Abstract
Study design:
Survey.
Objectives:
To determine whether upper extremity reconstruction in patients with tetraplegia is underutilized internationally and, if so, what are the barriers to care.
Setting:
International—attendees of a meeting in Paris, France.
Methods:
One hundred and seventy attendees at the Tetrahand meeting in Paris in 2010 were sent a 13-question survey to determine the access and utilization of upper limb reconstruction in tetraplegic patients in their practice.
Results:
Respondents ranged the globe including North America, South America, Europe, Asia and Australia. Fifty-nine percent of respondents had been practicing for more than 10 years. Sixty-four percent of respondents felt that at least 25% of people with tetraplegia would be candidates for surgery. Yet the majority of respondents found that <15% of potential patients underwent upper extremity reconstruction. Throughout the world direct patient referral was the main avenue of surgeons meeting patients with peer networking a distant second. Designated as the top three barriers to this care were lack of knowledge of surgical options by patients, lack of desire for surgery and poor referral patterns to appropriate upper extremity surgeons.
Conclusion:
The results of this survey, of a worldwide audience, indicate that many of the same barriers to care exist regardless of the patient’s address. This was a preliminary opinion survey and thus the results are subjective. However, these results provide a roadmap to improving access to care by improving patient education and interdisciplinary physician communication.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) profoundly alters a person’s life. After injury, a priority for people with tetraplegia is to increase their independence.1, 2, 3 A key component to degree of independence for these people is how much residual upper extremity function remains.4, 5 Multiple procedures exist to improve the upper extremity function of those with tetraplegia including procedures to restore elbow extension, wrist extension and grasp. Jaspers Focks-Feenstra et al.6 demonstrated long-term patient satisfaction after upper extremity surgery for patients with tetraplegia. Wangdell studied satisfaction and performance after grip reconstruction in patients with tetraplegia.7 Patients reported 38% of tasks (that is, writing, sewing, buttoning) as impossible to perform before surgery. After surgery, patients were able to perform 78% of these tasks and rated 11% as ‘able to do extremely well’. Despite these favorable results, in the United States these procedures are underutilized with only 14% of appropriate candidates receiving upper extremity reconstruction.8
There are likely many reasons for this underutilization including patient factors such as not wanting the increased dependence for the rehabilitation after surgery, waiting for a cure and lack of knowledge. Other barriers to care are at the physician level. A survey of physiatrists and surgeons found that referring physicians had concerns about the efficacy and safety of surgery.9 A second study demonstrated that many patients were simply uninformed about this option and those who did know had a negative impression of the available surgeries.10 Anderson et al.11 found a similar lack of knowledge about upper extremity reconstruction options among patients with tetraplegia.
The work on utilization of upper extremity in tetraplegia has been focused upon in the United States. The physician barriers seemed to be an important contributor but the US also has a unique health care system, which may present other barriers to care (lack of health insurance, low reimbursement, and so on). If the barrier is at the physician or patient level, then this underutilization may be an international phenomenon. This study hypothesized that the same barriers to care for this population exist internationally regardless of health system of structure. This survey’s goal was to gain a worldwide perspective on the utilization of upper extremity reconstruction, barriers to care and ways to improve access.
Materials and methods
Participants
The survey was sent to 170 attendees at an international upper extremity tetraplegia course in Paris in 2010. The attendees included surgeons, physiatrists, therapists and neurologists. This meeting was geared to practitioners actively caring for the upper limbs of SCI patients.
Survey
This was a 13-question survey sent via electronic mail (Figure 1). The questions were designed to address perceptions of the access and utilization of upper limb reconstruction in patients with tetraplegia. The study was approved by the Institutional Review Board. The need for formal consent was waived as completion of the survey was implied consent. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Analysis
Responses for multiple-choice questions were counted and divided by the total number of responses received to determine percentages. Answers to open-ended questions were reviewed by two independent reviewers for clarity. Free responses were grouped for analysis when similar words or phrases were identified within a response. For example, ‘educate physiatrists’, ‘improve awareness of PTs and OTs’ and ‘educate doctors and therapists who take care of the acute injury’ were all grouped together as educate referring practitioners. The analysis was simple descriptive statistics and percentages were used to present the data.
Results
Fifty-two of 170 surveys were completed for a 30% response rate. Respondents ranged the globe including North America, South America, Europe, Asia and Australia. The distribution of represented countries is shown in Table 1. Fifty-two percent of responses were from surgeons, whereas 21% and 15% were from therapists and physiatrists, respectively. Fifty-nine percent of respondents had been practicing for more than 10 years with over 17% having more than 20 years of experience. Seventy-one percent of respondents worked in a spinal cord or rehabilitation center. Direct referral and patient networking were the two most common routes by which patients found providers for care.
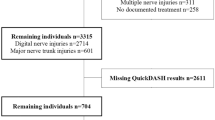
The responses indicated a disconnect between patient candidacy for upper extremity reconstruction and actual receipt of the surgery. Sixty-four percent of respondents felt that at least 25% of people with tetraplegia would be candidates for surgery. Yet the majority of respondents found that <15% of potential patients underwent upper extremity reconstruction (Figure 2).
