Abstract
Study design:
Within-participant randomised controlled trial.
Objectives:
To determine whether strength training combined with usual care increases strength in partially paralysed muscles of people with recent spinal cord injury (SCI) more than usual care alone.
Settings:
SCI units in Australia and India.
Methods:
Thirty people with recent SCI undergoing inpatient rehabilitation participated in this 12-week trial. One of the following muscle groups was selected as the target muscle group for each participant: the elbow flexors, elbow extensors, knee flexors or knee extensors. The target muscle on one side of the body was randomly allocated to the experimental group and the same muscle on the other side of the body was allocated to the control group. Strength training was administered to the experimental muscle but not to the control muscle. Participants were assessed at baseline and 12 weeks later. The primary outcome was maximal isometric muscle strength, and the secondary outcomes were spasticity, fatigue and participants’ perception of function and strength.
Results:
There were no dropouts, and participants received 98% of the training sessions. The mean (95% confidence interval (CI)) between-group difference for isometric strength was 4.3 Nm (1.9–6.8) with a clinically meaningful treatment effect of 2.7 Nm. The mean (95% CI) between-group difference for spasticity was 0.03/5 points (−0.25 to 0.32).
Conclusion:
Strength training increases strength in partially paralysed muscles of people with recent SCI, although it is not clear whether the size of the treatment effect is clinically meaningful. Strength training has no deleterious effects on spasticity.
Similar content being viewed by others
Introduction
Weakness secondary to partial paralysis is one of the most common impairments after spinal cord injury (SCI). Partial paralysis is caused by disruption to some but not all motor pathways. This type of weakness in the upper limbs can profoundly reduce hand function.1 Similarly, partial paralysis of the lower limb muscles prevents people from walking.2 The ability to walk and use the hands are both high priorities for people with SCI and important determinants of quality of life.3
Many different interventions are used and advocated to increase strength.4 However, the most common type of strength training is progressive resistance training. This involves maximally contracting muscles against high levels of resistance. Typically, this is done in sets of 10 contractions. The sets are repeated three times in one training session, and training is performed three times a week for at least 12 weeks (that is, 90 maximal contractions per week).5 The basis for the belief that progressive resistance training is effective comes largely from trials involving people without paralysis.6, 7 However, it cannot be assumed that what is effective for muscles of able-bodied individuals is also effective for the partially paralysed muscles of a person with SCI.
There are currently only three clinical trials that have examined the effectiveness of any type of strength training in the partially paralysed muscles of people with SCI.8, 9, 10 The first randomised controlled trial involving the wrist muscles of people with SCI failed to find a clear therapeutic effect of progressive resistance training. However, many participants had strength of less than grade 3/5. It was hypothesised that progressive resistance training may not be effective in these very weak participants due to insufficient neural drive to stimulate muscle fibre hypertrophy.9 In those very weak people, repetitive practice with low resistance may be more important because increases in strength may be largely secondary to neural adaptations.11 A second clinical trial examined the effectiveness of progressive resistance training and electrical stimulation in muscles that were stronger and larger than those examined in the first trial.8 The results indicated a treatment effect, although the 95% confidence interval (CI) associated with the mean between-group difference was wide and failed to rule in or out the possibility of either a very small or very large treatment effect. In addition, the use of electrical stimulation made it difficult to determine whether the electrical stimulation, the progressive resistance training or both, were the important aspects of the training programme. More recently a small crossover trial of five participants compared isometric strength training with concentric strength training in the lower limbs of people with incomplete SCI.10 Interestingly, the between-group difference indicates that isometric strength training is superior to concentric strength training. These results need to be replicated in a larger trial but nonetheless suggest that the type of muscle contraction used in strength training may be important.
