Abstract
Study design:
Small case series of patients with cervical spondylotic amyotrophy (CSA) managed by conservative treatment with hyperbaric oxygen (HBO) therapy.
Objective:
To study the effects of conservative treatment with HBO therapy of CSA patients.
Setting:
Department of Orthopaedic Surgery, Imakiire General Hospital, Kagoshima, Japan.
Methods:
This study included 10 patients with CSA who underwent rehabilitation, including cervical traction and muscle exercise, for some period of time but did not respond well to it, and were then managed by additional HBO therapy for rehabilitation. Information was obtained on the duration of symptoms and strength of the most atrophic muscle, intramedullary high-signal-intensity changes on T2-weighted magnetic resonance imaging, presence of ‘snake-eyes’ appearance and the number of stenotic canal levels.
Results:
The mean duration of symptoms before HBO treatment was 3.1 months. The axial T2-weighted magnetic resonance images of all 10 patients showed a ‘snake-eyes’ appearance. The mean number of stenotic canal levels was 0.3. There was marked improvement on manual muscle testing from a mean of 1.9 pretreatment to a mean of 4.4 at the last follow-up after HBO therapy. The outcomes of all 10 patients, whose results were classified as excellent or good, were considered clinically satisfactory.
Conclusion:
To our knowledge, conservative treatment with HBO therapy for CSA patients has not previously been described. It appears that HBO therapy might improve ischemic injury of the anterior horns in CSA patients with short duration of symptoms.
Similar content being viewed by others
Introduction
Cervical spondylotic amyotrophy (CSA) is a well-known but rare condition with cervical spondylosis characterized by severe muscle atrophy and weakness in the upper extremities without significant sensory deficits.1, 2 Cases of CSA can be grouped into a proximal type with atrophy of proximal muscles, including the deltoid, biceps and triceps; distal type with atrophy of muscles of the forearm and hands; and diffuse type with atrophy of both proximal and distal muscles. The pathophysiology and treatment of this condition remain controversial.
HBO therapy, which is widely performed for patients in hypoxic condition, is an attractive method of treatment that has frequently been used for several neurological conditions, including stroke, cerebral palsy, brain injury and spinal cord injury.3, 4, 5, 6, 7 HBO therapy has been shown to decrease tissue edema, improve blood flow and promote oxygen delivery, leading to an increase in the oxygen level in neuronal tissues and enhancement of cellular and metabolic functions.8
To our knowledge, the effectiveness of conservative treatment with HBO therapy for the management of CSA has not been reported. Herein, we report a small case series of CSA successfully managed by conservative treatment with HBO therapy and review the literature.
Materials and methods
This study included 10 patients with CSA who underwent rehabilitation, including cervical traction and muscle exercise, for some period of time but did not respond well to it, and were then managed by additional HBO therapy for rehabilitation. Approval was obtained from the Institutional Review Board of the Imakiire General Hospital. The mean age of the patients was 58 years (range: 45–74 years), and there were seven male and three female patients, including seven with proximal type, two with distal type, and one with diffuse type of the disease. All patients had muscle atrophy of the upper extremities without gait disturbance or sensory deficit. Denervation potentials and decreased motor unit potentials were found in the atrophic muscles on standard needle electromyography, but abnormal electromyographic findings were not noted in the thoracic paraspinal muscles and lower extremity muscles in all 10 patients.
Information was obtained on the duration of symptoms and strength of the most atrophic muscle, which was evaluated using manual muscle testing (MMT). Imaging studies included plain radiographs and magnetic resonance imaging (MRI) of the cervical spine. T2-weighted MRI was examined for intramedullary high-signal-intensity changes and ‘snake-eyes’ appearance, a high-intensity area in the anterior horns. The number of stenotic canal levels was also investigated. Cases with disappearance of the subarachnoid space on the sagittal T2-weighted MRI were considered to have spinal canal stenosis.
Response to HBO treatment
In accordance with our protocol, patients received HBO (100% O2 at 2 atm absolute for 1 h) once daily for a total of 10–20 cycles. Improvements in muscle strength were classified from excellent to poor (excellent, more than 2 grades of improvement on MMT or recovery to MMT grade 5; good, 1 grade of improvement on MMT; fair, no improvement on MMT; poor, worsening on MMT). Excellent and good outcomes were considered clinically satisfactory, while fair and poor outcomes were considered unsatisfactory.
Results
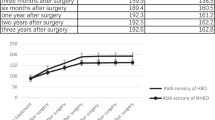
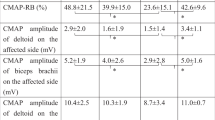
There was a marked improvement in MMT grades from a mean of 1.9 (range: 1–2) before treatment to a mean of 4.4 (range: 3–5) at the last follow-up after HBO. The mean follow-up period was 19.5 months (range: 12–36 months) in the 10 patients with CSA. Nine patients were classified as having excellent and one patient with distal type CSA as having good improvement in muscle strength. No patient in this case series was classified as fair or poor. Thus, the outcome of all 10 patients was considered clinically satisfactory. The mean duration of symptoms before HBO treatment was 3.1 months (range: 1–12 months). The duration of symptoms before HBO treatment was shorter in patients classified as having excellent improvement, with a mean of 2.1 months (range: 1–5 months), than in patients classified as having good improvement, who had a 12-month duration of symptoms. Sagittal T2-weighted MRI revealed intramedullary high-signal-intensity changes in seven patients, including six patients classified as having excellent improvement and one patient classified as having good improvement. ‘Snake-eyes’ appearance was noted on the axial T2-weighted MRI in all 10 patients. The mean number of stenotic canal levels was 0.3 (range: 0–2), and no stenotic canal level was observed in eight patients, including seven patients classified as having excellent improvement and one patient classified as having good improvement (Tables 1 and 2).