The top three barriers to upper limb surgery were felt to be lack of knowledge of surgical options by patients (ranked in the top 3 by 80% of respondents), lack of desire for surgery (90%) and poor referral patterns to appropriate upper extremity surgeons (74%). Other possible choices (lack of willing surgeons, financial concerns or other) ranked in the top 3 for <21% of respondents. Over 40 participants responded to the open-ended questions. When asked ways to improve access for upper limb surgery, most respondents indicated that improved communication and education between rehabilitation physicians and surgeons would be most effective. Example responses include ‘good cooperation between hand surgeon and physiatrist on spinal cord team’ and ‘relationship between spinal physicians/consultants and hand surgeons to ensure quality care’. In addition, better patient education regarding available options (‘good patient education’ and ‘information to patients at the first rehab period’) and early referral to hand surgeons (‘Early hand surgery clinic pre-assessment prior to discharge following 1st post-acute rehab’) were noted as ways to improve these patients’ access to upper limb surgery. Although multiple respondents felt that Internet information and patient networking both in person and electronically were important ways to improve patient education about available reconstructive options, physician visits were also deemed critical as each patient would need a customized reconstruction plan.
Discussion
Barriers to care exist in all specialties and many patient populations. This study suggests that underutilization of surgical rehabilitation of the upper limb for people with tetraplegia is an international phenomena. This sense that optimal patients are not receiving care persists even in countries that have minimized the cost barrier with centralized health care. For example, one of our survey respondents stated that problems with cost did not exist in their country and ‘all patients that want (an) operation will have that possibility.’ However, other barriers seem to exist regardless of the patient’s country and its payment system. These barriers include lack of patient education and weak interdisciplinary connections between specialties who care for these complex patients. These data suggest that improving utilization of this care may not require restructuring of a nation’s health care system but instead requires improving communication at the patient and provider level.
The patient level barriers can span from lack of knowledge to physical barriers, such as no handicap parking. Many respondents in this study identified lack of patient education as a common barrier (that is, patients were unaware of the treatment). Matter et al.12 surveyed SCI patients to determine their preferred route and source of information regarding health care. Patients preferred if the sources of information were a SCI expert/rehabilitation specialist, information via the Internet or in person. To improve SCI patient education on treatment options for the upper limb, the first step is awareness that procedure exists, but they must also understand the risks and potential benefits. This information needs to be conveyed in clear language and written education should consider patient’s literacy levels.13, 14 Other teaching avenues, such as patients educating patients could supplement face-to-face interactions with physicians and written material.
Multiple respondents to our survey indicated that a mandatory referral to an upper extremity reconstruction specialist after a SCI would improve access. There are clinical practice guidelines for care of the SCI upper limb, such as the Paralyzed Veterans of America guidelines. Inclusion of a recommendation for the newly injured patient to consult with a hand surgeon may be one area to improve utilization of care.15 Although this may be straightforward in some health care systems where specialists and primary care providers are tightly linked, other systems may need to build and bolster the relationships between specialists and primary care providers function.
Sweden has a coordinated system of SCI care and respondents from Sweden reported no barriers to care for patients desiring upper extremity reconstruction. In Stockholm, Sweden, there is an established SCI care program consisting of one hospital-based Spinal Injury Unit, two inpatient rehabilitation centers and one outpatient clinic for lifelong follow-up. In a series of recent articles Divanoglou et al.16, 17, 18, 19 have compared outcomes after traumatic SCI in Sweden to the more fragmented system in Greece. The Swedish group noted improved survival, decreased length of stay and earlier surgical intervention with fewer readmissions compared with the Greek group. This series highlights some of the benefits that can be obtained from coordinated SCI care.
Another barrier noted by our respondents was a lack of understanding of the procedures by the nonsurgical referring physicians. Some US SCI physicians reported there was ‘no benefit’ or surgery was ‘hard to justify’ and this international survey found referral barriers also exist outside the US.9, 20 It is within our means to improve education and communication between surgeons and physiatrists and physical therapists who work closely with the tetraplegic population. One possible route would be to add an educational requirement for those residents specializing in SCI on upper extremity surgery and its outcomes. Curtin et al.9 demonstrated that physiatrists exposed to upper extremity reconstruction during residency were significantly more likely to believe that the risk of surgery were worth the benefits when compared with their colleagues who lacked this early exposure. Publishing in the literature of other specialties who work with people with tetraplegia is important for imparting research between groups. Multispecialty conferences focusing on the coordinated care of SCI patients are another way to share knowledge.
The results of our survey suggest a link between each of the barriers to care. Perhaps breaking through one will create a domino effect and clear the path towards improved utilization of upper extremity reconstruction. On the basis of this survey, we know the primary way patients with tetraplegia access care is through the direct referral from another provider. Multiple physicians and therapists do not know of the options for upper extremity reconstruction and, if they do, many are unaware of their positive long-term outcomes. These providers are, therefore, unlikely to refer their patients to a specialist for evaluation. Patients are also unaware of the options available to them and the significant impact that surgical reconstruction could have on their life. Improving knowledge is central to improving access to this care.
