Abstract
Study design:
Literature review.
Objective:
To critically review all publications/internet sites that have described/used the Walking Index for Spinal Cord Injury (WISCI II), as a measure of impairment of walking function after spinal cord injury (SCI), in order to identify its psychometric properties, clarify its nature, specify misuse and incorporate the findings in an updated guide.
Method:
A systematic literature search was done of Ovid MEDLINE, CINAHL, PsychINFO, Cochrane Central Register of Controlled Trials, Scopus and electronic sites using key words: WISCI or WISCI II, SCI, paraplegia/ tetraplegia/ quadriplegia and ambulation/gait/walking. Among 1235 citations retrieved, 154 relevant articles/sites were identified, classified and examined by the authors; recommendations were made based on findings.
Results and Discussion:
The validity (face/concurrent/content/construct/convergent/criterion) and reliability of the WISCI II has been documented in clinical trials and clinical series, and considered adequate by systematic reviewers. In chronic SCI subjects, reliable determination of the maximum (as opposed to self-selected) WISCI II level requires more time and experience by the assessor. The correct use of WISCI II is clarified for testing acute/chronic phases of recovery after SCI, age of subjects, devices and settings. The WISCI II and walking speed measures may be performed simultaneously.
Conclusion:
The increased use of the WISCI II is attributed to its unique characteristics as a capacity measure of walking function and its strong metric properties. Appropriate use of the WISCI II was clarified and incorporated into a new guide for its use. Combining it with a walking speed measure needs further study.
Sponsorship:
This study was supported in part by grant #H133N000023 from the National Institute on Disability and Rehabilitation Research (NIDRR), Office of Special Education and Rehabilitative Services (OSERS), and US Department of Education, Washington, DC.
Similar content being viewed by others
Introduction
The Walking Index for Spinal Cord Injury (WISCI) is an ordinal scale that captures the extent and nature of assistance (combinations of orthoses, supporting equipment such as walkers and human helpers) that persons with spinal cord injury (SCI) require to walk. The original 19 levels, from unable to walk in spite of all possible supports to being able to walk without any, were rank-ordered by a panel of SCI experts to reflect gradations of impairment and their relationship to walking function.1 The WISCI scale was modified the following year to the WISCI II with the addition of two levels.2 Since its introduction, it has enjoyed increased popularity3 and acceptance4 as a capacity measure of walking function for use in clinical trials.
International SCI experts5, 6 have, however, recommended that the WISCI II2 be combined with the Ten Meter Walk Test (10MWT), another validated tool for quantifying walking function. Systematic reviews of the medical literature confirm the validity of the WISCI/WISCI II7 and its use together with the 10 MWT for assessment of ambulatory function.8
It has been recommended by some, nonetheless, that the WISCI II undergo further evaluation.6, 7, 9 Recent studies10, 11, 12 have demonstrated reliability and the relationship of WISCI II to both the severity of the injury and to walking speed. These studies also showed the need to progress subjects systematically10, 11 from their community (self-selected) WISCI II level (performance, in the terminology of the International Classification of Functioning, Disability and Health (ICF))13 to their maximum level (capacity, in ICF terms), which has not been clearly stated in existing instructions to clinical investigators,14, 15, 16 and does require additional time and training for obtaining accurate assessments.
Our purpose here is to critically review all publications and internet sites that have described and/or used the WISCI/WISCI II, in order to identify and clarify the nature, psychometric properties, correct use and misuse of the WISCI II. Recommendations for proper use, stemming from this review, are incorporated into an updated guide (Appendix 1: WISCI II Guide: Instructions for Use) suitable for use by clinical investigators and dissemination in the literature and appropriate websites.17
Materials and methods
A systematic search was performed of all papers as well as websites mentioning WISCI/WISCI II. The literature search was conducted with the assistance of a senior librarian from May to August 2011 and identified papers published from 2000 to August 2011 that explicitly mentioned the WISCI/WISCI II, and/or articles that dealt with the measurement of walking capacity in patients with SCI. Databases included Ovid MEDLINE, Ovid MEDLINE In-Process and Other Non-Indexed Citations, CINAHL, PsychINFO, Cochrane Central Register of Controlled Trials and Scopus, which includes Embase citations. All study designs, including case reports, were included, with no restrictions on the ages of participants. Non-English articles and animal studies were excluded. The following search terms were used: WISCI/WISCI II, SCI, paraplegia/tetraplegia/quadriplegia, ambulation/gait and walking/walking capacity. Citations were then imported into a RefWorks© database and duplicates removed, leaving 1235. In addition, other databases such as Google and a hand search of Spinal Cord yielded 12 citations not identified by the above strategy.
Two authors (GS and JFD) independently identified and classified the papers and (as applicable) their study design, which included both SCI and WISCI/WISCI II through a review of the abstracts, texts and references. A third author (PLD) reconciled differences and prepared results for circulation to the authors’ panel and subsequently to external reviewers. This yielded 168 citations from all sources, of which 14 were subsequently excluded as non-English, involving diseases other than SCI or animal research, for a total of 154 relevant references.
