Abstract
Study design:
International expert working group.
Objectives:
To revise the International Spinal Cord Injury (SCI) Bowel Function Basic Data Set as a standardized format for the collecting and reporting of a minimal amount of information on bowel function in clinical practice and research.
Setting:
Working group appointed by the American Spinal injury association (ASIA) and the International Spinal Cord Society (ISCoS).
Methods:
The draft prepared by the working group was reviewed by the International SCI Data Set Committee and later by members of the ISCoS Executive and Scientific Committees and the ASIA board. The revised data set was posted on the ASIA and ISCoS websites for 1 month to allow further comments and suggestions. Changes resulting from a Delphi process among experts in children with SCI were included. Members of ISCoS Executive and Scientific Committees and the ASIA board made a final review and approved the data set.
Results:
The International SCI Bowel Function Basic Data Set (Version 2.0) consists of the following 16 items: date of data collection, gastrointestinal and anal sphincter dysfunction unrelated to SCI, surgical procedures on the gastrointestinal tract, defecation method and bowel-care procedures, average time required for defecation, frequency of defecation, uneasiness, headache or perspiration during defecation, digital stimulation or evacuation of the anorectum, frequency of fecal incontinence, flatus incontinence, need to wear pad or plug, oral laxatives and prokinetics, anti-diarrheal agents, perianal problems, abdominal pain and discomfort and the neurogenic bowel dysfunction score.
Conclusion:
The International SCI Bowel Function Basic Data Set (Version 2.0) has been developed.
Similar content being viewed by others
Introduction
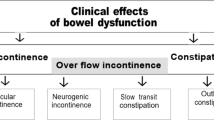
Spinal cord injury (SCI) has serious consequences for bowel function.1, 2, 3 The majority of individuals with SCI suffer from neurogenic bowel dysfunction (NBD) including constipation, fecal incontinence or abdominal pain. Thus, 42–95% of individuals with SCI report constipation,1, 2, 3, 4, 5 65% need digital stimulation or evacuation of the anorectum,2 25–41% need more than 30 min for bowel emptying,2, 5 75% have episodes of fecal incontinence,2 including 20–33% who are incontinent at least once per month2, 5 and 34–38% have chronic abdominal pain.5, 6 The severity of NBD depends on the completeness of SCI,2 and both prevalence and severity tend to increase with time after injury.6, 7
The International SCI Bowel Function Basic Data Set (Version 1.0) was constructed and published in 2009 as a standardized format for the collection and reporting of a minimal amount of information on bowel function in daily practice.8 After several comments were received by the authors and the ISCoS Data Set Committee, the data set underwent minor revision later the same year, however, without changing its basic structure. In line with the aim of the International SCI Data Sets,9 an International SCI Bowel Function Extended Data Set was developed to guide the collection of clinically relevant data in scientific studies on NBD.10 Today, the International SCI Bowel Function Basic Data Set has been used in several studies and it is included in databases around the world.
The inter-rater reliability of the International SCI Bowel Function Basic and Extended Data Sets was tested in an international setting in 2012.11 Most variables had acceptable reliability and only minor adjustments were recommended. A basic feature with the construction of the International SCI Bowel Function Data Sets was that by combining the basic and extended data sets, two commonly used scores for constipation and fecal incontinence could be computed.12, 13 The two scores have, however, not been validated among individuals with SCI. Furthermore, the option of computing them has not been used in international publications on individuals with SCI in the years following its publication.
The NBD score was developed in 2006 as a simple validated score to assess bowel dysfunction in adult individuals with SCI.14 The score includes 10 items that are associated with impaired quality of life caused by bowel symptoms. Each item is weighted according to the strength of its association with self-reported impaired quality of life. The NBD score has been used in several trials and other publications and it has been translated into at least nine languages. Most of the variables from the NBD score were already included in the International SCI Bowel Function Basic Data Set (Version 1.0 and 1.1). It is, however, impractical to have two very similar parallel tools for description of NBD. Thus, the current version of the data set allows easy computation and interpretation of the NBD score.
