewed by others
Introduction
Atypical teratoid/rhabdoid tumor (AT/RT) is a rare, highly aggressive and lethal neoplasm of the central nervous system (CNS) that usually occurs in very young children and infants. It may also occur in other anatomic sites, such as the kidneys, liver, abdomen or soft tissues. For CNS AT/RT, the posterior cranial fossa is the most frequent and well-studied location.1 The prevalence of pediatric spinal AT/RT is rare, with a total of 38 cases in the literature between 1987 and 2015.2 To our knowledge, only three cases are reported as presenting in the lumbar area.2–4 We herein report a case of lumbar intradural extramedullary AT/RT in an 1-year 4-month-old boy with review of the literature.
Case report
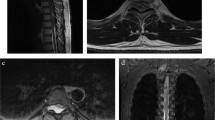
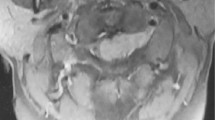
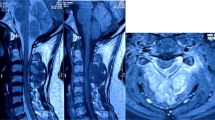
A previously healthy 16-month-old body presented with bowel habit change, urine retention and food refusal for 1 month. He was found unable to walk and had decreasing sitting balance over 7 days. He was irritable, crying and moaning on touching his buttocks. The physical examination showed loss of muscle tone of the lower extremities, but without increased reflexes of lower extremities or positive Babinski sign. Magnetic resonance imaging (MRI) of thoracolumbar spine revealed an intradural, extramedullary mass (0.7×1.1×6.9 cm) occupying the spinal canal at the level of T11-L3. The mass showed isointense to the spinal cord on T2-weighted images and heterogeneous enhancement (Figures 1a and b). The brain MRI revealed normal findings. At 17 months of age, T10-L3 laminectomy was performed, and an intradural extramedullary tumor was found extending from the ventral aspect of conus medullaris and occupying all the space of cauda equina. The tumor seems intimately attached to the conus medullaris under neuroendoscopic inspection. Neuroendoscopic microsurgical resection of the tumor was performed successfully (Figure 2a). Intraoperative squash preparation showed large, pleomorphic, plasmacytoid and polygonal cells with eccentrically placed nuclei and dense amphophilic cytoplasm (Figure 2b). Histopathology demonstrated predominant rhabdoid cells (about 70%) with eccentric nuclei and eosinophilic cytoplasmic hyaline inclusions (Figure 2c). There are also minor components of small cells and spindle cells. Immunohistologically, the tumor cells showed positive for epithelial membrane antigen, vimentin and neuron-specific enolase, and negative for glial fibrillary acidic protein, synaptophysin, smooth muscle actin, integrase interactor 1 (INI-1), progesterone receptor, CD117, or desmin (Figure 2d). The results were consistent with the diagnosis of AT/RT. After surgical management, the patient could sit longer, and muscle power of the lower extremities improved. However, flaccid neurogenic bladder and constipation were still noted. Intrathecal chemotherapy under European Rhabdoid Registry (EU-RHAB) protocol with Doxorubicin, Carboplatin, Etoposide, Ifosfamide, Vincristine, Cyclophosphamide and Actinomycin-D was given. Intermittent urinary infections due to neurogenic bladder were treated with antibiotics. After first course of chemotherapy, he was placed under harvest peripheral blood stem cell for further management. Unfortunately, the follow-up spine MRI at 3 months after surgery showed recurrent tumor at the T11-L2 level (Figure 1c). At 20 months of age, neuroendoscopic microsurgical debulking operation for the recurrent tumor was performed. After surgery, the patient received concurrent chemotherapy (EU-RHAB) and radiotherapy (whole craniospine 2400 cGY and spine boost 3060 cGy). An equivocal small residual tumor (0.5 cm) at T11 level was disclosed on the follow-up MRI after radiotherapy. The general condition of the patient remained good (7 months following initial surgery), except having problems of mild sitting imbalance and neurogenic bladder with urinary retention.
Magnetic resonance imaging of the spine. (a) T2-weighted sagittal image shows an intradural extramedullary mass occupying the spinal canal at the level of T11-L3. (b) Gadolinium-enhanced T1-weighted, fat suppression sagittal image demonstrates heterogeneous enhancement of this mass. (c) Three months post operation, gadolinium-enhanced T1-weighted, fat suppression sagittal image demonstrates recurrent intradural extramedullary mass at the level of T11-L2 (arrows: tumor).
(a) Surgical findings show tumor abutting the caudal equina. Complete resection of the tumor was performed with partial resection of the cauda equina (arrows: tumor). (b) Squash preparation showed large, pleomorphic, plasmacytoid and polygonal cells with eccentric nuclei and dense amphophilic cytoplasm (hematoxylin and eosin; original magnification x400). (c) Histopathologically, there are predominant cells with rhabdoid features including eccentric nuclei, and eosinophilic cytoplasmic hyaline inclusions. (hematoxylin and eosin; original magnification x400). (d) Loss of INI-1 immunoreactivity was seen, characteristic of atypical teratoid rhabdoid tumors. (INI-1; original magnification x400).