Several weaknesses are present in this study. As a survey-based study, it is dependent on respondents for the data. With a response rate of only 30%, we likely experienced selection bias in the respondents. Those that feel passionate (either positively or negatively) about a topic may be the most likely to respond. In addition, we solicited respondents’ thoughts as part of their answers, which creates a level of subjectivity in the responses. This open-ended questioning provides information to help direct future more-refined interventions.
We may not be able to increase the number of reconstructive hand surgeons or change cost barriers internationally, but we can advance care by improving education and communication between health care providers, therapists and patients around the world. The subjective nature of this survey provides a starting point; an objective study of referral patterns in areas deemed to have both effective and ineffective surgeon/physiatrist relationships would help better highlight the challenges we need to overcome.
Data Archiving
There were no data to deposit.
References
Simpson LA, Eng JJ, Hsieh JT, Wolfe DL . The health and life priorities of individuals with spinal cord injury: a systematic review. J Neurotrauma 2012; 29: 1548–1555.
Putzke JD, Richards JS, Hicken BL, DeVivo MJ . Predictors of life satisfaction: a spinal cord injury cohort study. Arch Phys Med Rehabil 2002; 83: 555–561.
van Leeuwen CM, Post MW, Hoekstra T, van der Woude LH, de Groot S, Snoek GJ et al. Trajectories in the course of life satisfaction after spinal cord injury: identification and predictors. Arch Phys Med Rehabil 2011; 92: 207–213.
Snoek GJ, IJzerman MJ, Hermens HJ, Maxwell D, Biering-Sorensen F . Survey of the needs of patients with spinal cord injury: impact and priority for improvement in hand function in tetraplegics. Spinal Cord 2004; 42: 526–532.
Anderson KD . Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma 2004; 21: 1371–1383.
Jaspers Focks-Feenstra JH, Snoek GJ, Bongers-Janssen HM, Nene AV . Long-term patient satisfaction after reconstructive upper extremity surgery to improve arm-hand function in tetraplegia. Spinal Cord 2011; 49: 903–908.
Wangdell J, Friden J . Satisfaction and performance in patient selected goals after grip reconstruction in tetraplegia. J Hand Surg Eur Vol 2010; 35: 563–568.
Curtin CM, Gater DR, Chung KC . Upper extremity reconstruction in the tetraplegic population, a national epidemiologic study. J Hand Surg Am 2005; 30: 94–99.
Curtin CM, Wagner JP, Gater DR, Chung KC . Opinions on the treatment of people with tetraplegia: contrasting perceptions of physiatrists and hand surgeons. J Spinal Cord Med 2007; 30: 256–262.
Wagner JP, Curtin CM, Gater DR, Chung KC . Perceptions of people with tetraplegia regarding surgery to improve upper-extremity function. J Hand Surg Am 2007; 32: 483–490.
Anderson KD, Friden J, Lieber RL . Acceptable benefits and risks associated with surgically improving arm function in individuals living with cervical spinal cord injury. Spinal Cord 2009; 47: 334–338.
Matter B, Feinberg M, Schomer K, Harniss M, Brown P, Johnson K . Information needs of people with spinal cord injuries. J Spinal Cord Med 2009; 32: 545–554.
Hansberry DR, Agarwal N, Shah R, Schmitt PJ, Baredes S, Setzen M et al. Analysis of the readability of patient education materials from surgical subspecialties. The Laryngoscope 2014; 124: 405–412.
Cene CW, Dewalt DA . Left behind: ensuring clarity and completeness of our educational materials and messages. JAMA Intern Med 2013; 173: 583–584.
Paralyzed Veterans of America Consortium for Spinal Cord Medicine. Preservation of upper limb function following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med 2005; 28: 434–470.
Divanoglou A, Westgren N, Seiger A, Hulting C, Levi R . Late mortality during the first year after acute traumatic spinal cord injury: a prospective, population-based study. J Spinal Cord Med 2010; 33: 117–127.
Divanoglou A, Seiger A, Levi R . Acute management of traumatic spinal cord injury in a Greek and a Swedish region: a prospective, population-based study. Spinal Cord 2010; 48: 477–482.
Divanoglou A, Westgren N, Bjelak S, Levi R . Medical conditions and outcomes at 1 year after acute traumatic spinal cord injury in a Greek and a Swedish region: a prospective, population-based study. Spinal Cord 2010; 48: 470–476.
Divanoglou A, Levi R . Incidence of traumatic spinal cord injury in Thessaloniki, Greece and Stockholm, Sweden: a prospective population-based study. Spinal Cord 2009; 47: 796–801.
Bryden AM, Wuolle KS, Murray PK, Peckham PH . Perceived outcomes and utilization of upper extremity surgical reconstruction in individuals with tetraplegia at model spinal cord injury systems. Spinal Cord 2004; 42: 169–176.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
DISCLAIMER
The contents of this work do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
Rights and permissions
About this article
Cite this article
Fox, P., Suarez, P., Hentz, V. et al. Access to surgical upper extremity care for people with tetraplegia: an international perspective. Spinal Cord 53, 302–305 (2015). https://doi.org/10.1038/sc.2015.3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2015.3