The International SCI Bowel Function Basic Data Set was developed for adults with SCI and it has not been tested specifically among children. There is, however, also a need for standardized collection and reporting of data on bowel function in children with SCI. It is proposed to use the present data set among children aged more than 3–4 years where bowel continence is expected. This has necissitated some clarifying comments to some variables in the syllabus for the data set. In general, when used with children, parents or primary caregivers are the primary sources for report until ~11 years of age. At the age 12–15, parent and child report in combination is proposed. The validity of the NBD score was tested in adults and neither the score nor its interpretation is directly applicable to children.
The aims of the present work were to revise the International SCI Bowel Function Basic Data Set (Version 1.1) based on experiences with its use since publication, to include the NBD score in the revised version, and to modify the syllabus for the data set in order to allow its use among children with SCI.
Materials and methods
The development of the International SCI Bowel Function Basic Data Set (Version 2.0) was very similar to the construction of its first version and to the development of other International SCI data sets.9 A working group was formed, including members appointed by the American Spinal Injury Association (ASIA) and the International Spinal Cord Society (ISCoS) and a representative from the International SCI Data Set Committee. A literature search was made on PubMed and Scopus to identify publications referring to the International SCI Bowel Function Basic Data Set and the NBD score. Practical experiences and results from the reliability study were also considered.11 The developmental process for the data set followed the steps below:
-
1)
The chairman of the working group (KK) wrote a draft for the data set and a syllabus both of which were circulated among the members of the group for comments. On the basis of their comments a second draft was made.
-
2)
The data set was reviewed by members of the International SCI Data Set Committee.
-
3)
Comments from the committee members were sent to the working group and relevant changes were made.
-
4)
Members of the ISCoS Executive and Scientific Committees and the ASIA board were invited to comment the data set.
-
5)
The working group prepared a response to comments from the Committees/Board members and further changes were made in the data set.
-
6)
Relevant societies, organizations and individuals with a potential interest were invited to comment, and the data set was posted on the ISCoS and ASIA websites for 1 month open to comments and suggestions.
-
7)
Minor adjustments were made after discussion in the working group.
-
8)
The results obtained from a Delphi process among experts in children SCI were included.
-
9)
Members of ISCoS Executive and Scientific Committees, and ASIA board received the data set for final review and approval.
-
10)
Endorsement by relevant international organizations and societies will be sought.
Results
The data set form is shown in the Appendix. The complete data sheet, data syllabus is available on the website of ISCoS (www.iscos.org.uk/international-sci-bowel-data-sets).
In the previous version of the data set, the time period listed for various symptoms varied. This is now 4 weeks for all.
Date of data collection
As the collection of data on bowel function may be carried out at any time since SCI, the date of data collection is imperative to compute time since injury and to identify the data collected in relation to other data collected on the same individual at various time points.
This variable is unchanged from the previous version of the data set.
Gastrointestinal or anal sphincter dysfunction unrelated to SCI
This relates to gastrointestinal or anal sphincter dysfunction concomitant and thus unrelated to changes in bowel function due to SCI. Functional gastrointestinal disorders, especially irritable bowel syndrome and idiopathic constipation, are very common in the general population. The prevalence depends on the exact definitions used but varies from 5% up to ~20%. The presence of functional or other gastrointestinal disorders before SCI may affect symptoms and treatment outcome.
Anal sphincter lesions due to childbirth are common and may contribute to fecal incontinence.15 Many types of gastrointestinal and anal sphincter dysfunction exist and it is therefore impractical to give an exact list of such conditions.
This variable is unchanged from the previous version of the data set.
Surgical procedures on the gastrointestinal tract
For the overall assessment of bowel function in individuals with SCI, information about surgical procedures on the gastrointestinal tract is important. This variable covers any surgical procedure on the gastrointestinal tract before or after SCI. It also includes perianal surgery. Because of the large number of possible surgical procedures, it is impractical to list more than the most important or common.