Although there are three trials examining the effectiveness of strength training, there is still considerable uncertainty about the responsiveness of partially paralysed muscles to any type of strength training programme. The aim therefore of this trial was to determine the effects of a 12-week strength training programme on maximal voluntary isometric muscle strength. The secondary aims were to determine the effects of the training on spasticity, muscle fatigue and participants’ perceptions of strength and function. We restricted our study to muscles with grade 3/5 or 4/5 strength and included both isometric and concentric strength training because the tentative evidence to date supports the combination of this type of training in stronger muscles.10
Methods
An assessor-blinded randomised within-participant controlled trial was conducted in five SCI units—four SCI units in Australia and one SCI unit in India. The first and last participants were randomised in September 2014 and November 2015, respectively. The start of recruitment at the five SCI units was staggered with the last SCI unit commencing recruitment in August 2015. One target muscle group was selected for each participant from the following groups of muscles: elbow flexors, elbow extensors, knee flexors or knee extensors but only if the corresponding contralateral muscle group had similar strength. If more than one muscle group was suitable for inclusion, then the stronger muscle was chosen although the clinicians had some freedom to select a muscle based on their clinical judgement and the practicalities of implementing the trial protocol. Participants received a strength programme for the target muscle group on one side of the body only (experimental side). The side receiving strength training was determined by random allocation.
The trial was registered with the Australian New Zealand Clinical Trials Registry (ACTRN12614000914662). All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed. The study was approved through all appropriate ethics committees.
Participants
Thirty in-patients with recent SCI were recruited (see Table 1 for the inclusion and exclusion criteria). A computer-generated blocked random allocation schedule was compiled before commencement by a person not involved in the recruitment of participants. Each participant was randomly allocated to train the target muscle in their left or right limb. Participants’ allocations were placed in opaque, sequentially numbered and sealed envelopes, which were held off site by an independent person. Once a participant passed the screening process and completed the initial assessments, an envelope was opened and allocation revealed. The participant was considered to have entered the trial at this point.
Intervention
The target muscle group in the experimental limb was trained three times a week for 12 weeks following the key principles of progressive resistance training.12 Participants performed 40 maximal contractions in four sets of 10 and were provided with verbal encouragement throughout. The first two sets of 10 maximal contractions were isometric contractions (4 s duration with a 4 s rest interval) and the second two sets of 10 were concentric contractions with a 2 min rest after each set of 10 contractions. Resistance was applied through the hands of the therapists to ensure the muscle contractions required maximal effort from the participants. All therapists received training in how to correctly hold the limb while providing resistance to ensure consistency. Therapists tried to ensure that the resistance they applied exhausted participants by the end of each set of 10 contractions.13 If participants’ strength increased and the therapists were unable to provide sufficient resistance, then weights were applied to the participants’ limb in addition to the resistance applied through the therapists’ hands.
All participants continued to receive usual care that involved comprehensive rehabilitation. This involved gait and functional training for activities of daily living as considered necessary by their treating therapists (for example, training to transfer, walk, roll and push a manual wheelchair). Participants received other forms of therapy deemed appropriate for managing fitness, respiratory compromise, contractures, spasticity or pain. In addition, participants were able to receive any type of strength training programme deemed appropriate by their treating therapists to other muscles groups on both sides of the body with the exception of the target muscle group. The treating therapists responsible for providing usual care were blinded to whether the left or right side of the target muscle group was receiving the strength training intervention. This was possible because the therapist providing the usual care did not also provide the strength training.
Assessment
Participants were measured by a blinded assessor once before randomisation and once 12 weeks after randomisation (with a 1-week window). The success of blinding was recorded. The primary outcome was maximal voluntary isometric strength. The secondary outcomes were spasticity, muscle fatigue and participants’ perceptions of strength and function.
The details of the outcome measures are as follows.
Maximal voluntary isometric strength
A dynamometer (Lafayette Instrument Company, Lafayette, IN, USA) was used to measure peak isometric muscle strength at the target muscle’s mid length (for example, 90° elbow flexion for the elbow flexor muscle group).14 The dynamometer was cradled in a custom-made rigid jig that allowed the participant to push or pull against a fixed interface. There were two jigs specifically designed for this study—one for the upper limb and one for the lower limb (see Figure 1). Strength was recorded in pounds and converted into Nm (using the perpendicular distance from the joint axis to the centre of the force transducer). The perpendicular distance was recorded for each measure and was kept as consistent as possible for each attempt. Participants were required to perform six maximal isometric muscle contractions and were provided with verbal encouragement throughout. There was a 60 s rest between each trial. The left limb was always measured before the right limb. A between-group difference equivalent to 15% of mean initial strength was set as clinically meaningful before the commencement of the study.