The list of 154 citations with their assigned classification is published as Supplementary Material (Supplementary Table 1). Sixteen of the 154 study citations examined underlying mechanisms of physiological changes and referenced the WISCI II scale. Ten of these 16 studies correlated changes in WISCI II scores with neurophysiological parameters, whereas 6 cited the WISCI/WISCI II only in the bibliography or for purposes of classification of the subjects.
Relevant citations included six systematic reviews of outcome measures for SCI, which referenced WISCI/WISCI II. Two reviews7, 8 assessed the validity and other psychometric properties of outcome measures for ambulation, including the WISCI II. Other reviews targeted measures of disability,18 general function or mobility19 or merely reference the WISCI II in studies on body weight-supported/robot-assisted gait training.20, 21 Articles7, 9 that identified limitations of the WISCI/WISCI II were studied carefully for issues related to the WISCI/WISCI II requiring clarification. Later, the guide for suggested future use of the WISCI II was edited by a coauthor (MS-R) who has trained clinical investigators in previous clinical trials in Asia, Europe and USA. The final guide was reviewed by the panel of authors and by outside reviewers for comment and approval. The outside reviewers were chosen to provide balance and reduce bias; Tania Lam7 and Hubertus van Hedel30 had published most of criticisms discussed in this manuscript.
A panel composed of authors of the WISCI/WISCI II identified the following issues for further analysis and discussion: the nature of the WISCI/WISCI II, the relationship of severity of injury to walking capacity, the validity, reliability and responsiveness of the scale and its correct use (see below).
Results and Discussion
Nature of the WISCI II
The WISCI II is unique as a walking capacity scale for individuals with SCI who have the capacity ‘to stand and walk,’ for several reasons. First, it has standard criteria for the testing environment, and subjects are progressed systematically through a validated sequence of capacity levels,22 incorporating devices and personal assistance, to their maximum walking capacity. Second, WISCI II ranks levels according to the severity of underlying impairment rather than the need for physical assistance, walking aids or braces (or their equivalent). The relationship between the severity of the impairment, reflected in the strength of leg muscles (lower extremity motor scores (LEMS)), and the WISCI II has been demonstrated in acute23 and chronic11 subjects with SCI. In fact, in subjects with acute SCI, the initial (baseline) LEMS is the best predictor of WISCI II score at 12 months post SCI onset, explains most of the variance in the WISCI II, and has high correlations with WISCI II improvement at 3, 6, 9 and 12 months.23 The strength of these correlations differ based on whether subjects are paraplegic or tetraplegic, the demographics of the population studied, and whether subjects have acute or chronic injuries.11, 24 Factors other than LEMS such as pain, spasticity or balance also contribute to walking function. Training has a major role in improvement in walking function for subjects with chronic SCI, in whom leg strength has been maximized and plateaued.24
The WISCI II’s levels reflect the underlying impairment and should not be dichotomized into dependent and independent levels based on physical assistance, in an attempt to more closely mirror a disability scale. Its unique features differentiate the WISCI II from disability scales, which may fail to identify differences in devices when assigning scores. As an example, the Functional Independence Measure (FIM) assigns a 6 for locomotion to an individual capable of modified independent ambulation regardless of the device(s) used; while the Spinal Cord Independence Measure (SCIM) progresses the ranking of devices from walking frame to one cane without addressing personal assistance at each level as discussed by Patrick.25
The WISCI II scale is an impairment-related capacity scale and the LEMS explains most of the variance (R2=0.85) of the WISCI score at 12 months in a multicenter randomized trial of 146 subjects.23 Capacity measures of walking function such as the WISCI II and walking speed utilized in research studies require standardized measurements of devices, distance and the environment. However, global disability scales (performance) such as the FIM reflect burden of care and describes what a person routinely does in their environment,13 which ‘may differ from individual to individual and from one time to another’.26 Curt27 reported significant functional improvement in activities of daily living at 12 months in 246 Asia A and B subjects assessed by the SCIM (a global disability scale) with no change in WISCI scores. This improvement is most likely owing to training alone (that is, compensation)27 as a subject with complete paraplegia may achieve wheelchair independence with no recovery in lower extremity strength. Thus, papers19, 28 that identify the WISCI II as a disability scale place it in the incorrect domain (ICF classification) and are in error.
Systematic progression justifies all WISCI II levels
In the original publications,1, 2 the ranking of the 21 levels was determined and validated by SCI specialists from eight countries. Order was determined by the severity of the underlying motor impairment, which resulted in some WISCI II levels that require physical assistance but few devices (that is, reflecting less impairment) being placed higher than other levels where subjects ambulate without physical assistance but more devices. This is one of the characteristics that distinguish the WISCI II as a capacity scale from disability scales, which always rank individuals who do not require human assistance higher, regardless of the use of devices. Some publications29, 30 noted that the observed frequency of some WISCI II levels (14 and 17) was low and therefore they might not be needed. It was also noted that the WISCI II instructions require clarification as to how to assess subjects’ walking capacity at follow-up after discharge from the hospital.
