Abstract
Study design:
Prospective, randomized and controlled study.
Objectives:
The aim of the study was to investigate the effect of intermittent normobaric hyperoxia (InHO) for treatment of neuropathic pain in patients with spinal cord injury (SCI).
Setting:
The First Affiliated Hospital of Nanhua University, Hengyang, Hunan Province, China.
Methods:
Patients with SCI from Hunan Province were recruited from the First Affiliated Hospital of Nanhua University. History, duration, localization and characteristics of pain were recorded. Visual analog scale (VAS), the Patient Global Impression of Change (PGIC) and Short Form-36 walk-wheel (SF-36ww) was used to investigate the effect of InHO. Patients were randomly assigned to study and control groups. In study group, patients were exposed to pure oxygen via non-rebreathing reservoir mask, which increased the provided oxygen at a rate of 7 l min−1 for 1 or 4 h daily in 2 weeks. While in control group, patients breathed air via non-rebreathing reservoir mask at the same rate.
Results:
A total of 62 SCI patients with neuropathic pain were included in the study. The mean age of the patients was 36.85±10.71 years. Out of 62 patients, 21 were tetraplegic and 41 were paraplegic. Overall, 14 patients had complete SCI while 48 patients had incomplete injuries. Three groups were similar with respect to age, gender, duration, smoker or not, level and severity of injury. In the 4 h per day InHO groups, a statistically significant reduction of the VAS values was observed (P<0.05). Significant difference was also found in SF-36ww pain scores and PGIC (P<0.05). However, such an effect was not evident in the control group.
Conclusion:
This study revealed that in treatment of neuropathic pain of SCI patients, InHO may be effective.
Perspective:
This article presents InHO may effectively complement pharmacological treatment in patients with SCI and neuropathic pain.
Similar content being viewed by others

Introduction
Persistent pain is a frequent secondary complication following spinal cord injury (SCI), with approximately 70% of persons with SCI reporting some form of pain and approximately 30% of these manifests as neuropathic pain.1,2 In one-third of those, the pain is severe.3 Chronic neuropathic pain is often associated with conditions such as depression and anxiety, and strongly affects daily functioning and overall quality of life.4,5 Many people with SCI rate chronic neuropathic pain as one of the most difficult problems to manage. Pharmacotherapy includes anticonvulsants, antidepressants, opioids and local anesthetics,6,7 but responses vary and side effects limit compliance. Non-pharmacological treatments such as physical therapy, relaxation, hyperbaric oxygen and acupuncture are suggested.8, 9, 10, 11, 12, 13
Oxygen therapy has been clinically used for the treatment of chronic obstructive pulmonary disease and severe oxygen desaturation. Recent researches have reported that oxygen therapy appears to be effective in the pain management and show same effectiveness as hyperbaric oxygen.14, 15, 16 Though studies have revealed the analgesic effect of hyperbaric oxygen in both rats and human with neuropathic pain,13,17, 18, 19 costs and poor availability limit the use of hyperbaric oxygen. These prompt us to investigate the effect of intermittent normobaric hyperoxia (InHO) in the treatment of neuropathic pain.
In this randomized, double-blind, placebo-controlled study, we aimed to compare the effect of InHO with same flow rate of air in Chinese SCI patients with neuropathic pain.
Materials and methods
Participants
Patients with SCI from Hunan Province were recruited from the First Affiliated Hospital of Nanhua University. Individuals were considered eligible if they were between 18 and 62 years of age, with chronic pain that developed following injury, and SCI of more than 3 months' duration. Exclusion criteria included having a history of moderate-to-severe traumatic brain injury or diagnosis of severe psychiatric disorder. Due to InHO, those with chronic obstructive lung disease, pneumothorax, upper respiratory infection, fever, viral infection, history of seizure, optic nerve inflammation and history of ear surgery were also excluded. Women were excluded if they were pregnant or breastfeeding.
All patients were required to have a score >4 cm on the 10 cm visual analog scale (VAS) of the Short- Form-McGill Pain Questionnaire at screening (before a 2-week, single-blind, placebo run-in period) and at randomization. Neuropathic pain was diagnosed by the examination of an experienced physiatrist and confirmed with a LANSS score of 12 and above.20 All patients were prescribed to take 10 mg per day of amitriptyline at 2000 h for at least 15 days for a stable effect before treatment. We refrained from using any other medication for pain.20
This study was approved by the Medical Ethics Committee of the First Affiliated Hospital of Nanhua University, and all participants gave informed consent to participate.