Spasticity
Spasticity was included as a secondary outcome measure because some argue that strength training has deleterious effects on spasticity.15 The quality score of the Ashworth Scale was used to measure spasticity in the participants’ target muscle group. Specifically, the quality of resistance felt when the limb was moved was recorded on a five-point scale where 0 reflected ‘no increase in tone’ and 4 reflected ‘limb rigid in flexion or extension’. It was decided before the commencement of the study that a between-group difference of one point would be considered indicative of a detrimental effect of strength training on spasticity.
Muscle fatigue
Muscle fatigue was measured using the dynamometer and jig as outlined above; however, participants were required to perform repeated maximal isometric contractions of 4 s duration over 3 min with a 4 s rest between each contraction. The mean torque generated over the last three contractions was divided by the mean torque generated over the first three contractions to calculate the fatigue index.16 A between-group difference equivalent to 15% of the mean initial fatigue index was considered clinically meaningful.
Participants’ perceptions of strength
At the completion of the trial, participants were asked to rate separately their impressions of change in strength in their right and left target muscle group on a 15-point scale where −7 indicated ‘a very great deal worse’, 0 indicated ‘no change’ and +7 indicated ‘a very great deal better’.17 A between-group difference of one point was considered clinically meaningful.
Participants’ perceptions of function
At the completion of the trial, participants were asked to rate separately their impressions of change in their ability to use their right and left limb for functional activities on a 15-point scale where −7 indicated ‘a very great deal worse’, 0 indicated ‘no change’ and +7 indicated ‘a very great deal better’.17 A between-group difference of 1 point was considered clinically meaningful.
In addition, participants were asked to rate the inconvenience of the training programme. They rated the inconvenience on a 10-point scale, where 1 indicated the training was ‘extremely inconvenient’ and 10 indicated that the training was ‘not at all inconvenient’.
Statistical analysis
STATA v13 (Stata-corp, College station, TX, USA) was used for all analyses using intention-to-treat. The t-distribution was used to estimate mean between-group differences and associated 95% CI from the change data (that is, post intervention minus pre-intervention) or post-intervention data for outcomes without a baseline measure. To test the robustness of the assumptions about the normality of the distribution of the data, all analyses were repeated using the STATA ‘cendif’ routine and bootstrapping techniques. The ‘cendif’ routine is based on the generalised Hodges-Lehmann median differences function and makes no assumptions about the normality of distributions.18 The results from the additional analyses were almost identical and are not reported here.
Results
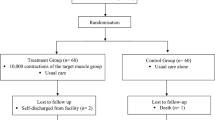
The flow of participants through the trial is shown in Figure 2. No participant withdrew from the study. The median (interquartile range, IQR) age and time since injury were 46 years (25–65) and 2 months (1.4–3.1), respectively. Participants had American Spinal Injury Association Impairment Scale (AIS) A (n=8), AIS B (n=1), AIS C (n=11) or AIS D (n=10) lesions with neurological levels ranging from C1 to L3 and motor levels ranging from C1 to L3 as defined by the International Standards for Neurological Classification of SCI (see Table 2). The groups were similar at baseline for most key prognostic factors.
The protocol dictated that participants perform the progressive resistance strength training three times a week for 12 weeks with a total of 36 training sessions. This was largely achieved with a median (IQR) total number of 36 (35–36) training sessions provided over 12 weeks (equivalent to 98%). Training sessions were missed on public holidays or if participants were unwell. As far as possible, additional sessions were provided to make up for missed sessions. All assessors remained blinded for the 12-week outcome measure.
