Abstract
Study design:
Case report.
Objectives:
To describe a case of suprascapular nerve entrapment (SNE) in a patient with a spinal cord injury (SCI) as a cause of shoulder pain.
Setting:
Physical Medicine and Rehabilitation Institute, Nancy, France.
Report:
Six months after the occurrence of acute paraplegia T9 ASIA, a 45-year-old man complained of pain in the posterior and lateral areas of the left shoulder. A clinical assessment found an atrophy of the infraspinatus muscle and a muscular weakness during external shoulder rotation. SNE was suggested as a cause of pain and confirmed by nerve conduction recording. Magnetic resonance imaging excluded any compressive cyst. SNE at the spinoglenoid notch, related to upper limb overuse, was suggested. A gluco-corticoid injection in the proximity of the suprascapular nerve eliminated the pain in a few hours. Two months after the injection, the pain had not reappeared, the infraspinatus muscle atrophy was resolved, and supraspinal nerve conduction was normalized.
Conclusion:
Shoulder pain is common in individuals with paraplegia, but this is the first time that SNE has been reported as a cause of pain. This micro-traumatic pathology, well known in athletes, is probably under-diagnosed in patients with SCI who overuse their upper limbs for wheelchair propulsion and body transfers.
Similar content being viewed by others
Introduction
Shoulder pain in patients with spinal cord injuries (SCIs) is common1, 2 and may be disabling or alter the quality of life. Overusing the upper limbs for wheelchair propulsion and body transfers may induce significant constraints on the shoulder musculoskeletal system.1, 2 Micro-traumatic injuries can affect the suprascapular nerve. In this paper, we report suprascapular nerve entrapment (SNE) as an unusual cause of shoulder pain in a patient with SCI.
Case report
A 45-year-old man, without a medical history, had an idiopathic acute transverse myelitis, inducing a complete T9 paraplegia (ASIA motor scale 54/100, ASIA C). Six months after the onset of paraplegia, he complained of pain in the posterior and lateral area of the left shoulder, without traumatic injury. Pain increased with shoulder motion and during the night, and its intensity was estimated by the patient at 5/10 on a visual analogic scale. Functionally, he is restricted in wheelchair locomotion, in transfers and in grasping things above the shoulder level.
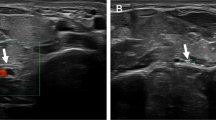
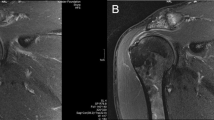
A clinical assessment found an atrophy of the infraspinatus muscle (Figure 1) and a muscular weakness during external shoulder rotation. There was no clinical sign of a rotator cuff tear, impingement syndrome, acromioclavicular joint disease or cervical disk disease. Distal motor latency of the suprascapular nerve (Figure 2) was increased on the left side (4.4 ms), whereas it was normal on the right side (3 ms, normal values: 3.3±0.5).3 The left infraspinatus muscle displayed electromyographic signs of denervation, whereas the left and right supraspinatus muscles and right infraspinatus muscle had normal electromyography. X-rays and magnetic resonance imaging of the left shoulder were normal, without indications of compressive cysts. For these reasons, SNE occurring at the nerve distal part at the spinoglenoid notch level was suggested. A gluco-corticoid injection in the proximity of the suprascapular nerve, associated with a partial rest of the upper limb, was followed by the complete elimination of pain less than 12 h after the injection. Two months after the injection, the pain had not reappeared, and the infraspinatus muscle atrophy was resolved. Distal motor latency of the suprascapular nerve as recorded on the infraspinatus muscle was normalized. Electromyographic signs of denervation persisted on the infraspinatus muscle, but the electromyographic trace was richer during voluntary activity.
Discussion
Shoulder pain is common in individuals who have SCI, its prevalence ranging between 35 and 51%.1, 2 Disorders affecting soft tissues (for example, tendons, muscles, bursae), bones or joints are frequent.2 To the best of our knowledge, this is the first time that SNE has been reported as a cause of pain shoulder in an individual with paraplegia.1, 4, 5 SNE has been reported in athletes as a non-frequent but under-diagnosed micro-traumatic pathology.4, 5
In individuals with SCI, the upper limbs are overused, especially in activities requiring strength (for example, wheelchair propulsion, transfers) and in activities requiring a wide range of motion (for example, grasping objects located over shoulder height). However, the joints of the upper limbs are not anatomically adapted to these kinds of activities. For this reason, overuse causes micro-traumatic lesions, such as SNE, as seen in athletes. SCI could be considered as a risk factor for developing this micro-traumatic condition.
Anatomically, the suprascapular nerve, which is derived from the upper trunk of the brachial plexus originating at C5 and C6 roots, can be injured at two locations: at the suprascapular notch, affecting both the supraspinatus and infraspinatus muscles, or at the spinoglenoid notch, affecting only the infraspinatus muscle. Clinically, SNE pain is located at the posterolateral area of the shoulder and can radiate to the lateral part of the shoulder or to the neck. Muscle weakness is usually found during shoulder abduction or external rotation. In severe cases, an atrophy of the spinati muscles can be observed, which obviously suggests SNE. However, in most cases atrophy is not present, and thus the diagnosis of SNE is difficult to affirm.4, 5
A local gluco-corticoid injection is usually performed for this pathology in athletic people.4, 5 In our patient, the gluco-corticoid injection had a rapid and lasting effectiveness. If this treatment is not effective, surgical nerve decompression can be proposed.4, 5 The early implementation of such treatments depends on a rapid diagnosis. However, we know that this pathology is under-diagnosed4, 5 and therefore certainly under-treated. In this case, the persistence of shoulder pain can have significant functional repercussions on the patient's locomotion and transfer capabilities and the ability to grasp objects over a certain height. Untreated SNE could thus be the origin of a diminished autonomy and a reduced quality of life. The psychological repercussions of chronic pain must also be taken into account.
Conclusion
This case report described micro-traumatic SNE in a patient with SCI. This is a rare cause of shoulder pain, but worth looking for, as the treatment is simple, cheap and effective. Better knowledge of this probably under-diagnosed pathology would allow the prevention and treatment of shoulder pain in individuals with SCI to be improved.
References
Dyson-Hudson TA, Kirshblum SC . Shoulder pain in chronic spinal cord injury, Part I: Epidemiology, etiology, and pathomechanics. Spinal Cord Med 2004; 27: 4–17.
Hastings J, Goldstein B . Paraplegia and shoulder. Phys Med Rehabil Clin N Am 2004; 15: vii, 699–718.
Delisa JA, Mackenzie K, Baran EM . Manual of Nerve Conduction Velocity and Somatosensory Evoked Potentials, 2nd edn. Raven Press: New York, 1987.
Vastamäki M, Göransson H . Suprascapular nerve entrapment. Clin Orthop 1993; 297: 135–143.
Antoniadis G, Richter HP, Rath S, Braun V, Moese G . Suprascapular nerve entrapment: experience with 28 cases. J Neurosurg 1996; 85: 1020–1025.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Facione, J., Beis, J., Kpadonou, G. et al. Suprascapular nerve entrapment in a patient with a spinal cord injury. Spinal Cord 49, 761–763 (2011). https://doi.org/10.1038/sc.2010.89
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.89
Keywords
This article is cited by
-
Anterior interosseous nerve neuropathy in a patient with spinal cord injury: case report and literature review
Spinal Cord Series and Cases (2022)