While prior guides1, 14 stated that during the acute period SCI subjects should be assessed at the highest possible level without compromising safety, as determined by a trained therapist, the precise method of systematic progression in chronic subjects has not been stated. Determining the maximum WISCI II level requires that subjects be progressed systematically through each level, as several studies10, 11 have shown that the maximal level may be 3 to 6 levels higher than the patient’s self-selected one. Marino’s study10 provides insight into how frequently WISCI II levels 14 and 17 are used during the progression of subjects from their self-selected to maximum WISCI II level. Over half (14/26) of the subjects progressed to or beyond level 14 during the determination of their maximal WISCI II level and almost a quarter (6/26) progressed to 17 or above. However, only 2 of 26 ended their progress at levels 14 or 17. In chronic subjects, the challenge is ensuring that the maximum level has been accurately evaluated. This method of progression for chronic subjects has been described in recent papers10, 11 and has been incorporated into the updated guide.17
Psychometric qualities of the WISCI II
Validity
One of the strongest features of the WISCI II, which has likely contributed to its broad acceptance, is high validity across multiple dimensions. The hierarchical ranking agreed on by the 24 experts in SCI walking function established content and face validity.1, 2 A subsequent prospective study22 of 170 subjects in four countries confirmed that progression through the levels followed a monotonic pattern in more than 80% of subjects, and the correlation of walking capacity (WISCI II) with impairment (LEMS) was 0.91 (P<0.001) at final assessment, supporting content and construct validity. Subsequent studies by our group and others have demonstrated criterion-related, predictive and concurrent validity, as well as both convergent and divergent construct validity.11, 22, 27, 29, 31, 32 The outcomes of the Spinal Cord Injury Locomotor Trial (SCILT)23 reported predictive, criterion and concurrent validity: the WISCI II was correlated with LEMS (impairment), balance, walking speed, 6-min walk (capacity), locomotor FIM (7 items) and the total motor FIM (13 items). Others studies have shown a correlation between the WISCI II and mobility measures such as the 10MWT, Timed up and Go test,31, 33 6-min walk test (6MWT),32, 34 Berg Balance Scale, SCIM and Spinal Cord Injury-Functional Ambulation Profile.33
Reliability and responsiveness
Although the validity of the WISCI/WISCI II has been well established, it has been suggested that further evidence of reliability and responsiveness is needed.6, 7, 18, 30 During the development of the WISCI II, a videotape was created of representative patients functioning at each level (40 randomized clips) and circulated to SCI experts. The data collected included 24 individual independent scorings and team scorings. The inter-rater reliability was 1.00 for individual participants and the eight participating teams.1 However, reliability here involved agreement on the nature and types of physical assistance, and aids the person used with walking.
A more crucial test for a capacity scale is whether two appropriately trained individuals agree on the same level of maximum capacity after assessing and progressing the same patient independently. In a study of subjects with chronic SCI, Marino and colleagues10 reported that inter- and intra-rater reliability were both 1.00 for self-selected WISCI II level. The intra-rater reliability for maximal level WISCI II was 1.00 and inter-rater reliability was 0.98. The progression from self-selected to maximal WISCI II level also showed good agreement between and within therapists. Recently, Scivoletto12 reported that inter-rater reliability was 0.98 for 19 acute patients.
The WISCI II was initially reported9 to have limited responsiveness in the period of 0–3 months post SCI onset and poor responsiveness in subsequent periods; however, the study cohort was small (n=22) and consisted of good walkers (70% with LEMS ⩾30). In a more representative sample of 886 persons with American Spinal Injury Association Impairment Scale (AIS) A, B, C and D injuries, the same group reported several years later4 that responsiveness was good in AIS C (N=137) and D (N=223) subjects, and equal to that of the 10MWT at 3, 6 and 12 months after injury.
In a study11 of 76 subjects with chronic SCI, WISCI II reproducibility was excellent, with an intra-class correlation coefficient of 0.99 for both the self-selected and maximum WISCI II level. The resulting smallest real differences of 0.79 (self-selected) and 0.60 (maximum) suggest that ‘a change of one WISCI II level can be interpreted as real in a chronic patient’.
The study of the psychometric properties of the WISCI II in chronic subjects has been limited to an assessment of reliability, reproducibility and validity in two studies.10, 11 Further validation in chronic subjects is warranted.
Use and misuse of the WISCI II
Past criticisms of the WISCI II include ceiling effects,7, 23, 30 floor effects,7 lack of responsiveness beyond 3 months,30 lack of clarity regarding the scoring of equivalents of short leg braces (for example, Alpine boots),3, 30 broad range of physical assistance,30 redundant categories30 and cultural differences in use of walking devices. Several of these, such as responsiveness and low-frequency (unneeded) categories, have been addressed above.
