Abstract
Study design:
The spinal cord injury ability realization measurement index (SCI-ARMI) assesses rehabilitation potential and efficacy based on the linear relationship between the Spinal Cord Independence Measure (SCIM) and the American Spinal Injury Association impairment scale (AIS) motor scores (AMS).
Objectives:
The objective of this study is to develop new SCI-ARMI formulas using a more flexible approach that is less sensitive to the distribution of the AMS score among spinal cord lesion (SCL) patients.
Setting:
Loewenstein Rehabilitation Hospital, Raanana, and the Statistical Laboratory, School of Mathematics, Faculty of Exact Sciences, Tel-Aviv University, Israel.
Methods:
SCIM III and AMS of 226 Israeli SCL patients were monitored. Linear formulas, quadratic formulas and non-parametric formulas were estimated to express the relationship between the 95th percentile of the SCIM III values for patients with given AMS at discharge from rehabilitation (SCIM95) and the corresponding AMS value. This relationship was used to calculate SCI-ARMI values, defined as the ratio of the observed SCIM score and the respective SCIM95 for a given patient's AMS score.
Results:
The estimated quadratic formula for the relationship between the 95th percentile of the SCIM III and the AMS score was found to be most appropriate, and formulas are provided for SCIM95 calculation in the various areas of function. The use of these formulas to calculate SCI-ARMI values is presented.
Conclusion:
The new formulas improve the accuracy of calculated ability realization for any AMS. The new statistical procedure will be used for the upcoming data analysis of a larger-scale international SCI-ARMI study.
Similar content being viewed by others
Introduction
The spinal cord injury ability realization measurement index (SCI-ARMI) is a measure for the assessment of disability weighted for the neurological deficit. Its advantages in evaluating quantitatively the independent role of rehabilitation in improving function beyond that of neurological recovery alone, and in assessing the prospect and the success of rehabilitation has already been described earlier.1
The SCI-ARMI value was defined as the ability realization value, calculated as the ratio of the actual functional performance and the potential performance, multiplied by the maximal Spinal Cord Independence Measure (SCIM) score that a healthy person can achieve.1, 2
The SCI-ARMI score (range 0–100), which can assist in the estimation of the prospect and effect of rehabilitation after a spinal cord lesion (SCL), is calculated combining the SCIM scores and the American Spinal Injury Association Impairment Scale (AIS) motor scores (AMS).3 This calculation was originally based on a linear relationship between the second version of SCIM (SCIM II) and AMS.1 Such a linear relationship, however, does not always exist in all score ranges. Furthermore, the method that was used to estimate it suffered from the small number of patients with SCIM and AMS scores in the lower range, which may have reduced the accuracy of the formula.
A different statistical approach was used in the present work to develop new SCI-ARMI formulas, not necessarily linear and not sensitive to the number of SCL patients available for each AMS. The newly developed formulas are based on the third version of SCIM (SCIM III),2 and not on SCIM II. In the original study, only the total SCIM score was investigated. In the current study, in addition to the formula corresponding to the total SCIM score, formulas corresponding to each SCIM III subscale were developed. This article presents the new SCI-ARMI development and examines its validity and utility.
Methods
Admission and discharge SCIM III and AMS scores were obtained from the records of 250 successive SCL inpatients treated in the Spinal Department of Loewenstein Rehabilitation Hospital between 2004 and 2010. Inclusion criteria were a SCL (AIS grades A, B, C or D) and age above 18 years. Patients with concomitant impairments such as brain injury or mental disease, or any condition (other than one caused by SCL) that might influence their everyday function were excluded. Other exclusion criteria were missing data, more than 2 weeks between SCIM and AIS examination dates on one hand and the corresponding dates of admission or discharge on the other, and more than 1 week between the SCIM and AIS examinations either at admission or at discharge. Two hundred twenty six patients met the inclusion criteria and were included in the analysis.
The mean age of the 226 patients was 51.3 years (s.d.=18.6); 65% of them were men; 48.2% had tetraplegia, the rest paraplegia. Admission AIS grade was A in 19% of patients, B in 2.7%, C in 23.9%, and D in 54.4%. Lesion etiology was traumatic in 38.9% of patients and non-traumatic in 61.1%. The traumatic etiologies were road accidents in 35.2%, falls in 30.7%, assault in 15.9%, work accidents in 11.4%, sporting accidents in 2.3%, suicide attempts in 1.1%, and other in 3.4%. The non-traumatic etiologies were spinal stenosis in 52.9%, disc diseases in 13.8%, tumors in 18.1%, vascular lesions in 7.2%, myelopathy of unknown origin in 3.6%, infection in 3.6%, and other in 0.7%.