This variable is unchanged from the previous version of the data set.
Defecation method and bowel-care procedures
Individuals with SCI may use a combination of bowel emptying procedures. For practical purposes one should be defined as the main method. This is the method considered most important by the individual and the doctor or nurse. To be included in the data set, supplementary methods should be performed at least once every week.
More than one supplementary method can be used. The choice of defecation method and bowel-care procedures may change with time, and in the present data set they are given for the last 4 weeks. ‘Digital anorectal stimulation’ indicates use of a finger to trigger rectal contractions and anal relaxation, inducing rectal emptying. ‘Digital evacuation’, by contrast, is the need to dig out stools with a finger. Mini enema (or Clysma) contains 150 ml or less, and enema contain >150 ml. In individuals having a colostomy, this is always considered the main method for defecation. This variable is unchanged from the previous version of the data set. Not applicable is primary for children who are not of age for bowel continence.
Average time required for defecation
Time needed for defecation is clinically very important and strongly associated with impact on quality of life.2 The time given is from first transferring to the toilet or commode until end of defecation and transferal to wheel chair or moving from the toilet. If bladder emptying, body washing, shaving and so on is also performed while sitting at the toilet, time for this is subtracted as far as possible. For individuals performing bowel management while lying in the bed, time required is from beginning to end of bowel management, not including time for bladder management, body washing and so on. Time needed for defecation is the assessed average time for each defecation within the last 4 weeks. This variable does not distinguish between spontaneous or assisted defecation.
The number of possible answers within this variable has been reduced from seven to four. This is in accordance with the NBD score and makes the variable simpler to use.
Frequency of defecation
The frequency of defecation is very variable. However, in the general population more than 94% defecate between three times per day and three times per week.16 Among individuals with SCI, ~3% defecate less than once every week.2 Infrequent defecation is an indicator of insufficient bowel management and is associated with impact on quality of life.
The number of possible answers within this variable has been reduced from 10 to 5. This is in accordance with the NBD score and makes the item simpler to use.
Uneasiness, headache or perspiration during defecation
The feelings of general uneasiness and headache and the presence of perspiration during defecation is reported by ~25% of individuals with SCI.2, 5
The symptoms are mainly present in individuals with cervical or upper thoracic lesions and indicate that autonomic dysreflexia occurs during defecation. Digital anorectal stimulation, rectal evacuation or transanal irrigation may cause autonomic dysreflexia either with symptoms or as silent autonomic dysreflexia.17 For children, fussiness and irritability are common signs that autonomic dysreflexia may be present.18 This variable is new in the data set but part of the NBD score.
Digital stimulation or evacuation of the anorectum
Digital stimulation or evacuation is reported by approximately two-thirds of individuals with SCI.2 In some, it indicates poor emptying of the rectum, and the use of digitation is associated with impaired quality of life due to NBD.
The variable is part of the NBD score and now also included in the data set.
Frequency of fecal incontinence
Fecal incontinence is defined as involuntary passage of stools. It has profound influence on quality of life and may cause severe restriction on social activities. This variable does not distinguish between incontinence to solid or liquid stools but does exclude flatus incontinence. In individuals with ileo- or colostomy, leakage is considered as fecal incontinence. The number of possible answers within this variable has been reduced from eight to five. This is in accordance with the NBD score and makes the variable simpler to use. The variable is not applicable for children who are not of age for bowel continence.
Flatus incontinence
Flatus incontinence is defined as involuntary passage of gas. In individuals with ileo- or colostomy, leakage of gas from the stoma bag is considered as flatus incontinence. This variable is part of the NBD score and now also included in the data set.
Need to wear pad or plug
This variable describes the need to wear a pad because of fecal incontinence or combined fecal and urinary incontinence. The need to wear a pad only for urinary incontinence is not included. The need to wear a pad indicates insufficient bowel management. The use of anal plug is mainly relevant for individuals with conal or cauda equina lesions.
To make the variable easy to use, the number of possible answers has been reduced to Yes/No.
