Abstract
Objective:
To (1) examine the opinions of medical staff working in spinal cord injury (SCI) centres (SCICs); (2) evaluate their knowledge, attitudes and practices towards obesity prevention and management; (3) report the number of beds and dietitians available at each SCIC.
Methods:
A 37-item questionnaire was sent to 23 SCICs in the UK, the Netherlands, Belgium and the Republic of Ireland between September 2012 and January 2013.
Results:
Eighteen SCICs returned the questionnaires for analysis. All respondents stated that they had an interest in obesity treatment but only 2.3% of the respondents received training in obesity management. Sixty-one percent of staff did not consider body mass index (BMI) to be appropriate for use in SCI patients and subsequently less than half of the respondents use BMI routinely. The majority of respondents reported that they are confident in dealing with overweight (74.5%) and obese (66.1%) SCI adults, less than half (44.1%) are confident in treating overweight and obese SCI children. Respondents also indicated the need for nationally adopted guidelines and a lack of physical activity provision. There were 17.5 whole-time equivalent (WTE) dietitians recorded in 22 SCICs, equivalent to 47.8 beds per WTE dietitians (range 10–420). Non-UK SCIC dietitians are significantly better resourced than in UK SCICs (beds per WTE dietitian: 36 vs 124, P=0.035).
Conclusion:
Medical staff expressed the need to participate in obesity prevention and management. Appropriate training should be considered for all medical staff and the development of specific weight management guidelines and dietetic provision should be considered.
Similar content being viewed by others
Introduction
Obesity is common after spinal cord injury (SCI). It has become a major clinical and public health problem which requires several medical interventions, modifications of individual behaviour and environmental changes.1 Recent literature reported that up to 45% of SCI patients were overweight and 29% were obese.2,3 Obesity is recognised as both a cause and consequence of disease and it has been shown to be associated with poor clinical outcomes and increased healthcare costs.2 There are many health risks and co-morbidities including hypertension, diabetes, ischaemic heart disease, gallstones, osteoarthritis and some malignancies associated with obesity.1
Yet in clinical practise, many patients, allied health professionals and hospital managers do not realise how common obesity is in hospitalised patients.4,5 If ignored, this will cause a greater problem with the development of chronic nutrition-related complications.1
Among medical staff, knowledge of attitudes towards and practices in the management of obesity have been studied in various English-speaking countries, especially among general practitioners.6, 7, 8, 9 However, despite high awareness of obesity as a medically significant issue,10 the magnitude of the obesity epidemic remains high and is worsening, particularly in patients with neurological disabilities such as spinal cord injuries.2 Weight management is not commonly offered to SCI patients, at least not in the United Kingdom.11,12
SCI specialists have been identified as important potential contributors to the prevention and treatment of overweight and obesity, in part, because of continued involvement during rehabilitation. SCI medical staff are therefore in a unique position to provide guidance to patients. In some countries, SCI consultants will continue to see their patients as part of life-long followup. They are a frequently used source for information about weight control and are perceived to be a reliable formal source of information. However to our knowledge, no studies reporting the views of SCI specialists have been published.
A more detailed understanding of knowledge, attitudes and practise is necessary to determine the best way to facilitate the contribution of SCI medical staff to management of obesity after SCI. Although there are standard published recommendations for SCI management and optimal staffing levels,13,14 these documents do not make specific recommendations regarding obesity management.
While dietitians are considered essential members of the multidisciplinary team caring for patients with obesity management,1,15 the availability of dietitians in British and European SCICs remains variable.4
We therefore conducted this international survey in order to include all the SCICs in four western European countries including Belgium, the Republic of Ireland, the Netherlands and the United Kingdom as we assume that we share similar management approaches for SCI care. The aims of the study were: (i) to examine the opinions on weight management among medical staff working in SCICs; (ii) to evaluate their knowledge, attitudes and practices towards obesity prevention and management; (iii) to report the number of dietitians per bed available at each SCIC.