Study design and treatment
This was an parallel-group, double-blind, randomized clinical trial comparing 2 weeks of flexible-dose InHO with placebo. In study group 1 (A group), patients were exposed to air for the first 3 h and then pure oxygen for 1 h via non-rebreathing reservoir mask for an hour at a rate of 7 l min−1.13,16 In study group 2 (B group), patients were exposed to pure oxygen for 4 h at the same rate.21,22 In control group, patients were exposed to air for 4 h via non-rebreathing reservoir mask. Randomization was preceded by a 2-week, single-blind, placebo run-in period; baseline data were collected at randomization.
Efficacy assessments
Spontaneous pain relief, the primary outcome variable, was assessed by asking participants to indicate the intensity of their current pain on a 10-cm VAS between 0 (no pain) and 10 (worst possible pain) after exposition. As a secondary measure of pain relief, we used the Patient Global Impression of Change (PGIC).23 To assess patients' quality of life, Short Form-36 walk-wheel (SF-36ww) a modification of the original SF-36 was used.24
Statistical analysis
Statistical analysis was performed using the SPSS 18.0 program (SPSS Inc., Chicago, IL, USA). Pre- and post-treatment values in the same groups were compared with paired samples Wilcoxon test. Pre- and post-treatment comparisons in different groups were performed using the Mann–Whitney U-test and repeated measures analysis of variance test.
The Fisher's exact test was used to compare groups by categorical variables. A value of P⩽0.05 was considered statistically significant.
Result
The primary outcome of patients
Sixty-two patients (39 men and 23 women) participated in the study. Patients' demographic characteristics are summarized in Table 1. Mean age was 36.85±10.71 years. No significant difference between groups was observed in gender, age and smoking or not.
Twenty-one patients were tetraplegic and 41 patients were paraplegic (Table 2).
Average period after injury was 10.25 months (3–21 months) for the patients studied. Average time lapse between the injury and the development of pain was 6.85 months (3–15 months) and average pain duration was 4.3 years (0.3–10.2 months). Locations of neuropathic pain are in Table 3. When locations and duration of pain, average time lapse between the injury and pain were compared, no statistically significant differences were observed between the groups.
Mean LANSS score was 15.25 (s.d.±3.28) with range 13–23.
The primary outcome of pain
On the first day, neuropathic pain mean VAS value of three groups were 5.68±1.41 in control group, 6.00±1.37 in A group and 5.39±1.53 in B group (Figure 1). No significant difference was observed in mean VAS value of the first day when compared (P=0.360).
After 2 weeks' treatment, mean VAS value of three groups were 5.65±1.53 in control group, 4.91±1.56 in A group and 3.53±1.64 in B group. In the 14th day mean VAS value, a statistically significant difference was observed between control and B group (P<0.001). B group also showed significant difference when compared with A group (P=0.006). Compared with control group, A group also showed decreasing VAS value, but did not reach significant difference (P=0.138).
To further investigate the effect of InHO during day time, we evaluated mean VAS value of there groups in the morning, noon, evening and night on the 15th day (Table 4; Figure 2). From the table, B group demonstrated significant difference compared with control group all the day. When compared with A group, B group showed significant difference among the morning (P=0.003), afternoon (P=0.002) and evening (P=0.002), but not at the night (P=0.079).
To further evaluate the long-term effect of neuropathic pain with SCI, day 30 and day 60 mean VAS scores were measured (Figure 3). Unfortunately, such analgesic effect faded in our trial (data not shown).
These results indicated that InHO therapy can reduce pain temporarily in neuropathic pain with SCI.
The secondary measure of pain relief and quality of life scales
On the GPIC, some improvement were reported among three group. Patients in B group showed improvement at day 14 in 42.9% (n=9), at day 30 in 23.8% (n=5) and at day 60 in 19.0% (n=4 ). Patients in A group reported improvement at day 14 in 23.8% (n=5), at day 30 in 14.3% (n=3) and at day 60 in 14.3% (n=3). Control groups showed improvement at day 14 in 20.0% (n=4), at day 30 in 15.0% (n=3) and at day 60 in 10% (n=2). Results were statistically significant at day 14 in B group compared with A group (P<0.001) and control group (P<0.001).
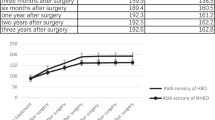
In the bodily pain domain of the SF-36ww, B group showed a significant improvement at day 14 compared with control group and A group, although not at days 30 and 60. The total score of the SF-36ww and other subdomains did not show statistically significant differences (see Figures 4 and 5).