The ceiling effect and other limitations of walking function were addressed in the original publication1 by the statement ‘different distances (household and community), velocity and energy requirements will need to be added’. Two studies demonstrating the ceiling effect were reported in 2006; one with 22 subjects9 who were primarily AIS D, and the SCILT randomized controlled trial23 of 144 patients, which included AIS B, C and D subjects. In both studies, the subjects who reached the maximum WISCI II level of 20 were able to show improvement in the speed of walking in subsequent evaluations. Ceiling effects were one of the reasons that studies examining subjects at different distances and speeds were planned.10, 11, 35 Most authorities recommend combining the WISCI II with a measure of walking speed to compensate for this shortcoming. The floor effect has been mentioned in one systematic review,7 based on one study29 that included a large proportion (84/284) of AIS A SCI subjects. While this study has value for demonstrating validity and providing normative data, the WISCI II was not designed for AIS A subjects, as it was developed for subjects ‘who can stand and walk’.
Cultural issues
Cultural differences are an important consideration in planning a clinical trial and our group has shown differences across cultures for both clinical approaches to walking training and consumer preferences for walking with SCI.25, 36 For example, parallel bars are used far more frequently in the Europe than the USA,22 which reflects the therapists’ preference for equipment. This would change WISCI II baseline scores if this equipment was unavailable or at least not tried. In the context of an international trial, however, the effects of cultural differences are not limited to the types of walking aids and braces used, but also result from differences in methods/intensities of therapy and dissimilar lengths of stay, which may affect maximum WISCI II scores. Future multicenter studies across cultures (USA, Europe and Asia) must consider this in the design and protocol.
Braces
The ‘grouping’ of both short and long leg braces into one category ‘braces’3 and the variety of alternatives to short leg braces such as ‘alpine boots’30 has been raised as a problem when assigning WISCI II levels.
Our prospective study22 showed that the ‘descriptors’ for the different types of braces (short leg; long leg, unilateral, bilateral), as listed in prior WISCI II publications1, 2 and updated on the website,14, 17 may be used to record the types of braces used as subjects progress to their maximum WISCI II level. The information on the type of brace does not alter the scoring of the WISCI II level. However, recording the use of aids is an extremely important information in the design of a trial, because of potential cultural differences. Thus, the use of descriptors is recommended in planning cross-cultural trials (Appendix 1—WISCI II Guide: Instructions for Use).
This study revealed that the use of one (9%) or two (5%) long leg braces is far less common than the use of short leg braces (28%).22 Therefore, adding separate WISCI II levels to reflect all the possible brace combinations would result in a large increase in the number of levels, and does not seem warranted.
The criticism3 that advance reciprocating gait orthosis braces are not included needs clarification. Advance reciprocating gait orthosis braces and other devices enable subjects with complete injuries to ambulate with a spring loaded assist. Such mechanical devices could impact the correlation between an underlying motor impairment and demonstrated walking capacity, and were never intended to be part of the WISCI II assessment of SCI subjects who can ‘stand and walk’.
The descriptors (Appendix 1: WISCI II Guide: Instructions for Use) mentioned above are rarely reported by those who study and utilize the WISCI II other than the WISCI/WISCI II authors themselves.22 Based on these reports, several modifications of protocol language regarding walkers and braces have been adopted14 since the original publication. Some of the website descriptions15, 16 of the WISCI/WISCI II do not make mention of the expanded list of descriptors.
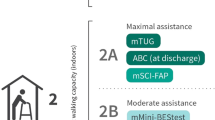
Physical assistance
For the WISCI II levels that incorporate physical assistance, there is the potential for variability in the extent of assistance provided. To provide additional clarification, the descriptors for specific amounts of physical assistance have been provided on the WISCI II scoring sheet. Descriptors A1 (Max Assist × 2 people) and A2 (Min/Mod assist × 2 people) apply only to WISCI II levels 1 and 2, both of which require maximal assistance. Descriptor A3 (Min/Mod assist × 1 person) applies to WISCI levels 3, 4, 6, 7, 8, 10, 11, 14 and 17. The Instructions for Use also clarify that any physical contact with the subject, including ‘contact guarding’, is considered as physical assistance.
Use in children
Although two of the websites15, 16 are kept current and can be updated through communication with the authors of the sites, there are several omissions/inaccuracies that have not been previously addressed by the WISCI/WISCI II authors. The first has to do with the use of the WISCI II for children. The psychometric properties (validity and reliability) of the WISCI II have not been evaluated for children aged 13 to 21, as implied by Rehab Measures.16 A study will be reported in 2012 that examines reliability in children.37
Qualifications of staff and time needed to administer the WISCI II
Another issue relates to the time required to perform the WISCI II test, where one site16 states ‘5 minutes’ while the other15 has ‘a minimal time’. While this is accurate for the acute and sub-acute phases of SCI, where therapists tend to know the capacity of their patients very well, recent studies in chronic subjects, who were not known to their assessors,10, 11, 35 describe the need for progressive testing of WISCI II levels from self-selected (SS) to maximum (Max), which may require 15 min. As there often is a difference of 3 to 6 levels between SS and Max, testing cannot be performed in 5 min (Appendix 1—WISCI II Guide: Instructions for Use).