The mean (95% CI) between-group difference for maximal voluntary isometric strength was 4.3 Nm (95% CI, 1.9–6.8) but the 95% CI spanned the clinically meaningful treatment effect of 2.7 Nm, indicating that while strength training increased strength there is uncertainty about whether the size of the treatment effect is clinically meaningful. The mean (95%CI) between-group differences for perceived change in strength and function were 2.2 points (1.3–3.0) and 2.1 points (1.2–3.0), respectively, indicating that participants perceived clinically meaningful increases in strength and function. The mean (95% CI) between-group difference for spasticity was 0.03 points (−0.25 to 0.32), with the upper end of the 95% CI less than one point. This indicates that the strength training did not have deleterious effects on spasticity. The effects of strength training on fatigue were unclear with the 95% CI associated with the mean between-group difference spanning the clinically meaningful treatment effect (see Table 3).
The median (IQR) perception of inconvenience of the strength training was 9/10 (9–10), where a score of 10 indicates ‘not at all inconvenient’. There were no serious adverse events although one participant experienced quadriceps tightening and discomfort throughout his last week of training with the concentric contractions. This was resolved with applying less resistance and dissipated once the exercises were ceased.
Discussion
This study indicates that strength training increases strength in the partially paralysed muscles of people with SCI. These results are important because weakness is a major problem for people with SCI and very little research attention has been directed at determining the effectiveness of different strength training paradigms. However, it is not clear from our results whether the increases in strength are clinically meaningful because the 95% CI associated with the mean between-group difference spans our pre-determined clinically meaningful treatment effect. We set the clinically meaningful treatment effect at 15% of mean initial values. This was somewhat arbitrary but even if we had set it to a lower value, the interpretation of our results remains the same unless people consider a treatment effect as low as 1.9 Nm as potentially worthwhile. Interestingly, participants perceived that the intervention improved strength and function with the lower ends of the 95% CIs associated with the mean between-group differences above our pre-defined clinically meaningful treatment effects of 1 point. However, participants were not blinded so their perceptions may in part reflect preconceived ideas about the benefits of strength training.
The results of this study align with a similar study we conducted in people with grade 3/5 or 4/5 strength of the quadriceps muscles although in our earlier study we added electrical stimulation to our strength training programme.8 The main difference in results between the two studies is the precision of the treatment effect (reflected by the width of the 95% confidence interval associated with the mean between-group difference). The 95% confidence interval in this study (95% CI, 1.9–6.8 Nm) indicates more precision than in our earlier study (95% CI, 1–27 Nm). The tighter precision may reflect the larger sample size, the weaker participants or the within-group study design. Although a within-group study design generally increases the precision of treatment estimates, it can also decrease treatment effects if training one limb has a carryover effect onto the untrained limb.19 A larger trial using a between-group design would offer the best solution to both issues.
We included a measure of fatigue because we were interested in determining whether strength training reduces fatigue. However, our results were inconclusive failing to rule in or out a treatment effect on this outcome. A larger sample is required to provide a clear answer to this question. These results align with the results of our previous studies, which have all failed to demonstrate a clear treatment effect of any type of strength training on fatigue.8, 9 These results may reflect a problem with the way we measure fatigue. For example, fatigue may be better measured with repeated contractions over more than 3 min. Alternatively, our results may indicate that our strength training programmes do not reduce fatigue. We know from able-bodied literature that the optimal training programme for reducing fatigue involves more emphasis on repeated contractions and less emphasis on resistance.20 We may therefore need to incorporate these training principles to reduce fatigue. However, we need to be open to the possibility that partially paralysed muscles do not respond in the same way to training as the non-paralysed muscles of able-bodied people and that it may be very difficult to reduce fatigue with any type of training.
The results of this study indicate no deleterious effects of strength training on spasticity. The 95% CI associated with the mean between-group difference indicates that these results cannot be dismissed on the basis of the sample size. There is now mounting evidence both from our own previous trials8, 9 and from trials in people with other types of neurological conditions21, 22 to quash any remaining concerns that strength training increases spasticity.