Side effects
During the therapy, no side effect of InHO was seen.
Discussion
Nearly half of SCI patients are at risk of developing neuropathic pain.8,12 SCI-related neuropathic pain is often difficult to relieve. Pharmacotherapy includes anticonvulsants, antidepressants, opioids and local anesthetics,6,7 but responses vary and side effects limit compliance. More and more non-pharmacological treatments, including hyperbaric oxygen, have been introduced for the treatment of SCI-related neuropathic pain. However, few have been involved in InHO therapy. In the present study, we investigated the effect of InHO for treatment of neuropathic pain in Chinese patients with SCI in a case–control, prospective study. The result revealed normobaric hyperoxia therapy produced temporary analgesic effect in SCI patients.
In our study, 4 h InHO for 2 weeks significantly decreased VAS value (about 20%) among SCI patients with neuropathic pain. While 1 h treatment did not reach significant difference compared with treatment with air. Gu et al.13 reported that treatment with pure oxygen for 70 min for seven consecutive days did not significantly alter the increased thermal sensitivity in neuropathic rats. This result was accordance with ours in SCI patients with neuropathic pain. Maybe 1h InHO therapy is not enough to reach the point to produce analgesic effect. On the GPIC results, 4h per day InHO produced analgesic effect in 42.9% patients, which was <1h hyperbaric oxygen treatment (60–75%).13 To assess some aspect of quality of life scales, SF-36ww and PGIC were used. Significant difference was found only at day 14 in SF-36ww pain scores and PGIC results, which was accordance with the result of VAS scores. However, no significant difference was found in results of VAS scores, SF-36ww or PGIC beyond day 14. Unlike hyperbaric oxygen, long-term effects of InHO on quality of life was not found in our study. Besides, about 10–20% patients in control group also showed improvements after treatment with air in PGIC results. This was a little lower than the results in Gu’s report.13 Maybe SCI-induced neuropathic pain was more serious than idiopathic trigeminal neuralgia.
Celik et al.20 reported that neuropathic pain intensity was higher in the night than in the morning, noon and the evening. To investigate the effect of InHO therapy during day time, we used VAS four times daily after treatment for the evaluation of pain severity. Administration of 4h per day InHO reduced pain intensity all the day time compared with control group. However, no significant difference were reached when compared A with B group in the night. This might be the result of alterative pain intensity in the night.
Though the analgesic effect of oxygen therapy have been found for years, the mechanisms of therapeutic effect remain unknown. However, studies in neuroscience give us an insight into the mechanisms in neuropathic pain. First, normobaric hyperoxia treatment has been found to inhibit gp91(phox) expression, Akt activation, NADPH oxidase activity and MMP-2/9 induction;25, 26, 27 while Akt activation, NADPH oxidase activity and MMP-2/9 induction have been proven to have important roles in the formation and development of neuropathic pain.28, 29, 30, 31 Second, InHO can increase the expression of tumor necrosis factor-α converting enzyme, which can convert the transmembrane tumor necrosis factor-α into soluble tumor necrosis factor-α.21 Transmembrane tumor necrosis factor-α increases hypersensitivity of phenotype of sensory neurons and activate microglia.32,33 However, soluble tumor necrosis factor-α does not have that function. Third, normobaric hyperoxia can increase antioxidant enzyme activities (superoxide dismutase, catalase, glutathione peroxidase and glutathione reductase).34 Finally, antioxidant treatment has been proven to protect the spinal GABA neurons from impairment of oxidative stress and subsequently inhibit the development of neuropathic pain.35
There are also some limitations to our study. The most important one is low participant number and inability. Most studies on oxygen therapy in treatment with pain ranged from 15 to 70 min,14, 15, 16 and most studies of InHO in neuroscience designated 4 h per day for six consecutive days (almost a week) as their treatment.21,22,34 We regarded daily term (1 h per day, 2 h per day and 4 h per day) and weeks (1 week, 2 weeks and 4 weeks) of InHO therapy as factors. This meant that 10 groups of patients were required for our trial. Unfortunately, only 62 participants was not enough for so many groups. Besides, Gu et al.13 reported that treatment with pure oxygen for 70 min for seven consecutive days (1 week) did not significantly alter the increased thermal sensitivity in SCI rats. To make the trial proceeding, we only treated patients with 1 h per day and 4 h per day for 2 weeks.
Although statistical significance was detected for some variables, the power for detecting other differences might not have been sufficient, such as evaluation of anxiety, depression and sleep because of the concomitant medications. Nor a longer-term than 2 weeks of InHO was researched, either.