Methods
A 37-item cross-sectional survey was developed based on reviewed literature8 and was modified further by a team of multidisciplinary professionals working in SCICs.
Three 3-, 4- and 5-point scales were used, in which the participants had to indicate their level of agreement with each statement by selecting one from ‘strongly agree’, ‘agree’, ‘neutral’, ‘disagree’ or ‘strongly disagree’; or in practise statements, from ‘very confident’, ‘fairly confident’ or ‘not confident’ and in service statements, from ‘all of the time’, ‘most of the time’, ‘occasionally’ or ‘not at all’.
The questionnaire consisted of five sections; five questions on demographic data and staff awareness; 10 statements on exploring attitudes; three statements on self-efficacy; 11 statements on major limitations and; eight statements on service improvements.
In addition to gathering baseline demographic data and professional characteristics, a spokesman for each SCIC was asked to provide the number of available SCI beds and the number of whole-time equivalent (WTE) dietetic staff.
Because of the small sample size and for ease of presenting the data, most of the responses were grouped together, such that ‘agreed’ encompassed both ‘strongly agreed’ and ‘agreed’, ‘disagreed’ both ‘strongly disagreed’ and ‘disagreed’ and ‘most of the time’ referring to ‘all’ and ‘most of the time’.
Ethics
Formal ethical permission to conduct the study was not required by the Stoke Mandeville hospital review board as this was considered to be a clinical audit not involving active patient participation (National Research Ethics Service (NRES)).16 This was accepted by the other centres. The questionnaires were approved by the local clinical audit departments for phrasing and grammar of the questions. In addition, a pilot questionnaire was sent to three medical staff to assess the content and the time required to complete the questionnaire; feedback from this guided the drafting of the final version of the questionnaire (Supplementary Appendix 1). For Dutch and Belgian participants, the English survey was translated into native language by the study co-author (JvM) and validated by co-authors (ER) all of whom are competent in both languages (Supplementary Appendix 2).
Survey administration
The survey was administered to all medical staff working in the SCICs over four European countries (Belgium: n=3, the Republic of Ireland: n=1; the Netherlands: n=8 and the United Kingdom: n=11) between October 2012 and May 2013, with a covering letter addressed to the local medical lead explaining that findings would be used to identify current knowledge, attitude and practices of medical staff and to identify areas for improvement. Participants were reassured that all findings would be treated anonymously and in confidence to encourage respondents to answer honestly. Completed questionnaires were anonymised prior to analysis. Two reminders were sent (one at 8 weeks and one 12 weeks after the initial survey distribution).
Statistical analysis
Descriptive statistics were used to calculate the response frequency. Data are reported as medians (ranges).
Further statistical analysis was conducted to compare the existence of associations between respondents’ demographic and professional characteristics and their survey responses. In addition, the dietetics workforce was compared between UK and non-UK SCICs. For numeric data on an ordinal level, the Mann–Whitney test was used, and for cross-tabulation on a nominal level, the χ2-test was performed. The data were analysed using Minitab version 15 (Minitab, Coventry, UK) and significance was accepted if P<0.05.
Results
Medical staff from 23 SCICs were approached. The centres contained a total of 823 SCI beds (48 in Belgium, 36 in the Republic of Ireland, 258 in the Netherlands and 481 in the United Kingdom) (Tables 1 and 2).
The overall SCIC response rate was 78.4% (18/23 SCICs; 59 individual responses, 2–12 responses per SCIC, 63.6% in the United Kingdom (n=7), 66.7% in Belgium (n=2), 62.5% in the Netherlands (n=5) and 100% in the Republic of Ireland (n=1)).
Demographics and professional characteristics
Nearly half of the respondents were male (n=26). The median duration of practise in SCICs was 2.5 years. Fifty-four percent (n=32) of respondents were senior doctors/consultants (had completed training) and 67.8% (n=40) were from the UK SCICs (Table 1).
No junior/trainee doctors reported that they had received formal training in obesity management of SCI patients and only two (6.3%) senior doctors reported that they had formal training in this area.