In our study, the therapists used their hands to provide the resistance. The training was provided in this way to ensure the muscle contractions required maximal effort from the participants. The therapists also provided verbal encouragement throughout the 10 contractions to motivate the participants to maximally contract their muscles. The downside of this method of strength training is that it is difficult to quantify the resistance provided by therapists. However, our results indicate that despite this disadvantage, participants got stronger. Perhaps if the training was provided in other ways or with commercially available gym equipment then the treatment effects may have been even more convincing. The use of equipment decreases reliance on therapists and therefore is less costly. However, in our experience it is difficult to get the fine graduation in resistance required to ensure patients with neurologically induced weakness are maximally contracting throughout the 10 contractions. Future studies could further explore this issue.
One limitation of our study is that we only measured isometric strength even though our training involved isometric and concentric contractions. It would have been interesting to also measure strength during concentric contractions. We explored ways of doing this but it was not easy in the clinical setting, and it may not be necessary to measure both types of strength because they are strongly correlated.23, 24 It is somewhat surprising that a recent study indicated that strength training using isometric contractions was superior to strength training using concentric contractions, and indicated no within-group changes in strength of those who only performed concentric contractions.10 The study was only small and needs verifying in a larger trial but nonetheless highlights how little is known about optimal strength training paradigms.
In conclusion, physiotherapists have administered strength training to non-paralysed muscles for a long time and have assumed that this intervention is equally applicable to partially paralysed muscles, but these assumptions have not been adequately tested. The results of this study provide some of the first evidence to indicate that partially paralysed muscles are responsive to strength training. The results are not generalisable to grade 1 or 2 muscles and still indicate some uncertainty about whether the size of the treatment effect is clinically meaningful.
Data Archiving
There were no data to deposit.
References
Snoek GJ, Ijzerman MJ, Hermens HJ, Maxwell D, Biering-Sorensen F . Survey of the needs of patients with spinal cord injury: impact and priority for improvement in hand function in tetraplegics. Spinal Cord 2004; 42: 526–532.
Manns PJ, Chad KE . Components of quality of life for persons with a quadriplegic and paraplegic spinal cord injury. Qual Health Res 2001; 11: 795–811.
Collinger JL, Boninger ML, Bruns TM, Curley K, Wang W, Weber DJ . Functional priorities, assistive technology, and brain-computer interfaces after spinal cord injury. J Rehabil Res Dev 2013; 50: 145–160.
Harvey LA . Physiotherapy rehabilitation for people with spinal cord injuries. J Physiother 2016; 62: 4–11.
Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc 2011; 43: 1334–1359.
Mulroy SJ, Thompson L, Kemp B, Hatchett PP, Newsam CJ, Lupold DG et al. Strengthening and optimal movements for painful shoulders (STOMPS) in chronic spinal cord injury: a randomized controlled trial. Phys Ther 2011; 91: 305–324.
Taylor NF, Dodd KJ, Damiano DL . Progressive resistance exercise in physical therapy: a summary of systematic reviews. Phys Ther 2005; 85: 1208–1223.
Harvey LA, Fornusek C, Bowden JL, Pontifex N, Glinsky J, Middleton JW et al. Electrical stimulation plus progressive resistance training for leg strength in spinal cord injury: a randomized controlled trial. Spinal Cord 2010; 48: 570–575.
Glinsky J, Harvey L, Korten M, Drury C, Chee S, Gandevia SC . Short-term progressive resistance exercise may not be effective at increasing wrist strength in people with tetraplegia: a randomised controlled trial. J Physiother 2008; 54: 103–108.
Jayaraman A, Thompson CK, Rymer WZ, Hornby TG . Short-term maximal-intensity resistance training increases volitional function and strength in chronic incomplete spinal cord injury: a pilot study. J Neurol Phys Ther 2013; 37: 112–117.
Folland JP, Williams AG . The adaptations to strength training: morphological and neurological contributions to increased strength. Sports Med 2007; 37: 145–168.