Future study might consist of a prospective study, which would allow for a more complete gathering of some other variables, a larger participant number and a more longer-term treatment of InHO. Ideally, such a study would be powered to obtain statistical significance from major variables of interest.
Conclusions
Until treatment options for SCI-related neuropathic pain become adequate, all interventions that might help a patient should be considered. InHO therapy may be an effectively complement pharmacological treatment in patients with SCI and neuropathic pain.
Data archiving
There were no data to deposit.
References
Bonica JJ . Introduction: Semantic, Epidemiologic, and Educational Issues. in Casey KL (ed). Pain and Central Nervous System Disease: The Central Pain Syndromes. Raven Press: New York, NY, pp 13–29, 1991.
Calmels P, Mick G, Perrouin-Verde B, Ventura M . Neuropathic pain in spinal cord injury: identification, classification, evaluation. Ann Phys Rehabil Med 2009; 52: 83–102.
Finnerup NB, Johannesen IL, Sindrup SH, Bach FW, Jensen TS . Pain and dysesthesia in patients with spinal cord injury: a postal survey. Spinal Cord 2001; 39: 256–262.
Harden N, Cohen M . Unmet needs in the management of neuropathic pain. J Pain Symptom Manage 2003; 25: S12–S17.
Wetering EJ, Lemmens KM, Nieboer AP, Huijsman R . Cognitive and behavioral interventions for the management of chronic neuropathic pain in adults—a systematic review. Eur J Pain 2010; 14: 670–681.
Moulin DE, Clark AJ, Gilron I, Ware MA, Watson CP, Sessle BJ et al. Pharmacological management of chronic neuropathic pain—consensus statement and guidelines from the Canadian Pain Society. Pain Res Manag 2007; 12: 13–21.
Attal N, Cruccu G, Haanpaa M, Hansson P, Jensen TS, Nurmikko T et al. EFNS guidelines on pharmacological treatment of neuropathic pain. Eur J Neurol 2006; 13: 1153–1169.
Norrbrink C . Transcutaneous electrical nerve stimulation for treatment of spinal cord injury neuropathic pain. J Rehabil Res Dev 2009; 46: 85–94.
Fattal C, Kong-A-Siou D, Gilbert C, Ventura M, Albert T . What is the efficacy of physical therapeutics for treating neuropathic pain in spinal cord injury patients? Ann Phys Rehab Med 2009; 52: 149–166.
Sun R, Kuo-Hsuan C . Neuropathic pain: mechanisms and treatments. Chang Gung Med J 2005; 28: 597–604.
To TP, Lim TC, Hill ST, Frauman AG, Cooper N, Kirsa SW et al. Gabapentin for neuropathic pain following spinal cord injury. Spinal Cord 2002; 40: 282–285.
Siddall PJ . Management of neuropathic pain following spinal cord injury: now and in the future. Spinal Cord 2009; 47: 352–359.
Gu N, Niu JY, Liu WT, Sun YY, Liu S, Lv Y et al. Hyperbaric oxygen therapy attenuates neuropathic hyperalgesia in rats and idiopathic trigeminal neuralgia in patients. Eur J Pain 2012; 16: 1094–1105.
Ozkurt B, Cinar O, Cevik E, Acar AY, Arslan D, Eyi EY et al. Efficacy of high-flow oxygen therapy in all types of headache: a prospective, randomized, placebo-controlled trial. Am J Emerg Med 2012; 30: 1760–1764.
Cohen AS, Burns B, Goadsby PJ . High-flow oxygen for treatment of cluster headache: a randomized trial. JAMA 2009; 302: 2451–2457.
Bennett MH, French C, Schnabel A, Wasiak J, Kranke P . Normobaric and hyperbaric oxygen therapy for migraine and cluster headache. Cochrane Database Syst Rev 2008: CD005219.
Li F, Fang L, Huang S, Yang Z, Nandi J, Thomas S et al. Hyperbaric oxygenation therapy alleviates chronic constrictive injury–induced neuropathic pain and reduces tumor necrosis factor-alpha production. Anesth Analg 2011; 113: 626–633.
Gibbons CR, Liu S, Zhang Y, Sayre CL, Levitch BR, Moehlmann SB et al. Involvement of brain opioid receptors in the anti-allodynic effect of hyperbaric oxygen in rats with sciatic nerve crush-induced neuropathic pain. Brain Res 2013; 1537: 111–116.
Zhao BS, Meng LX, Ding YY, Cao YY . Hyperbaric oxygen treatment produces an antinociceptive response phase and inhibits astrocyte activation and inflammatory response in a rat model of neuropathic pain. J Mol Neurosci 2014; 53: 251–261.