Perhaps the issue that requires the greatest emphasis is the need for trained clinicians to perform the WISCI II assessments. In the acute and sub-acute phases, the therapist must determine the maximum WISCI II level and this requires a clinical judgment based on experience, because the subjects/patients are not capable of making a reliable judgment on what the minimum support needed for walking is as they begin to recover ambulatory function. After the patient is discharged to the community and returns for assessment 3 to 12 months post injury, the preferred WISCI II level is by definition self-selected. At times subjects have developed habits of walking without braces and with an unstable ankle, testing by a trained clinician is required to determine the appropriate maximum WISCI II level, especially to make judgments on patient safety that limit the maximum WISCI II.
Future Directions: Combining WISCI II with a Walking Speed Measure
Rationale
In exploring the reasons for combining the WISCI II with a measure of walking speed, we briefly examine the characteristics of both to demonstrate why each complements the other. The nature and limitations of the WISCI II, particularly its ceiling effect, have been discussed above. Subjects with a less severe initial injury may recover to the maximum WISCI II level of 20 within the first 3 months after SCI and will no longer see improvement on the WISCI II,9, 23 therefore further improvement in walking capacity requires assessing speed. Walking speed, however, has the limitation of a floor effect in clinical trials, as illustrated in the SCILT trial.38 The baseline data38 for walking speed, measured for 50 feet in the Dobkin trial, was assessed in <20% (20/142) of subjects, while all 142 subjects had baseline data for the WISCI II (median=1.49 and range 0–17). The walking speed for the 10MWT showed a floor effect30 in a large sample of 917 subjects, in which only 6 subjects were able to complete the 10MWT and Timed up and Go test at 2 weeks, compared with 74 at 1 month and 136 at 3 months. The ‘flying start’ or dynamic start of the 10MWT, as reported by van Hedel,30 requires subjects to walk a minimum of 14 m in order to assess the speed for the 10 middle meters, which are timed, and very few AIS C subjects are capable of this at 2 weeks. Upon examining the strengths and weaknesses of walking speed measures and WISCI II, it seems logical to combine the two. As the 10MWT can demonstrate improvement in less severely paralyzed subjects at later stages of recovery when there is often a ceiling for the WISCI II (level 20) and the WISCI II has far less of a floor effect at baseline assessment, the two tests complement each other. This idea is shared in the literature,7, 8, 39 and an international consensus conference on ambulation and gait6 recommended use of both measures in clinical trials. Our systematic search of the literature reveals that a combination of the two measures is used not only in clinical trials40 and case series,4, 31 but has been used to validate other measures.33
Is it possible to administer both tests at the same time?
If it is recommended to acquire the data at the same time (that is, during the same observed/timed10-m walk), the use of a dynamic start is not possible for standardized WISCI II testing. While some authors41 recommend a dynamic start with 2 m of acceleration before measurement of walking speed, others42 state that the static start with no acceleration is adequate. In a systematic review of walking speed research in neurological diseases,42 it was concluded that the static start is the preferred method for the 10MWT. In addition, Scivoletto43 has shown that in chronic incomplete SCI patients, walking speed with a static start does not differ significantly (P=0.092) from walking with a dynamic start. Subjects with the highest scores (WISCI II 18–20) and the lowest scores (WISCI II 9–12) showed no statistical difference between the two methods and inter-/intra-rater reliability was.98–99. Furthermore, Marino,10 Kim35 and Burns11 have reported excellent correlations of walking speed measured using a static start with WISCI II levels. Based on these recent studies, it appears that WISCI II and 10MWT may be performed simultaneously, but this will need to be investigated in larger populations.
Is a combined scoring system for WISCI II and 10MWT possible?
A single score that encompasses the two most important agreed-upon elements of walking capacity has tremendous research potential. The statistical method of blending the two metrics would be the most challenging issue.
A recent study of walking function reported by Musselman et al.33 attempted to validate a new measure that combines timed activities, use of devices and physical assistance into one metric. The authors employed both the 10MWT and the WISCI II to validate their instrument, which has many similarities to a combined 10MWT/WISCI II. The ordering of assistance, which combines walking aids (walkers, crutches and canes) and physical assistance from one person, however, does not take into account braces. It ‘encompasses the timed performance of 7 tasks, such as walking and negotiating obstacles, doors, and stairs.’ (p. 285), but not the walking capacity measured by the WISCI II or 10MWT, and may serve as a complement to these measures in a trial. However, the combining of the WISCI II and the 10MWT with timed activities would produce so many combinations and permutations that it is not feasible.