Ginis KA, Hicks AL, Latimer AE, Warburton DE, Bourne C, Ditor DS et al. The development of evidence-informed physical activity guidelines for adults with spinal cord injury. Spinal Cord 2011; 49: 1088–1096.
Kraemer WJ, Ratamess NA . Fundamentals of resistance training: progression and exercise prescription. Med Sci Sports Exerc 2004; 36: 674–688.
Sisto SA, Dyson-Hudson T . Dynamometry testing in spinal cord injury. J Rehabil Res Dev 2007; 44: 123–136.
Sharp SA, Brouwer BJ . Isokinetic strength training of the hemiparetic knee: effects on function and spasticity. Arch Phys Med Rehabil 1997; 78: 1231–1236.
Hartkopp A, Harridge SDR, Mizuno M, Ratkevicius A, Quistorff B, Kjaeer M et al. Effect of training on contractile and metabolic properties of wrist extensors in spinal cord-injured individuals. Muscle Nerve 2003; 27: 72–80.
Barrett B, Brown D, Mundt M, Brown R . Sufficiently important difference: expanding the framework of clinical significance. Med Decis Making 2005; 25: 250–261.
Newson R . Parameters behind ‘nonparametric’ statistics: Kendall's tau, Somer's D and median differences. Stata J 2002; 2: 45–64.
Lee M, Carroll TJ . Cross education: possible mechanisms for the contralateral effects of unilateral resistance training. Sports Med 2007; 37: 1–14.
Campos GE, Luecke TJ, Wendeln HK, Toma K, Hagerman FC, Murray TF et al. Muscular adaptations in response to three different resistance-training regimens: specificity of repetition maximum training zones. Eur J Appl Physiol 2002; 88: 50–60.
Smania N, Picelli A, Munari D, Geroin C, Ianes P, Waldner A et al. Rehabilitation procedures in the management of spasticity. Eur J Phys Rehabil Med 2010; 46: 423–438.
Morris SL, Dodd KJ, Morris ME . Outcomes of progressive resistance strength training following stroke: a systematic review. Clin Rehabil 2004; 18: 27–39.
Mandalidis D, O'Brien M . Relationship between hand-grip isometric strength and isokinetic moment data of the shoulder stabilisers. J Bodywork Mov Ther 2010; 14: 19–26.
Lord JP, Aitkens SG, McCrory MA, Bernauer EM . Isometric and isokinetic measurement of hamstring and quadriceps strength. Arch Phys Med Rehabil 1992; 73: 324–330.
Acknowledgements
We thank all our participants and staff from the SCI units in Australia and India who contributed to the trial. We thank the workshop staff at Neuroscience Research Australia who designed and constructed the rig used for our strength measurements. Simon Gandevia is supported by the National Health and Medical Research Council of Australia. Prince of Wales Hospital Foundation and National Health and Medical Research Council of Australia sponsored this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bye, E., Harvey, L., Gambhir, A. et al. Strength training for partially paralysed muscles in people with recent spinal cord injury: a within-participant randomised controlled trial. Spinal Cord 55, 460–465 (2017). https://doi.org/10.1038/sc.2016.162
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2016.162
This article is cited by
-
Robotic technology (ROBERT®) to enhance muscle strength in the hip flexor muscles following spinal cord injury: a feasibility study
Spinal Cord Series and Cases (2024)
-
Using the benefit-harm trade-off method to determine the smallest worthwhile effect of intensive motor training on strength for people with spinal cord injury
Spinal Cord (2024)
-
Effects of high-intensity and progressive volume resistance training on functional, mental states, and quality of life of people with spinal cord injury
Sport Sciences for Health (2024)
-
Early and intensive Motor Training for people with spinal cord injuries (the SCI-MT Trial): description of the intervention
Spinal Cord (2023)
-
Exoskeleton-assisted walking improves pulmonary function and walking parameters among individuals with spinal cord injury: a randomized controlled pilot study
Journal of NeuroEngineering and Rehabilitation (2021)