Observed SCIM III and AMS values were obtained for every SCI patient. To produce a conservative estimate for the highest possible SCIM III given the patient's AMS value, we used the 95th percentile of SCIM III values at discharge from rehabilitation (SCIM95) for patients with a given AMS at discharge (AMSd). The advantage of the 95th percentile over the maximal observed value is that the latter estimate is a ‘moving target’ that tends toward 100% as the number of available patients increases; in other words, with a large enough population of patients sharing the same AMS score, we are likely to find an extraordinary patient with a SCIM score of 100. This does not reflect a stable feasible value. The reason for choosing discharge values was that at discharge from rehabilitation, ability realization is presumed to be maximal, and patients usually achieve the highest SCIM scores for given neurological states. The relationship between AMS and SCIM III values at discharge was estimated and tested using Spearman's correlation.
The SCIM95 equation specifies the highest SCIM III score that 95% of patients with similar AMS can achieve. To estimate SCIM95, we tried (a) linear formulas, (b) quadratic formulas and (c) non-parametric formulas for estimating the relationship between the 95% percentile at an AMS value and that AMS value. The various formulas were estimated using the statistical software environment R, implementing the quantile regression method for linear and quadratic formulas, and the LOWESS algorithm for non-parametric formulas.4, 5, 6
The two parametric formulas, the linear being a special case of the quadratic one, were compared using the likelihood ratio test. The two were further compared with the non-parametric LOWESS-based quantile regression,6 executing 1000 repetitions of random sub-sampling cross-validation. Each time, half of the data was chosen at random and used for fitting the three models. From the remaining observations, the 15th and the 85th quantiles of the AMS values were estimated, and the observations within that range were used for validation of the three models. The criterion for comparison of model prediction accuracy was the average percent included below the estimated SCIM95 line, with the desired number being 95%.
The 95% confidence interval for Spearman's correlation was obtained using the percentile bootstrap method, and so was the P-value, which coincides with the P-value obtained by the usual normal approximation for the permutation distribution.
SCI-ARMI gain values, and their dependence on various factors, were tested using sign test, two-sample Wilcoxon test, Spearman's correlation and the Kruskal–Wallice test, as appropriate.
Results
Mean AMSd values were 78.7 (median 85, range 7–100); mean SCIM III values at discharge were 70.7 (median 76.5, range 15–100). AMS and SCIM III values at discharge were moderately correlated (r=0.69, P<0.0001).
The quadratic formula for total SCIM95 as a function of AMS is presented in Figure 1a. The quadratic formula was found better than both the non-parametric and the linear formulas, as was evident from the cross-validation comparisons in which an average of 94.4, 90.6 and 93.3% of the observation within the validation samples were below the estimated SCIM95 line. Therefore, in the sequel, we used the quadratic formulas of SCIM95 for self-care, respiration and sphincter management, and mobility, shown in Figures 1b–d. The SCI-ARMI formulas derived from these SCIM95 formulas are displayed in Table 1.
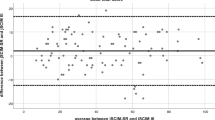
The correlation between SCI-ARMI values at discharge, calculated using the formula for total SCIM, and AMS at discharge was found to be statistically significant, but low: (r=0.28; P=0.00001). All SCI-ARMI values were higher after rehabilitation than before it, except for one patient (Figure 2a; P<0.00001). Hence, the gain was positive for practically all subsets of patients. The gain was similar in men and women (Figure 2c; P>0.25). SCI-ARMI gain values were higher at younger ages (Figure 2b; P<0.001), in traumatic than in non-traumatic SCL (Figure 2d; P<0.001) and in patients with lower AIS grades (Figure 2f; P<0.0001). SCI-ARMI gain tended to be higher at thoracic SCL levels, but the tendency was not found to be significant (Figure 2e; P>0.7).
Boxplots (mean±s.d.) and a scatter plot of the difference between discharge and admission SCI-ARMI values, showing that SCI-ARMI values after rehabilitation were higher than before rehabilitation in the entire patient population (a), across all ages (b), in both men and women (c), in both traumatic (T) and non-traumatic (NT) SCL (d), at any SCL level (e), and in patients with any AIS grade (f). The figures also show that SCI-ARMI gain values were higher in younger patients (b), in traumatic rather than non-traumatic SCL (d), in mid-thoracic SCL (e), and in patients with lower AIS grades (f).
Discussion
Caregivers customarily assess SCL patients’ expected functional status, using published data that relate function after presumably optimal rehabilitation of patients with complete SCL to the SCL level.7 In these assessments, the patient's actual functioning is compared with expected functioning by intuitive extrapolation, considering the actual severity of the patients’ SCL, which is frequently incomplete. This type of procedure may assist in assessing the rehabilitation potential, progress in rehabilitation and the efficacy of rehabilitation. But despite the negative correlation found between SCL level and the discharge functional score,8, 9 the sequence of levels of functionality at various SCL levels is highly inconsistent in patients with incomplete lesions. It may be extremely difficult, therefore, to perform a quantitative and reliable assessment of expected functional status in these patients intuitively, and to report quantitative data that explain the assessment of rehabilitation prospects or progress.