Conclusion
The increased use of the WISCI II may be attributed to its unique characteristics as a capacity measure of walking function, its strong metric properties and recommendations by international panels.5, 6, 39 A systematic review of the literature found over 150 WISCI/WISCI II citations, including clinical trials, cohort studies, case series, case reports, reviews and websites describing outcome measures. Recent studies using the WISCI II have addressed concerns regarding the reliability of data resulting from testing in chronic SCI subjects, where more time and experience by the assessor is required. Misunderstandings and inappropriate use of the WISCI II scale revealed in this review of the literature have required clarification and updating of the testing guide,17 which is published as an Appendix and will be disseminated electronically. The major future challenge is enhancing the utility of the WISCI II by combining it with a walking speed measure, in a statistically valid way.
References
Ditunno JF, Ditunno PL, Graziani V, Scivoletto G, Bernardi M, Castellano V et al Walking Index for Spinal Cord Injury (WISCI): an international multicenter validity and reliability study. Spinal Cord 2000; 38: 234–243.
Ditunno PL, Ditunno JF . Walking Index for Spinal Cord Injury (WISCIII): scale revision. Spinal Cord 2001; 39: 654–656.
Harvey L, Marino RJ . The walking index for spinal cord injury. Austr J Physiother 2009; 55: 66.
van Hedel HJ, Dietz V . Walking during daily life can be validly and responsively assessed in subjects with a spinal cord injury. Neurorehabil Neural Repair 2009; 23: 117–124.
Steeves JD, Lammertse D, Curt A, Fawcett JW, Tuszynski MH, Ditunno JF et al Guidelines for the conduct of clinical trials for spinal cord injury (SCI) as developed by the ICCP panel: clinical trial outcome measures. Spinal Cord 2007; 45: 206–221.
Jackson AB, Carnel CT, Ditunno JF, Read MS, Boninger ML, Schmeler MR et al Outcome measures for gait and ambulation in the spinal cord injury population. J Spinal Cord Med 2008; 31: 487–499.
Lam T, Noonan VK, Eng JJ . A systematic review of functional ambulation outcome measures in spinal cord injury. Spinal Cord 2008; 46: 246–254.
Labruyere R, Agarwala A, Curt A . Rehabilitation in spine and spinal cord trauma. Spine (Phila Pa 1976 ) 2010; 35: S259–S262.
van Hedel HJ, Wirz M, Curt A . Improving walking assessment in subjects with an incomplete spinal cord injury: responsiveness. Spinal Cord 2006; 44: 352–356.
Marino RJ, Scivoletto G, Patrick M, Tamburella F, Read MS, Burns AS et al Walking index for spinal cord injury version 2 (WISCI-II) with repeatability of the 10-m walk time: inter- and intrarater reliabilities. Am J Phys Med Rehabil 2010; 89: 7–15.
Burns AS, Delparte JJ, Patrick M, Marino RJ, Ditunno JF . The reproducibility and convergent validity of the Walking Index for Spinal Cord Injury (WISCI) in chronic spinal cord injury. Neurorehabil Neural Repair 2011; 25: 149–157.
Scivoletto G, Tamburella F, Calogere F, Molinari M, Ditunno JF . Walking Index for Spinal Cord Injury (WISCI) Reliability in Patients with Acute Spinal Cord Injury (SCI). International Congress on Spinal Cord Medicine and Rehabilitation 2011 Annual Meeting. Washington, DC, USAhttp://www.iscos.org.uk/page.php?content=64 (accessed 1 June 2012).
World Health Organization. ICF: International Classification of Functioning, Disability and Health. Geneva, Switzerland. 2001.
Patrick M, Marino RJ, Ditunno PL, Ditunno JF . Instructions for the Use of the Walking Index for Spinal Cord Injury II (WISCI II). Regional Spinal Cord Injury Center of the Delaware Valley. Thomas Jefferson University. 2005. http://www.spinalcordcenter.org/research/wisci_guide.pdf (accessed 1 June 2012).
Eng JJ Walking Index for Spinal Cord Injury (WISCI) and WISCI II. Spinal Cord Evidence (SCIRE) project. University of British Columbia. http://www.scireproject.com/outcome-measures/walking-index-spinal-cord-injury-wisci-and-wisci-ii (accessed 1 June 2012).
Raad J, Moore J . Rehab Measures: Walking Index for Spinal Cord Injury. Rehabilitation Measures Database. Rehabilitation Institute of Chicago 2011. http://www.rehabmeasures.org/Lists/RehabMeasures/DispForm.aspx?ID=957 (accessed 1 June 2012).
Patrick M, Marino RJ, Ditunno PL, Ditunno JF, Schmidt-Read M . Walking Index for Spinal Cord Injury II (WISCI II) Guide: Instructions for Use. Regional Spinal Cord Injury Center of the Delaware Valley. Thomas Jefferson University. 2012. http://www.spinalcordcenter.org/research/wisci_guide.pdf (accessed 18 October 2012).
Furlan JC, Noonan V, Singh A, Fehlings MG . Assessment of disability in patients with acute traumatic spinal cord injury: a systematic review of the literature. J Neurotrauma 2011; 28: 1413–1430.
Dawson J, Shamley D, Jamous MA . A structured review of outcome measures used for the assessment of rehabilitation interventions for spinal cord injury. Spinal Cord 2008; 46: 768–780.
