Abstract
Study design:
Retrospective study.
Objectives:
The purpose of this study was to identify the clinical factors for differentiating malignant from benign intramedullary spinal cord tumors.
Setting:
Niigata, Japan.
Methods:
We conducted a retrospective review of charts and images. Preoperative paralysis including walking ability, urinary function, magnetic resonance imaging (MRI) findings and pathological diagnosis were evaluated in 33 consecutive cases of intramedullary spinal cord tumor, and the clinical factors that were useful for differentiating malignant from benign tumors were identified.
Results:
Early progression of paralysis was the most valuable feature for differentiating malignant from benign tumors. Malignant tumors were suspected in only three of ten cases on the basis of MRI findings.
Conclusion:
Simple assessment of walking ability is easy to perform and is useful for predicting the pathological malignancy of intramedullary tumors of the spinal cord.
Similar content being viewed by others
Introduction
The treatment of malignant intramedullary tumors is challenging. Because of the invasive nature of such tumors, and the fact there is no barrier in the spinal cord, complete excision is very difficult in most cases, and surgical techniques that are usually performed for benign tumors have a risk of causing subarachnoid dissemination. On the other hand, most benign tumors can be surgically excised, and the functional prognosis is relatively good. Hence, preoperative differentiation of malignant tumors is important. In this study, we investigated the clinical factors that are useful for diagnosis of malignant intramedullary tumors, and found that simple assessment of walking ability was valuable.
Materials and methods
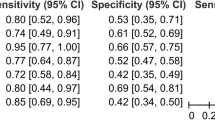
This retrospective study included 33 consecutive cases of intramedullary spinal cord tumor treated in one University Hospital from 1989 to 2009. For the purposes of the study, cases with a pathological diagnosis of grade I were considered benign, and those that were grade III or IV were considered malignant. Cases of grade II astrocytoma, or those for which the pathological diagnosis was unclear, were excluded. For each case, we reviewed the charts, pathology reports and magnetic resonance imaging (MRI) findings. Preoperative paralysis, walking ability, period from the onset of symptoms to gait inability if the patient was non-ambulatory, urinary function, MRI reports by radiologists and pathological diagnosis were investigated. Preoperative neurological status was graded using a standardized functional scale (Table 1).1, 2 Urinary dysfunction was graded according to the Japanese Orthopedic Association score for cervical compressive myelopathy.3 Neuropathologists in the Department of Pathology, Brain Research Institute, Niigata University, made pathological diagnoses basically according to the 2007 World Health Organization (WHO) classification and grading scheme.4 Data were analyzed using GraphPad Prism 5 (GraphPad Software, Inc., La Jolla, CA, USA). Numbers of ambulatory and non-ambulatory cases in each group were compared using the χ2-test. T-test was used for analysis of the period from disease onset until patients became non-ambulatory. Factors potentially useful for differentiating malignant from benign tumors were then identified.
Results
The pathological diagnosis was malignant in 10 cases (Table 2). Seven of these ten cases were high-grade malignant tumors, including glioblastoma and malignant lymphoma, and three were grade III glioma (anaplastic astrocytoma). In 23 cases, the tumors were diagnosed as benign. There were 3 grade 1 astrocytomas, 12 ependymomas, 7 hemangioblastomas and one subpial schwannoma.
Preoperative neurological status of each group is shown in Table 3. Twenty one cases of benign tumor were classified as grade 1 or 2 on the standardized scale, and the patients were able to walk without any assistance. One patient was able to walk with the help of a cane, and only one patient (4.3%) with a benign tumor could not walk. However, 9 of the 10 patients (90%) with malignant tumors were unable to walk (grade 4). The ratio of non-ambulatory patients was significantly higher in the malignant tumor group (P<0.0001). Another patient with a malignant tumor (anaplastic astrocytoma, WHO grade III) was able to walk but only with the assistance of a cane (standardized scale grade 3). The period from onset until a patient with a benign tumor becoming non-ambulatory was 82 months. Nine of the patients with malignant tumors, including all seven showing high-grade malignancy, became non-ambulatory within 90 days from the onset of symptoms, and 8, including all seven high-grade malignancy, became non-ambulatory within 60 days from onset (Table 2). The average period from onset until a patient becoming non-ambulatory was 28.9 days for high grade (WHO grade IV), and this was significantly shorter than 97 days for WHO grade III glioma (P<0.02) (Figure 1).