Oral laxatives and prokinetics
Oral laxatives are commonly used by individuals with SCI. A large number of oral laxatives exist either as liquids/drops or tablets/capsules/granulates and it is impractical to give a full list within the frames of this data set. Commonly used bulking or osmotic agents are lactulose, psyllium, magnesium and sorbitol.
Commonly used irritant laxatives are bisacodyl and sodium picosulphate.
Use of the prokinetic drug: prucalopride that was tested in a pilot study among individuals with SCI should be listed here.19 The guanylate cyclase-C receptor agonist Linaclotide and the chloride channel activator Lubiprostone have not yet been evaluated in individuals with SCI, but if used, they should also be listed here.
The variable has been slightly modified to include new drugs and it is also part of the NBD score. If both liquids/drops and tablets are used, the number of points given in the NBD score will be four.
Anti-diarrheal agents
Fiber supplement and constipating drugs are usually first-line therapy against fecal incontinence of non-neurogenic origin. The most commonly used drug is Loperamide.
In individuals with SCI this approach is, however, rarely used as it may aggravate constipation. The variable only covers drugs taken with the aim of prolonging intestinal transit and to prevent fecal incontinence. Thus, the use of drugs that have constipation as side effect, e.a. opioids or antocholinergics, is not included.
The variable has been simplified because medication affecting bowel function will usually be included in the (electronic) list of medication. This item is part of the NBD score.
Perianal problems
Due to straining and assisted defecation hemorrhoids, fissures and rectal prolapse are more common among individuals with SCI than in the general population. Anal soiling may contribute to perianal sores. In the present data set, perianal sores are located within the crena ani or the perineum and not on the buttocks or lower back.
For practical purposes, no distinction is made in the present data set between rectal mucosal prolapse and full-wall rectal prolapse. Perianal problems may change with time and only those present within the last 4 weeks should be noted.
This variable is unchanged from the previous version of the data set, and is partly included in the NBD score.
Abdominal pain and discomfort
Abdominal pain is commonly reported by individuals with SCI and to many it causes serious discomfort.6, 7 It may be a symptom of constipation.
This variable is new in the data set.
Total NBD score (optional)
The NBD score has been developed and validated for assessment of bowel dysfunction in individuals with SCI.14 It is computed by adding the points given in parenthesis after each relevant variable in the data set. Interpretation of the score is shown to make the combined use of the NBD score and the data set easier (Appendix).
Discussion
The data within the International SCI Bowel Function Basic Data Set (Version 2.0) will usually be used in conjunction with data included in the International SCI Core Data Set and sometimes with data from other data sets.20 A significant change from the earlier version of the data set is that it combines data needed for basic description of bowel function with those necessary to compute the NBD score. Thereby, a validated score for bowel dysfunction is directly available from the data set. This provides clinicians and researchers with a simple, validated and widely used tool for evaluation and monitoring of bowel function.
The option of computing the Cleveland constipation score and a fecal incontinence score from items within the combined International SCI Bowel Function Basic and Extended Data Sets has been abandoned.12, 13 The two scores are commonly used in able bodied, but they have not been validated in individuals with SCI. The authors considered including the Bristol stool scale in the data set, but decided not to do so because it has not been validated in individuals with SCI.21 Inclusion of the NBD score directly in the data set necessitated the inclusion of extra items, whereas others could be simplified and the time range for symptoms reported could be standardized to 4 weeks.
The international inter-rater reliability test of the International SCI Bowel Function Basic and Extended Data Sets identified problems with only few items.11 In the International SCI Bowel Function Basic Data Set, the reporting of ‘mini enema’ as a supplementary method within the item ‘Defecation method and bowel care procedures’ had a kappa value of 0.19 (poor) and the option ‘other’ within ‘Medication affecting bowel function/constipating agents’ had a kappa value of 0.15 (poor). For all remaining items in the present data set, the inter-rater reliability was fair, moderate, good or very good.11 The reporting of specific medication affecting bowel function is no longer part of the data set as it is considered part of patients’ medication files. The same holds true for assessment of voluntary anal sphincter function which is part of the international standards to document remaining autonomic function after SCI.22 Another problem identified with both the basic and extended data sets was that some raters choose more than one response where only one was allowed.11 We expect that this problem will be reduced because the number of possible answers has been reduced in several of the variables.