Medical staff attitudes and knowledge towards obesity management
Forty-seven (76%) respondents agreed with the statement, ‘Obesity is a major health problem among patients with SCI and requires urgent action’. Non-UK respondents (100% vs 70%, P=0.037) and non-UK consultants (100% vs 71.4%, P=0.028) were more likely to agree with the statement than UK respondents (Table 3).
Most respondents believed that they have a role in obesity prevention (64.5%) and offer advice to their patients (77.9%). Most (86.5%) believed that advice on weight maintenance should be given to all patients with SCI in order to prevent obesity. Most respondents (86.4%) believed that weight management should be offered at an early stage rather than waiting until the patients are obese (18.6%).
Although all surveyed SCICs have dietitian support (Table 3), not all respondents reported that their centre has a dietitian that deals with weight management for SCI patients.
Obesity recognition
Most of the respondents (61%) reported that they do not believe that body mass index (BMI) is an appropriate measure to guide weight management in SCI patients. A minority (35.6%) of the respondents reported they monitor in-patients’ BMI. In the outpatient setting this is even less common (23.7%). Non-UK respondents were less likely to use BMI measurements (26.3% vs 35.6% in in-patients; 0% vs 35% in outpatients) than UK respondents.
Self-reported proficiency/ability
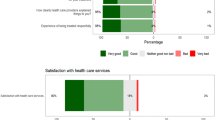
Most respondents felt more confident in treating overweight than obese SCI adults (Table 4). Three out of four respondents (74.6%) felt adequately trained to treat patients who are overweight, but only 2/3 (66.1%) of respondents rated themselves competent in managing obesity; fewer than half (44.1%) were confident in treating paediatric obesity, even though most centres were also responsible for the care of children with SCI (Table 4).
Significantly fewer UK respondents reported being confident in treating obese paediatric patients with SCI than non-UK correspondents (35% vs 63.2%, P=0.042, χ2: 4.144).
Barriers to weight management
The leading five obstacles, identified as limitations in delivering optimal care to obese patients, in descending order, were lack of nationally adopted guidelines (64.4%), lack of patient motivation and non-compliance (61%), lack of provision of a suitable physical activity programme (61%), short consultation time for medical staff (55.9%) and lack of specialist weight management clinics to which to refer patients (52.5%; Table 5).
Significantly more UK respondents reported short consultation times to be a limiting factor (70% vs 26.3%, P=0.015). Similarly, significantly more UK respondents felt they had inadequate training in providing lifestyle and behavioural counselling for their patients when compared with non-UK respondents (65% vs 21.1%, P=0.030).
Weight management strategies
All respondents felt an ideal weight management programme should include dietary advice (100%) and physical activity advice (100%). Leaflets and education material were rated as highly important as preventive measures and in general support (Table 6).
A large majority of respondents stated that family support (93.2%) and behavioural counselling (88.1%) were important. Most respondents would consider referrals of their patients to a dietitian (84.7%) as a first treatment step. Pharmacotherapy and bariatric surgery were the least used strategies, only 6.8% of respondents considered anti-obesity medications, and only 3.4% considered bariatric surgery as an option for weight management.
Dietetic provision in SCICs
The 22 responding centres house a total of 837 SCI beds. There were 17.45 WTE dietitians recorded; the median of 47.9 beds per WTE dietitian conceals a huge range (from 10–420). The workforce allocation is summarised in Table 2. Non-UK SCICs were significantly better resourced than UK SCICs (beds per WTE dietitian: 36 vs 124, P=0.035).
Suggestions
Ten out of fifty-nine respondents (16.9%) provided additional feedback. All responses were positive; common suggestions were the need for specific guidelines for weight management and opportunities to attend training.