Mehrholz J, Kugler J, Pohl M . Locomotor training for walking after spinal cord injury. Spine 2008; 33: E768–E777.
Swinnen E, Duerinck S, Baeyens J, Meeusen R, Kerckhofs E . Effectiveness of robot-assisted gait training in persons with Spinal cord injury: a systematic review. J Rehabil Med 2010; 42: 520–526.
Ditunno JF, Scivoletto G, Patrick M, Biering-Sorensen F, Abel R, Marino R . Validation of the walking index for spinal cord injury in a US and European clinical population. Spinal Cord 2007; 45: 275–291.
Ditunno JF, Barbeau H, Dobkin BH, Elashoff R, Harkema S, Marino RJ et al Validity of the walking scale for spinal cord injury and other domains of function in a multicenter clinical trial. Neurorehabil Neural Repair 2007; 21: 539–550.
Wirz M, van Hedel HJ, Rupp R, Curt A, Dietz V . Muscle force and gait performance:relationships after spinal cord injury. Arch Phys Med Rehabil 2006; 87: 1218–1222.
Patrick M, Ditunno P, Ditunno JF, Marino RJ, Scivoletto G, Lam T et al Consumer preference in ranking walking function utilizing the walking index for spinal cord injury II. Spinal Cord 2011; 49: 1164–1172.
Marino RJ . Domains of outcomes in spinal cord injury for clinical trials to improve neurological function. J Rehabil Res Dev 2007; 44: 113–122.
Curt A, van Hedel HJ, Klaus D, Dietz V . Recovery from a spinal cord injury: significance of compensation, neural plasticity, and repair. J Neurotrauma 2008; 25: 677–685.
Winchester P, McColl R, Querry R, Foreman N, Mosby J, Tansey K et al Changes in supraspinal activation patterns following robotic locomotor therapy in motor-incomplete spinal cord injury. Neurorehabil Neural Repair 2005; 19: 313–324.
Morganti B, Scivoletto G, Ditunno P, Ditunno JF, Molinari M . Walking Index for Spinal Cord Injury (WISCI): criterion validation. Spinal Cord 2005; 43: 27–33.
van Hedel HJ, Wirz M, Dietz V . Standardized assessment of walking capacity after spinal cord injury: the European network approach. Neurol Res 2008; 30: 61–73.
van Hedel HJ, Dietz V, Curt A . Assessment of walking speed and distance in subjects with an incomplete spinal cord injury. Neurorehabil Neural Repair 2007; 21: 295–301.
van Hedel HJ, Wirz M, Dietz V . Assessing walking ability in subjects with spinal cord injury: validity and reliability of 3 walking tests. Arch Phys Med Rehabil 2005; 86: 190–196.
Musselman K, Brunton K, Lam T, Yang J . Spinal cord injury functional ambulation profile: a new measure of walking ability. Neurorehabil Neural Repair 2011; 25: 285–293.
Lemay JF, Nadeau S . Standing balance assessment in ASIA D paraplegic and tetraplegic participants: concurrent validity of the Berg Balance Scale. Spinal Cord 2010; 48: 245–250.
Kim MO, Burns AS, Ditunno JF, Marino RJ . The assessment of walking capacity using the walking index for spinal cord injury: self-selected versus maximal levels. Arch Phys Med Rehabil 2007; 88: 762–767.
Ditunno PL, Patrick M, Stineman M, Morganti B, Townson AF, Ditunno JF . Cross-cultural differences in preference for recovery of mobility among spinal cord injury rehabilitation professionals. Spinal Cord 2006; 44: 567–575.
Calhoun CL, Mulcahey MJ . Pilot study of the evaluation of the validity and reliability of the Walking Index for spinal cord injury ii in young children with spinal cord injuries. J Pediatric Phys Med Rehab, In press.
Dobkin B, Apple D, Barbeau H, Basso M, Behrman A, Deforge D et al Weight-supported treadmill vs over-ground training for walking after acute incomplete SCI. Neurology 2006; 66: 484–493.
Alexander MS, Anderson KD, Biering-Sorensen F, Blight AR, Brannon R, Bryce TN et al Outcome measures in spinal cord injury: recent assessments and recommendations for future directions. Spinal Cord 2009; 47: 582–591.
Benito Penalva J, Opisso E, Medina J, Corrons M, Kumru H, Vidal J et al H reflex modulation by transcranial magnetic stimulation in spinal cord injury subjects after gait training with electromechanical systems. Spinal Cord 2010; 48: 400–406.
Salbach N, Mayo N, Higgins J, Ahmed S, Finch L, Richards C . Responsiveness and predictability of gait speed and other disability measures in acute stroke. Arch Phys Med Rehab 2001; 82: 1204–1212.
Graham JE, Ostir GV, Fisher SR, Ottenbacher KJ . Assessing walking speed in clinical research: a systematic review. J Eval Clin Pract 2008; 14: 552–562.