Discussion
AT/RT most commonly occurs in the brain, for newborn to 4-year-old children usually in the infratentorial region, and for those older than 5 years commonly in the supratentorial region.5 In a review of the literature, Tekautz et al.5 found only one case involving the spine in 31 patients diagnosed with CNS AT/RT during a 19-year period.6 The cervical and thoracic spinal sections are the most common locations. Our case is probably the youngest reported Asian patient of primary lumbar AT/RT in the literature.
MR imaging findings of AT/RT usually demonstrate a heterogeneous soft tissue mass that shows isointense or hypointense to spinal cord on T2-weighted images. Hemorrhage or calcifications may be seen. The lesions are heterogeneously enhanced, reflecting their histopathologic complexity. The tumor can occur anywhere along the spinal axis and may be intramedullary or intradural extramedullary in origin.1 The differential diagnosis is dependent on the site and origin of the lesion. For an extramedullary lesion, myxopapillary ependymoma, malignant nerve sheath tumor or metastasis should be included in the differential diagnosis. For an intramedullary lesion, it must be differentiated from primitive neuroepithelial tumor, ependymoma, astrocytoma or ganglioglioma.1
Histopathologically, AT/RT showed marked proliferation of cells with a high nuclear to cytoplasmic ration and prominent nucleoli with geographic necrosis. The immunostaining showed negative in INI-1 and positive in the epithelial membrane antigen, vimentin and smooth-muscle antigen. Besides, chromosome 22q11 abnormalities are also detected in the patient as one of the diagnostic clues.7
If AT/RT is discovered at pathology, abdominal imaging to exclude a primary renal tumor and neuroimaging survey of brain to detect CSF seeding should be obtained. On the basis of CNS cancer protocols, surveillance imaging is recommended every 3 months for 1 year following tumor resection.1
Patients with AT/RT have very poor prognosis. The majority develop progression, or recurrence with or without distant metastasis in a year following initial diagnosis. Most accepted poor prognostic factors for patients with AT/RT are in children aged below 2 years and in children who have metastasis at diagnosis.8 Current evidence in limited number of patients suggests that surgical resection is feasible. Approximately one-third of patients with AT/RT can achieve sustained remission after high-dose chemotherapy with autogenic stem cell transplantation. High-dose chemotherapy might be useful in patients with localized metastatic diseases. Radiotherapy should be started as soon as possible in children older than 18 months to control the distant disease. Progression-free survival and overall survival at 2 years are 53% and 70%, respectively.9
We present probably the youngest Asian patient of primary lumbar AT/RT with initial presentation of gradual sitting imbalance, food refusal and urinary retention. However, rapid recurrence of tumor was noted in 3 months after complete resection of tumor and first course of intensive chemotherapy. Debulking surgery of the recurrent tumor followed by concurrent chemotherapy and radiotherapy showed a promising initial result in this patient.
References
Moeller KK, Coventry S, Jernigan S, Moriarty TM . Atypical teratoid/rhabdoid tumor of the spine. AJNR Am J Neuroradiol 2007; 28: 593–595.
Dhir A, Tekautz T, Recinos V, Murphy E, Prayson RA, Ruggieri P et al. Lumbar spinal atypical teratoid rhabdoid tumor. J Clin Neurosci 2015; 22: 1988–1989.
Agrawal A, Bhake A, Cincu R . Giant lumbar paraspinal atypical teratoid/rhabdoid tumor in a child. J Cancer Res Ther 2009; 5: 318–320.
Yang CS, Jan YJ, Wang J, Shen CC, Chen CC, Chen M . Spinal atypical teratoid/rhabdoid tumor in a 7-year-old boy. Neuropathology 2007; 27: 139–144.
Yang M, Chen X, Wang N, Zhu K, Hu YZ, Zhao Y et al. Primary atypical teratoid/rhabdoid tumor of central nervous system in children: a clinicopathological analysis and review of literature in China. Int J Clin Exp Pathol 2014; 7: 2411–2420.
Tekautz TM, Fuller CE, Blaney S, Fouladi M, Broniscer A, Merchant TE et al. Atypical teratoid/rhabdoid tumors (ATRT): improved survival in children 3 years of age and older with radiation therapy and high-dose alkylator-based chemotherapy. J Clin Oncol 2005; 23: 1491–1499.
Biegel JA, Tan L, Zhang F, Wainwright L, Russo P, Rorke LB . Alterations of the hSNF5/INI1 gene in central nervous system: report on workshop. J Pediatr Hematol Oncol 2002; 24: 337–342.
Dufour C, Beaugrand A, Le Deley MC, Bourdeaut F, Andre N, Leblond P et al. Clinicopathologic prognostic factors in childhood atypical teratoid and rhabdoid tumor of the central nervous system: a multicenter study. Cancer 2012; 118: 3812–3821.
Benesch M, Bartelheim K, Fleischhack G, Gruhn B, Schlegel PG, Witt O et al. High-dose chemotherapy (HDCT) with auto-SCT in children with atypical teratoid/rhabdoid tumors (AT/RT): a report from the European Rhabdoid Registry (EU-RHAB). Bone Marrow Transplant 2014; 49: 370–375.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chao, M., Su, Yf., Jaw, TS. et al. Atypical teratoid/rhabdoid tumor of lumbar spine in a toddler child. Spinal Cord Ser Cases 3, 16026 (2017). https://doi.org/10.1038/scsandc.2016.26
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2016.26