All of the patients with malignant tumors had urinary dysfunction. Seven were rated as having complete retention, two had severe disturbance and one had mild disturbance (Table 4). The pathological diagnosis in the latter case was anaplastic astrocytoma (WHO grade III). Urinary dysfunction was observed in only 2 of the 23 benign cases, and in both cases the dyfunction was rated as mild (Table 4). The ratio of severe disturbance and complete retention was significantly higher in the malignant tumor group (P<0.0001).
We reviewed the preoperative MRI reports for all cases. From the MRI findings, malignancy was suspected in only three of the 10 patients with malignant tumors. Although syrinx was not observed in 10 patients with malignant tumor, cystic lesion was observed within the tumor in one case.
We concluded that preoperative paralysis, especially walking ability and urinary dysfunction, and early progression of paralysis are useful factors for differentiation of malignant from benign tumors. Becoming non-ambulatory within 3 months from symptom onset and severe urinary disturbance were considered to be signs of malignant intramedullary tumor.
Discussion
Malignant intramedullary tumors are rare. However, their prognosis has been reported to be poor because of metastasis or central nervous system dissemination.5, 6, 7, 8 Preoperative recognition of malignant tumors is important for selection of the treatment, because in malignant cases conventional surgical resection has a risk of causing dissemination and local recurrence. Radiation therapy might be recommended without biopsy when diagnosis of metastatic intramedullary tumor is highly suspected from the history or images.8 Although surgical treatment of malignant intramedullary tumors, especially primary malignant tumors, is extremely difficult, transection of the spinal cord has been advocated, and can be a life-saving option in some cases.9, 10
In the present series, progression of paralysis was rapid in almost all patients with malignant intramedullary tumors, and this was well reflected in their loss of walking ability. Similar findings have been reported in the cases with malignant astrocytomas,1, 5, 11 a malignant lymphoma12 and metastatic tumors.8, 13 One reason for this rapid progression of paralysis is probably related to the fact that there is no barrier to tumor infiltration within the spinal cord. Another reason is the relatively small diameter of the cord. The corticospinal tract can be easily damaged because of its anatomical proximity, even if a tumor occurs in another part of the spinal cord, whereas this situation does not always arise in the brain.
Radiological differentiation of malignant from benign tumors, or radiological assessment of tumor grade in the central nervous system, is reported to be difficult, and this was also the case in the present study.14 Pathological diagnosis of biopsy samples from intramedullary tumors is sometimes difficult because biopsy of the central nervous system may cause neurological deficit, and thus any biopsy specimens tend to be very small.6 It is also possible that the final pathological diagnosis might change later from initial diagnosis of central nervous system biopsy.6, 14, 15 If clinical progression does not match the expected prognosis, the original pathological diagnosis should not be adhered to. If a patient is able to walk several months after the onset of symptoms and the initial pathological diagnosis is one of malignant intramedullary tumor, it is prudent to reconsider the diagnosis. Alternatively, if the pathological diagnosis is astrocytoma and the patient becomes unable to walk only 2 months after onset, it is possible that the biopsy specimen might not have been obtained from an appropriate part of the tumor.
Rapid progression of paralysis is thus a more valuable clinical indicator for differentiating a malignant from a benign intramedullary tumor, than radiological or pathological information. Metastatic tumor, malignant lymphoma, malignant glioma or other malignant tumor should be highly suspected if patients’s paralysis is very rapid especially when patients have gait disturbance within 2 months after the onset of neurological symptoms. Early recognition of the rapidness of the paralysis might facilitate the early diagnosis of malignant tumors before patients become non-ambulatory.
Conditions other than intramedullary spinal cord tumors including anterior spinal artery syndrome, neuromyelitis optica16 and sarcoidosis,17 and so on, sometimes show acute or subacute progressive myelopathy and MRI findings mimicking intramedullary tumor. Careful differential diagnosis is necessary and biopsy should be considered before treatment.