Scivoletto G, Tamburella F, Laurenza L, Foti C, Ditunno JF, Molinari M . Validity and reliability of the 10-m walk test and the 6-min walk test in spinal cord injury patients. Spinal Cord 2011; 49: 736–740.
Acknowledgements
We would like to thank Gary Kaplan, Senior Information Services Librarian for Scott Memorial Library at Thomas Jefferson University, for his assistance with the literature search; and Tania Lam and Hubertus van Hedel for their review and critique of the manuscript. Dr Ditunno’s research on the Walking Index for Spinal Cord Injury has been funded in part by a grant from the National Institute on Disability and Rehabilitation Research (NIDRR), Office of Special Education and Rehabilitative Services (OSERS), US Department of Education, Washington, DC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Spinal Cord website
Supplementary information
APPENDIX 1
APPENDIX 1

Walking Index for Spinal Cord Injury (WISCI II) Descriptors
Physical limitation for walking secondary to impairment is defined at the person level and indicates the ability of a person to walk after spinal cord injury. The development of this assessment index required a rank ordering along a dimension of impairment, from the level of most severe impairment (0) to least severe impairment (20) based on the use of devices, braces and physical assistance of one or more persons. The order of the levels suggests each successive level is a less impaired level than the former. The ranking of severity is based on the severity or the impairment and not on functional independence in the environment. The following definitions standardize the terms used in each item:
Physical assistance: Physical assistance of two persons is moderate to maximum assistance.
‘Physical assistance of one person’ is minimal to moderate assistance.
‘Contact guarding’ is minimal assistance.
Braces: ‘Braces’ means one or two braces, either short or long leg.
(Splinting of lower extremities for standing is considered long leg bracing).
‘No braces’ means no braces on either leg.
Walker: ‘Walker’ is a conventional rigid walker without wheels.
Crutches: ‘Crutches’ can be Lofstrand (Canadian) or axillary.
Cane: ‘Cane’ is a conventional straight cane.
Level Description
-
0 Unable to stand and/or participate in assisted walking.
-
1 Ambulates in parallel bars, with braces and physical assistance of two persons, but less than 10 m.
-
2 Ambulates in parallel bars, with braces and physical assistance of two persons, 10 m.
-
3 Ambulates in parallel bars, with braces and physical assistance of one person, 10 m.
-
4 Ambulates in parallel bars, no braces and physical assistance of one person, 10 m.
-
5 Ambulates in parallel bars, with no braces and no physical assistance, 10 m.
-
6 Ambulates with walker, with braces and physical assistance of one person, 10 m.
-
7 Ambulates with two crutches, with braces and physical assistance of one person, 10 m.
-
8 Ambulates with walker, no braces and physical assistance of one person, 10 m.
-
9 Ambulates with walker, with braces and no physical assistance, 10 m.
-
10 Ambulates with one cane/crutch, with braces and physical assistance of one person, 10 m.
-
11 Ambulates with two crutches, no braces and physical assistance of one person, 10 m.
-
12 Ambulates with two crutches, with braces and no physical assistance, 10 m.
-
13 Ambulates with walker, no braces and no physical assistance, 10 m.
-
14 Ambulates with one cane/crutch, no braces and physical assistance of one person, 10 m.
-
15 Ambulates with one cane/crutch, with braces and no physical assistance, 10 m.
-
16 Ambulates with two crutches, no braces and no physical assistance, 10 m.
-
17 Ambulates with no devices, no braces and physical assistance of one person, 10 m.
-
18 Ambulates with no devices, with braces and no physical assistance, 10 m.
-
19 Ambulates with one cane/crutch, no braces and no physical assistance, 10 m.
-
20 Ambulates with no devices, no braces and no physical assistance, 10 m.
Scoring Sheet for the Walking Index for Spinal Cord Injury II (WISCI II)


Rights and permissions
About this article
Cite this article
Ditunno, J., Ditunno, P., Scivoletto, G. et al. The Walking Index for Spinal Cord Injury (WISCI/WISCI II): nature, metric properties, use and misuse. Spinal Cord 51, 346–355 (2013). https://doi.org/10.1038/sc.2013.9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.9
Keywords
This article is cited by
-
A therapist-administered self-report version of the Walking Index for Spinal Cord Injury II (WISCI): a psychometric study
Spinal Cord (2024)
-
Exoskeleton-based training improves walking independence in incomplete spinal cord injury patients: results from a randomized controlled trial
Journal of NeuroEngineering and Rehabilitation (2023)
-
Multicentric investigation on the safety, feasibility and usability of the ABLE lower-limb robotic exoskeleton for individuals with spinal cord injury: a framework towards the standardisation of clinical evaluations
Journal of NeuroEngineering and Rehabilitation (2023)
-
Early and intensive motor training to enhance neurological recovery in people with spinal cord injury: trial protocol
Spinal Cord (2023)
-
International surveillance study in acute spinal cord injury confirms viability of multinational clinical trials
BMC Medicine (2022)