Celik EC, Erhan B, Gunduz B, Lakse E . The effect of low-frequency TENS in the treatment of neuropathic pain in patients with spinal cord injury. Spinal Cord 2013; 51 334–337.
Bigdeli MR, Rahnema M, Khoshbaten A . Preconditioning with Sublethal Ischemia or Intermittent Normobaric Hyperoxia Up-regulates Glutamate Transporters and Tumor Necrosis Factor-α Converting Enzyme in the Rat Brain. J Stroke Cerebrovasc Dis 2009; 18: 336–342.
Nasrniya S, Reza Bigdeli M . Ischemic tolerance induced by normobaric hyperoxia and evaluation of group i and ii metabotropic glutamate receptors. Curr Neurovasc Res 2013; 10: 21–28.
Bryce TN, Budh CN, Cardenas DD, Dijkers M, Felix ER, Finnerup NB et al. Pain after spinal cord injury: an evidence-based review for clinical practice and research: report of the National Institute on Disability and Rehabilitation Research Spinal Cord Injury Measures Meeting. J Spinal Cord Med 2007; 30: 421.
Lee BB, Simpson JM, King MT, Haran MJ, Marial O . The SF-36 walk-wheel: a simple modification of the SF-36 physical domain improves its responsiveness for measuring health status change in spinal cord injury. Spinal Cord 2009; 47: 50–55.
Liu W, Sood R, Chen Q, Sakoglu U, Hendren J, Cetin O et al. Normobaric hyperoxia inhibits NADPH oxidase‐mediated matrix metalloproteinase‐9 induction in cerebral microvessels in experimental stroke. J Neurochem 2008; 107: 1196–1205.
Jin X, Liu J, Liu KJ, Rosenberg GA, Yang Y, Liu W . Normobaric hyperoxia combined with minocycline provides greater neuroprotection than either alone in transient focal cerebral ischemia. Exp Neurol 2013; 240: 9–16.
Liu C, Weaver J, Liu KJ . Rapid conditioning with oxygen oscillation neuroprotection by intermittent normobaric hyperoxia after transient focal cerebral ischemia in rats. Stroke 2012; 43: 220–226.
Choi SR, Roh DH, Yoon SY, Kang SY, Moon JY, Kwon SG et al. Spinal sigma-1 receptors activate NADPH oxidase 2 leading to the induction of pain hypersensitivity in mice and mechanical allodynia in neuropathic rats. Pharmacol Res 2013; 74: 56–67.
Kawasaki Y, Xu ZZ, Wang X, Park JY, Zhuang ZY, Tan PH et al. Distinct roles of matrix metalloproteases in the early-and late-phase development of neuropathic pain. Nat Med 2008; 14: 331–336.
Puntambekar P, Mukherjea D, Jajoo S, Ramkumar V . Essential role of Rac1/NADPH oxidase in nerve growth factor induction of TRPV1 expression. J Neurochem 2005; 95: 1689–1703.
Guedes RP, Araújo ASR, Janner D, Belló-Klein A, Ribeiro MF, Partata WA . Increase in reactive oxygen species and activation of Akt signaling pathway in neuropathic pain. Cell Mol Neurobiol 2008; 28: 1049–1056.
Wu Z, Wang S, Gruber S, Mata M, Fink DJ . Full-length membrane-bound tumor necrosis factor-α acts through tumor necrosis factor receptor 2 to modify phenotype of sensory neurons. Pain 2013; 154: 1778–1782.
Zhou Z, Peng X, Hagshenas J, Insolera R, Fink DJ, Mata M . A novel cell–cell signaling by microglial transmembrane TNFα with implications for neuropathic pain. Pain 2010; 151: 296–306.
Bigdeli MR, Rasoulian B, Meratan AA . In vivo normobaric hyperoxia preconditioning induces different degrees of antioxidant enzymes activities in rat brain tissue. Eur J Pharmacol 2009; 611: 22–29.
Yowtak J, Wang J, Kim HY, Lu Y, Chung K, Chung JM . Effect of antioxidant treatment on spinal GABA neurons in a neuropathic pain model in the mouse. Pain 2013; 154: 2469–2476.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gui, Y., Li, H., Zhao, M. et al. Effect of intermittent normobaric hyperoxia for treatment of neuropathic pain in Chinese patients with spinal cord injury. Spinal Cord 53, 238–242 (2015). https://doi.org/10.1038/sc.2014.161
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.161