Discussion
To the best of our knowledge, this is the first international multicentre survey to report on knowledge, attitudes and practices of SCIC medical staff in weight management and on the provisions of dietitians in SCICs. Previous surveys have primarily focused on obesity management among general practitioners and found that practices regarding obesity management vary widely.7, 8, 9
Weight gain after SCI is common. This is most likely due to reduced nutritional requirements secondary to enforced inactivity and immobilisation as a result of paralysis and changes in body composition,17 most marked in tetraplegia.18 In the long term, there seems to be a tendency for people with SCI to gain weight. Energy needs tend to decrease as a function of time post-injury related to loss of muscle mass. Desirable body weight/BMI for people with SCI may be lower than for the general population.19,20 After SCI, the percentage of body fat increases and muscle decreases. The body composition represented by a conventional BMI (overweight: >25 kg m−2; obese: >30 kg m−2) will be inappropriate after SCI. Buchholz’s19 and Laughton’s group 20 highlights that BMI values of over 22 kg m−2 are associated with high-fat mass in SCI individuals. The present study found that 61% of respondents considered BMI is to be an inappropriate measure to manage weight in SCI suggesting further research to define a disease-specific BMI or alternative measure is needed.
All respondents agree that successful weight management should start with prevention. Currently, there are no SCI-specific guidelines for prevention and management of overweight and obesity. Generic guidelines published by the UK National Institute for Health and Clinical Excellence suggest that dietary and lifestyle changes (a reduction in energy intake, following the eat-well plate set by the government)1 and increased physical activity in conjunction with behaviour modification support should be considered before any anti-obesity medications or bariatric surgery.20,21
Although weight loss has been advocated as a primary treatment strategy for obesity, to date, little high quality evidence exists to support this concept in patients with SCI. To our best knowledge, only limited trials have reported the effect of dietary interventions in obese SCI individuals. Studies demonstrate that a carefully planned programme with restricted dietary intake and lifestyle modification could be an effective way to reduce the body weight of obese patients with SCI without compromising total lean body mass and overall health.11,12
It is acknowledged that all patients with SCI should receive dietary advice in order to prevent obesity and its complications. In clinical practise, for all patients to be seen individually by a dietitian would lead to an unmanageable caseload. To offer educational material and input in patient education sessions may be an alternative, more effective and achievable approach. One UK SCIC offers dietetic input for patients with a BMI of 28 kg m−2 or above and the preliminary data has suggested that this approach has helped overweight individuals with SCI to reduce weight without compromising lean body mass.12
Dietitians see as their remit the management of factors related to obesity surrounding the physiological, psycho-social and ethnic needs of the patient. Professional guidelines and recommendations offer assistance on how dietitians might improve the quality of care and outcomes.2223 To tackle malnutrition and nutrition-related complications, the dietetic practise manual published by the British Dietetics Association has recommended that each SCIC should have access to a specialist dietitian in order to assess patients’ nutritional status and to provide further nutritional advice.22 More recently, the American Dietetic Association has also published guidelines for managing patients with SCI.24 It has emphasised the importance of a specialist dietitian in managing patients in acute, rehabilitation and community settings. The present study found considerable variation in dietetic provision among SCICs varied between centres and British centres have significantly lower dietetic provision when compared with some non-UK centres.
Strengths and limitations
The main strength of this study is that it is the first official international survey conducted in a multicentre European setting which obtained an overall 78.4% response rate from across four European countries.
Although the respondent sample size (n=59) was small, we feel that this still reflects the views of SCI doctors working in SCICs. To our knowledge, this represents at least 46.8% of all senior medical staff in the UK and Ireland SCICs (15 out of a total 32) which is comparable with the literature (53% response rate).25
Because the centre response rate varied from 2–12 responses per SCIC, some larger centres may be over-represented in the results. In addition, our technique of secondary invitation of respondents by selected lead individuals within a SCIC could introduce selection bias and we acknowledge this; however, guidance was provided to them to circulate the questionnaire to all medical staff, with varying degrees of experience and special interest, working in the SCIC.