Conclusion
Rapid progression of paralysis, especially walking ability, is a useful clinical factor for differentiation of malignant from benign intramedullary tumors.
Data Archiving
There were no data to deposit.
References
Kim MS, Chung CK, Choe G, Kim IH, Kim HJ . Intramedullary spinal cord astrocytoma in adults: postoperative outcome. J Neurooncol 2001; 52: 85–94.
Jyothirmayi R, Madhavan J, Nair MK, Rajan B . Conservative surgery and radiotherapy in the treatment of spinal cord astrocytoma. J Neurooncol 1997; 33: 205–211.
Yukawa Y, Kato F, Ito K, Horie Y, Nakashima H, Masaaki M et al. ‘Ten second step test’ as a new quantifiable parameter of cervical myelopathy. Spine 2009; 34: 82–86.
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 2007; 114: 97–109.
Cohen AR, Wisoff JH, Allen JC, Epstein F . Malignant astrocytomas of the spinal cord. J Neurosurg 1989; 70: 50–54.
Santi M, Mena H, Wong K, Koeller K, Olsen C, Rushing EJ . Spinal cord malignant astrocytomas. Clinicopathologic features in 36 cases. Cancer 2003; 98: 554–561.
Donovan DJ, Freeman JH . Solitary intramedullary spinal cord tumor presenting as the initial manifestation of metastatic renal cell carcinoma: case report. Spine 2006; 31: E460–E463.
Watanabe M, Nomura T, Toh E, Sato M, Mochida J . Intramedullary spinal cord metastasis: a clinical and imaging study of seven patients. J Spinal Disord Tech 2006; 19: 43–47.
Nakamura M, Ishii K, Watanabe K, Tsuji T, Takaishi H, Matsumoto M et al. Surgical treatment of intramedullary spinal cord tumors: prognosis and complications. Spinal Cord 2008; 46: 282–286.
Ewelt C, Stummer W, Klink B, Felsberg J, Steiger HJ, Sabel M . Cordectomy as final treatment option for diffuse intramedullary malignant glioma using 5-ALA fluorescence-guided resection. Clin Neurol Neurosurg 2010; 112: 357–361.
Innocenzi G, Salvati M, Cervoni L, Delfini R, Cantore G . Prognostic factors in intramedullary astrocytomas. Clin Neurol Neurosurg 1997; 99: 1–5.
Bruni J, Bilbao JM, Gray T . Primary intramedullary malignant lymphoma of the spinal cord. Neurology 1977; 27: 896–898.
Connolly ES, Winfree CJ, McCormick PC, Cruz M, Stein BM . Intramedullary spinal cord metastasis: report of three cases and review of the literature. Surg Neurol 1996; 46: 329–337 discussion 337–338.
Rachinger W, Grau S, Holtmannspotter M, Herms J, Tonn JC, Kreth FW . Serial stereotactic biopsy of brainstem lesions in adults improves diagnostic accuracy compared with MRI only. J Neurol Neurosurg Psychiatry 2009; 80: 1134–1139.
Chandrasoma PT, Smith MM, Apuzzo ML . Stereotactic biopsy in the diagnosis of brain masses: comparison of results of biopsy and resected surgical specimen. Neurosurgery 1989; 24: 160–165.
Yanagawa K, Kawachi I, Toyoshima Y, Yokoseki A, Arakawa M, Hasegawa A et al. Pathologic and immunologic profiles of a limited form of neuromyelitis optica with myelitis. Neurology 2009; 73: 1628–1637.
Yukawa Y, Kato F . Isolated spinal cord sarcoidosis mimicking an intramedullary tumor. J Spinal Disord 1999; 12: 530–533.
Acknowledgements
We thank Yoshiaki Tanaka, and Masafumi Saito of the Department of Orthopaedic Surgery for their technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ito, T., Sawakami, K., Ishikawa, S. et al. Progression of paralysis is the most useful factor for differentiating malignant from benign intramedullary tumors. Spinal Cord 51, 319–321 (2013). https://doi.org/10.1038/sc.2012.152
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.152