SCI-ARMI, which is based on the relationship between practically continuous scales, SCIM and AMS, allows a quantitative and reliable assessment of the relationship between actual and expected functioning of all patients, regardless of SCL completeness.1 SCI-ARMI shows how much of potential functioning the SCL patient is realizing, which indicates the amount of potential function the SCL patient is not realizing, in other words, the maximum function that can be added by rehabilitation. Comparison of SCI-ARMI before and after rehabilitation produces the SCI-ARMI gain, which presents quantitatively the functional progress that can be related mainly to rehabilitation.1 SCI-ARMI can also be used to minimize the confounding effect of rehabilitation in clinical trials, using daily function as an end point, by identifying rehabilitation systems with comparable efficacy. These qualities can make SCI-ARMI a useful instrument in clinical practice and research. But since the SCI-ARMI formula was first published in 2004, its availability only for the total score, the potential inaccuracy of the linear formula and the lack of a computerized instrument for automatic calculation of its value, based on routinely obtained measurements, have limited its use.
In the present study, we used a larger sample and a statistical method that minimizes the potential inaccuracy in the calculation of the SCI-ARMI formula. A software tool that incorporates formulas for all SCIM III tasks and automatically calculates SCI-ARMI (total score and scores for each subscale and task) when a patient's AMS and SCIM III values are entered, will be shortly available at: www.scimscore.com.
Assuming that daily function improved more than muscle power during rehabilitation, but not after it, SCIM95 values for any AMS are highest at discharge. Replacing the AMSd value in the SCIM95 formula, therefore, with an AMS value measured at any time yields a good estimate of the maximal SCIM scores that SCL patients can practically achieve for that AMS. Therefore, replacing the AMSd value with an AMS value measured at any time in the SCI-ARMI formula, which represents the ratio of the observed SCIM III and SCIM95 values, provides a good estimate of ability realization.
The new formulas presented here improve the accuracy of calculated ability realization for any AMS, because they reflect (a) the conditional SCIM III 95th percentile given the AMS, at any AMS, and (b) the non-linear relationship between the SCIM 95th percentile and the AMS.
The low correlation between total SCI-ARMI values calculated using the new formula and AMS confirms the relative isolation of measurements of function from the neurological status, thereby supporting the validity of the formula. The unconditioned improvement in SCI-ARMI (or ability realization) during rehabilitation also supports the validity of the new quadratic formulas.
The higher SCI-ARMI gain values at younger ages and in traumatic rather than in non-traumatic SCL may indicate better rehabilitation efficacy in these patient groups. The higher SCI-ARMI gain values in patients with lower AIS grades may indicate a ceiling effect for ability realization, which may be relatively high before rehabilitation in the higher AIS groups.
A limitation of SCI-ARMI, even with the quadratic formulas, is the representation of impairment by the AMS only, ignoring the possible contribution of sensory or autonomic deficits. Another limitation of the SCI-ARMI application is the potentially confounding effect of such factors as psychological status on rehabilitation. But, given that motor deficit and rehabilitation are usually the main factors affecting rehabilitation potential and efficacy, the current formulas can be useful for most SCL patients. Future refinement of the formulas, adding affecting variables, can improve their usefulness. Another limitation of the study is the fact that all patients were recruited from the same site. A forthcoming analysis of an international multi-center SCIM III and AMS data is expected to overcome this limitation.
In conclusion, new quadratic formulas that improve the accuracy of calculated ability realization for any AMS were developed, and findings support their validity.
Data Archiving
There were no data to deposit.
References
Catz A, Greenberg E, Itzkovich M, Bluvshtein V, Ronen J, Gelernter I . A new instrument for outcome assessment in rehabilitation medicine: spinal cord injury ability realization measurement index (SCI-ARMI). Arch Phys Med Rehabil 2004; 85: 399–404.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT et al. A multi-center international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord 2007; 45: 275–291.
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Medicine 2003; 26(Suppl 1): 50–56.
R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing 2011. Vienna, Austria. ISBN 3-900051-07-0, URL http://www.R-project.org/.
Koenker R . quantreg: Quantile Regression, R package version 4.67, URL http://www.r-project.org.
Sakov A, Golani I, Lipkind D, Benjamini Y . High-throughput data analysis in behavior genetics. Ann Appl Stat 2010; 4: 743–763.
Kirshblum S . Rehabilitation of spinal cord injury. In: DeLisa JA (ed). Physical Medicine and Rehabilitation, Principles and Practice. Lippincott Williams and Wilkins: Philadelphia, 2005, pp 1715–1752.
Middleton JW, Truman G, Geraghty TJ . Neurological level effect on the discharge functional status of spinal cord injured persons after rehabilitation. Arch Phys Med Rehabil 1998; 79: 1428–1432.
Van Hedel HJA, Curt A . Fighting for each segment: estimating the clinical value of cervical and thoracic segments in SCI. J Neurotrauma 2006; 23: 1621–1631.
Acknowledgements
The study was supported by the Loewenstein Rehabilitation Hospital Spinal Department Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Aidinoff, E., Benjamini, Y., Galili, T. et al. Non-linear formulas for the spinal cord injury ability realization measurement index. Spinal Cord 50, 324–327 (2012). https://doi.org/10.1038/sc.2011.145
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.145