There was a predominance of respondents from the United Kingdom (n=40) compared with non-UK respondents (n=19). Although this arguably over-represents one country’s perspective, it does not reflect the reality of staff mix in the SCI centres. The numbers of senior medical staff surveyed was comparable in the UK and non-UK centres (14 vs 19).
Conclusion
The present study found little variation in the knowledge, attitude and practices towards obesity prevention and management of medical staff working in the European SCICs. Limited knowledge among medical staff and variation in dietetic provision in SCIC are probably barriers to effective weight management.4 Without proper guidelines and training, it is unlikely that healthcare staff will have sufficient knowledge to identify at-risk patients or to offer appropriate treatment. This study reinforces the need to consider collaborating with national professional bodies to develop SCI-specific weight management guidelines which include clear guidance on optimal dietetic service provision within the SCICs.
Data Archiving
There were no data to deposit.
References
National Institute for Health and Clinical Excellence: Guideline on the prevention, identification, assessment and management of overweight and obesity in adults and children. NICE 2006 London http://www.nice.org.uk/nicemedia/live/11000/30365/30365.pdf, accessed 25Dec2013.
Wong S, Derry F, Jamous A, Hirani SP, Grimble G, Forbes A . The prevalence of malnutrition in spinal cord injured patients - a UK multicentre study. Br J Nutr 2012; 108: 918–923.
De Groot S, Post MW, Hoekstra T, Valent LJ, Faber WX, van der Woude LH . Trajectories in the course of body mass index after spinal cord injury. Arch Phys Med Rehabil 2014; 95: 1083–1092.
Wong S, Derry F, Grimble G, Forbes A . How do spinal cord injury centres manage malnutrition? A cross-sectional survey of 12 regional centres in the United Kingdom and Ireland. Spinal Cord 2012; 50: 132–135.
Wong S, Derry F, Graham A, Grimble G, Forbes A . An audit to assess awareness and knowledge of nutrition in a UK spinal cord injuries centre. Spinal Cord 2012; 50: 446–451.
Campbell K, Engel H, Timperio A, Cooper C, Crawford D . Obesity management: Australian general practitioners’ attitudes and practices. Obes Res 2000; 8: 459–466.
Thuan JF, Avignon A . Obesity management: attitudes and practices of French general practitioners in a region of France. Int J Obes 2005; 29: 1100–1106.
Al-Ghawi A, Uauy R . Study of the knowledge, attitudes and practices of physicians towards obesity management in primary health care in Bahrain. Pub Health Nutr 2009; 12: 1791–1798.
Fogelman Y, Vinker S, Lachter J, Biderman A, Itzhak B, Kitai E . Managing obesity: a survey of attitudes and practices among Israeli primary care physicians. Int J Obes 2002; 26: 1393–1397.
Kristeller JL, Hoerr RA . Physician attitudes toward managing obesity: differences among six speciality groups. Prev Med 1997; 26: 542–549.
Chen Y, Henson S, Jackson AB, Richards JS . Obesity intervention in persons with spinal cord injury. Spinal Cord 2006; 44: 82–91.
Wong S, Graham A . Grimble, Forbes A. Spinal Clinic for Obese Out-patient Project (SCOOP) – a 1 year report. Food Nutr Sci 2011; 2: 901–907.
Joint Standard Development Groups of the South England Review Group 2010 Standard for patients requiring spinal cord injury care (Revised 2010) http://www.secscg.nhs.uk/EasySiteWeb/getresource.axd?AssetID=99975&type=full&servicetype=Attachment, assessed 20 November 2010.
NHS England 2013 NHS standard contract for spinal cord injuries (all ages). NHS England, Redditch http://www.england.nhs.uk/wp-content/uploads/2013/06/d13-spinal-cord.pdf, accessed 9 September 2013.
Gall A, Turner-Stokes L . Guideline Development Group Chronic spinal cord injury: management of patients in acute hospital settings. Clin Med 2008; 8: 70–74.
National Research Ethics Service. Is Your Project Research? 2011. http://www.nres.nhs.uk/applications/is-your-project-research/, accessed on 24June2013.