The inter-rater reliability study further revealed that most raters rarely used the instructions for use for the data sets as posted in the ISCoS website.11 This is probably quite understandable in busy clinical practice and underlines the importance of data set forms being as self-explanatory as possible.
Previous versions of the International SCI Bowel Function Basic and Extended Data Sets were developed for use in adult patients. Hence, there has been an unfulfilled need for an instrument to document neurogenic bowel symptoms in children. Data needed to develop such an instrument are not available, but based on expert opinion by a group of pediatricians with special experience within the field, it was decided to use the present version with a few extra explanatory remarks. Whether this is valid or not needs to be investigated in future studies. The NBD score was specifically developed and validated among adult patients with SCI and it is not directly applicable to children.
Most of the existing International SCI Data Sets are intended to be filled in by a health-care professional and not developed for direct use by individuals with SCI.
Development of patient-completed questionnaires as produced for the pain data set may further promote the use of the data sets.23 Such patient-reported outcome measures could be developed for electronical use and filled in by the patient through email or an application for their telephone.
Abdominal pain is common among subjects with SCI (6) but not included in the NBD score. It is often relevant to supplement the information from the NBD score with the subjective assessment of pain. Abdominal pain is sometimes, but not always, related to constipation (6).
The International SCI Bowel Function Basic Data Set has been used in several studies and it is included in databases around the world. Therefore, changing the data set will have practical consequences for several people. We do, however, find that experiences made during the 6 years since the publication of the International SCI Bowel Function Basic Data Set (Version 1.0) support the major revisions made in the present version. A measure of the success of these revisions will hopefully be reflexed in their increasing clinical and research use. Developing the data set is an ongoing process, and all interested parties are encouraged to contact members of the working group or the ISCoS International SCI Data Set Committee through the first or last authors of this article.
DATA ARCHIVING
There were no data to deposit.
References
Glickmann S, Kamm MA . Bowel dysfunction in spinal cord injury patients. Lancet 1996; 347: 1651–1653.
Krogh K, Nielsen J, Djurhuus JC, Mosdal C, Sabroe S, Laurberg S . Colorectal function in patients with spinal cord lesions. Dis Colon Rectum 1997; 40: 1233–1239.
Stone JM, Nino-Murcia M, Wolfe VA, Perkash I . Chronic gastrointestinal problems in spinal cord injury patients: a prospective analysis. Am J Gastroenterol 1990; 84: 1114–1119.
De Looze D, Van Laere M, De Muynck M, Beke R, Elewaut A . Constipation and other chronic gastrointestinal problems in spinal cord injury patients. Spinal Cord 1998; 36: 63–66.
Harari D, Sarkarati M, Gurwitz JH, McGlinchey-Berroth G, Minaker KL . Constipation-related symptoms and bowel program concerning individuals with spinal cord injury. Spinal Cord 1997; 35: 394–401.
Finnerup NB, Faaborg P, Krogh K, Jensen TS . Abdominal pain in long-term spinal cord injury. Spinal Cord 2008; 46: 198–203.
Faaborg PM, Christensen P, Finnerup N, Laurberg S, Krogh K . The pattern of colorectal dysfunction changes with time since spinal cord injury. Spinal Cord 2008; 46: 234–238.
Krogh K, Perkash I, Stiens SA, Biering-Sørensen F . International bowel function basic spinal cord injury data set. Spinal Cord 2009; 47: 230–234.
Biering-Sørensen F, Charlifue S, DeVivo M, Noonan V, Post M, Stripling T et al. International spinal cord injury data sets. Spinal Cord 2006; 44: 530–534.