Spungen A, Bauman WA, Wang J, Pierson RN . The relationship between total body potassium and resting energy expenditure in individuals with paraplegia. Arch Phys Med Rehabil 1993; 66: 420–426.
Mollinger LA, Spurr GB, El Ghatit AZ, Barboriak JJ, Rooney CB, Davidoff DD, Bongard RD . Daily energy expenditure and basal metabolic rates of patients with spinal cord injury. Arch Phys Med Rahabil 1985; 66: 420–426.
Buchholz AC, Bugaresti JM . A review of body mass index and waist circumference as markers of obesity and coronary heart disease risk in persons with chronic spinal cord injury. Spinal Cord 2005; 43: 513–518.
Laughton GE, Buchholz AC, Martin Ginis KA, Goy RE . Lowering body mass index cutoffs better identifies obese persons with spinal cord injury. Spinal Cord 2009; 47: 757–762.
Wong S, Barnes T, Coggrave M, Forbes A, Pounds-Cornish E, Appleton S, Belci M . Morbid obesity after spinal cord injury: an ailment not to be treated?. Eur J Clin Nutr 2013; 67: 998–999.
Joint Standard Development Groups of the South England Review Group. Standard for Patients Requiring Spinal Cord Injury Care (Revised 2010) 2010 http://www.secscg.nhs.uk/EasySiteWeb/getresource.axd?AssetID1/499975&type1/4full&servicetype=Attachment, accessed 20 November 2013.
Thomas B, Bishop J . Manual of Dietetic Practice. Blackwell Publishing: Oxford, 2007.
American Dietetic Association (2009) Spinal cord injury (SCI). Evidence-based nutrition practice guideline. American Dietetic Association, Chicago http://www.guideline.gov/content.aspx?id=14889, accessed 20 Nov 2013.
Ferrante J, Piasecki AK, Ohman-Strickland PA, Crabtree BF . Family Physicians’ practices and attitudes regarding care of extremely obese patients. Obesity 2009; 17: 1710–1716.
Acknowledgements
All authors contributed to the report. We are grateful to all medical staff facilitating the dissemination of study questionnaires from the UK, the Netherlands, Belgium and the Republic of Ireland. We also thank the following persons who provided information for this study: Anthony Twist, Sian Gruffudd, Carolyn Taylor, Kim Paterson, Philippa Bearne, Heather Nunn, Rees Colling, Nusrat Kauser, Tebbe Sluis, Christof Smit, Janneke Stolwijk, Dirk van Kuppevelt, Govert Snoek, Helma Bongers, Marga Tepper, Willemijn Faber, Hans Slootman, David Gobets, Catja Dijkstra, Casper van Koppenhagen and Annick Viaene. University College London (UCL) Staff receive support from the Biomedical Research Centre funding awarded to UCL and its partner Trust by the National Institute for Health Research.
Author contributions
SW: Protocol development, questionnaire development, data analysis, manuscript preparation. JvM: Questionnaire translation, manuscript revision. MB: Clinical supervision, manuscript revision. IvN: Local SCIC coordinator, manuscript revision. ER: Local SCIC coordinator, manuscript revision. ES- Local SCIC coordinator, manuscript revision. SH: Statistical supervision, manuscript revision. AF: Academic supervision, manuscript revision and guarantor.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Parts of the study data were presented at the International Spinal Cord Society annual conference in October 2013, in Istanbul, Turkey and the British Association of Parenteral and Enteral Nutrition annual meeting in November 2013, in Harrogate, UK.
Supplementary Information accompanies this paper on the Spinal Cord website
Supplementary information
Rights and permissions
About this article
Cite this article
Wong, S., van Middendorp, J., Belci, M. et al. Knowledge, attitudes and practices of medical staff towards obesity management in patients with spinal cord injuries: an International survey of four western European countries. Spinal Cord 53, 24–31 (2015). https://doi.org/10.1038/sc.2014.168
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.168