Krogh K, Perkash I, Stiens SA, Biering-Sørensen F . International bowel function extended spinal cord injury data set. Spinal Cord 2009; 47: 235–241.
Juul T, Bazzocchi G, Coggrave M, Johannesen IL, Hansen RB, Thiyagarajan C et al. Reliability of the international spinal cord injury bowel function basic and extended data sets. Spinal Cord 2011; 49: 886–891.
Agachan F, Chen T, Pfeiffer J, Reisman P, Wexner SD . A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum 1996; 39: 681–685.
Vaizey CJ, Carapeti E, Cahill JA, Kamm MA . Prospective comparison of faecal incontinence grading systems. Gut 1999; 44: 77–80.
Krogh K, Christensen P, Sabroe S, Laurberg S . Neurogenic bowel dysfunction score. Spinal Cord 2006; 44: 625–631.
Hallock JL, Handa VL . The epidemiology of pelvic floor disorders and childbirth: an update. Obstet Gynecol Clin North Am 2016; 43: 1–13.
Drossman DA, Sandler RS, McKee DC, Lovitz AJ . Bowel patterns among subjects not seeking health care. Gastroenterology 1982; 83: 529–534.
Faaborg PM, Christensen P, Krassioukov A, Laurberg S, Frandsen E, Krogh K . Autonomic dysreflexia during bowel evacuation procedures and bladder filling in subjects with spinal cord injury. Spinal Cord 2014; 52: 494–498.
Hickey KJ, Vogel LC, Willis KM, Anderson CJ . Prevalence and etiology of AD in children with spinal cord injuries. J Spinal Cord Med 2004; 27: S54–S60.
Krogh K, Jensen MB, Gandrup P, Laurberg S, Nilsson J, Kerstens R et al. Efficacy and tolerability of Prucalopride in patients with constipation due to spinal cord injury. Scand J Gastroenterol 2002; 37: 431–436.
DeVivo M, Biering-Sørensen F, Charlifue S, Noonan V, Post M, Stipling T et al. International spinal cord injury core data set. Spinal Cord 2006; 44: 535–540.
Degen LP, Phillips SF . How well does stool for reflect colonic transit? Gut 1996; 39: 109–113.
Alexander MS, Biering-Sorensen F, Bodner D, Brackett NL, Cardenas D, Charlifue S et al. International standards to document remaining autonomic function after spinal cord injury. Spinal Cord 2009; 47: 36–43.
Jensen MP, Widerstrom-Noga E, Richards JS, Finnerup NB, Biering-Sørensen F, Cardenas DD . Reliability and validity of the International Spinal Cord Injury Basic Pain Data Set as self-report measures. Spinal Cord 2010; 48: 230–238.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix 1
Appendix 1

Rights and permissions
About this article
Cite this article
Krogh, K., Emmanuel, A., Perrouin-Verbe, B. et al. International spinal cord injury bowel function basic data set (Version 2.0). Spinal Cord 55, 692–698 (2017). https://doi.org/10.1038/sc.2016.189
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2016.189
This article is cited by
-
Impact of Neurogenic Lower Urinary Tract Dysfunction on Bowel Symptoms
Current Bladder Dysfunction Reports (2023)
-
Are micro enemas administered with a squeeze tube and a 5 cm-long nozzle as good or better than micro enemas administered with a 10 cm-long catheter attached to a syringe in people with a recent spinal cord injury? A non-inferiority, crossover randomised controlled trial
Spinal Cord (2022)
-
Guideline for the management of neurogenic bowel dysfunction in spinal cord injury/disease
Spinal Cord (2022)
-
What should be clarified when learning the International Standards to Document Remaining Autonomic Function after Spinal Cord Injury (ISAFSCI) among medical students
Spinal Cord Series and Cases (2021)
-
Development of a novel neurogenic bowel patient reported outcome measure: the Spinal Cord Injury Patient Reported Outcome Measure of Bowel Function & Evacuation (SCI-PROBE)
Spinal Cord (2020)