Representative cases
Case 1
A 74-year-old woman experienced weakness of the right hand muscles and difficulty with finger motion after physical exercise. The weakness gradually progressed, but was then stable for 2 months. Neurological examination revealed muscle weakness of the right forearm and hand muscles (grade 2/5 on MMT). The intrinsic muscles of both hands exhibited severe atrophy. Sensation was intact, as were the cranial nerves. Deep-tendon reflexes in the upper and lower extremities were normal bilaterally, without pathological reflexes. Electromyographic findings were compatible with denervation of the muscles innervated by C7, C8 and T1 bilaterally, with right-sided predominance. Sagittal T2-weighted MRI revealed slight intramedullary hyperintensity at the level of C4–C5 (Figure 1a). Axial T2-weighted MRI revealed high-intensity areas in the anterior horns from C5–C6 to C6–C7, with right-sided predominance (Figure 1b). The patient underwent cervical traction for 1 week, but her symptoms did not change markedly. She therefore began to undergo once-daily HBO treatment for 13 days. The duration between the onset of symptoms and start of HBO treatment was 3 months. Each HBO treatment involved pressurization to 2 atm absolute for 1 h. The muscle weakness of the right forearm and hand muscles gradually improved and recovered well by the end of HBO therapy (grade 4/5). Her condition has been stable for the past 3 years.
Case 2
A 62-year-old man experienced muscle weakness of the right shoulder and arm, which gradually progressed. Although a private clinician had treated him with rehabilitation for 4 months, his muscle weakness did not improve, and he was referred to our hospital. Neurological examination revealed severe bilateral muscle atrophy of the shoulders and arms, predominantly on the right side, as well as weakness of the right deltoid, biceps and brachioradialis muscles (grade 2/5). Sensation was normal. The biceps reflexes were diminished and the triceps reflexes were hyperactive bilaterally. Deep-tendon reflexes in both lower extremities were slightly hyperactive. He had a normal gait, without spasticity. Electromyographic findings were compatible with denervation of the muscles innervated by C5 and C6 bilaterally, with right-sided predominance. Sagittal T2-weighted MRI revealed cord compression with a region of intramedullary hyperintensity at the level of C3–C4 (Figure 2a). Axial T2-weighted MRI revealed high-intensity areas in the anterior horns from C3–C4 to C5–C6, with right-sided predominance (Figure 2b). HBO therapy was performed once a day for 11 days, under an absolute atmospheric pressure of 2 atm for 1 h. The duration of symptoms before HBO treatment was 5 months. The patient noted gradual improvement already during and marked improvement of his motor symptoms at the end of HBO therapy (grade 3/5). At 3 months after HBO therapy, the strengths of the right deltoid, biceps and brachioradialis muscles were each of grade 4/5. His condition has remained stable for the past 34 months.
Discussion
Whether the pathogenesis of CSA involves selective injury to the ventral nerve roots, the anterior horns of the cervical spine or both has remained unclear. Keegan1 reported a case of dissociated motor loss in the upper extremity with cervical spondylosis, which was attributed to selective compression of the ventral nerve roots. Yanagi et al.2 have attributed this syndrome to circulatory insufficiency in the territories of the spinal central arteries leading to ischemic injury of the anterior horn cells. In addition, some authors believe that CSA is caused by selective injury of the anterior horns in the spinal cord, on the basis of T2-weighted MRI findings of a ‘snake-eyes’ appearance of symmetric intramedullary high-signal intensity areas and findings of delayed enhanced computed tomography of intramedullary enhancement in the anterior horn on the affected side.9, 10 Ito et al.11 reported that both the anterior horns and ventral nerve roots are compromised by paramedian compression in CSA. Shinomiya et al.12 proposed a nerve root lesion or intrinsic cord lesion as a cause of proximal-type CSA, on the basis of findings of neuroradiological and electrophysiological assessment. Fujiwara et al.13 reported, on the basis of the surgical outcome of posterior decompression, that CSA was caused by impingement of either the anterior horn of the spinal cord or ventral nerve root, although some patients had impingement of both the anterior horn and ventral nerve root.
The diagnosis of CSA is generally based on clinical presentation, disease course, physical examination, neuroimaging findings, electrophysiological findings and the exclusion of other disorders that might cause similar clinical features. The clinical feature of CSA, including muscle atrophy and fasciculation of the upper extremities, resembles motor neuron diseases such as amyotrophic lateral sclerosis (ALS) and progressive spinal muscular atrophy. In particular, differentiation of CSA from early-stage ALS may be difficult. Bulbar muscle involvement obviously suggests ALS, and the clinical manifestations of ALS are diffuse and progressive. About half of the patients with progressive spinal muscular atrophy show a symmetric wasting away of intrinsic hand muscles, slowly advancing to the more proximal parts of the arm.14 On the other hand, CSA is characterized by muscle weakness and wasting away of the upper extremities that does not progress beyond a few myotomes, and that usually stabilizes for years after an initially progressive course.9, 12, 15, 16 In addition, findings of electromyography are observed only in the atrophic muscles in case of CSA, but are diffuse in patients with ALS.15 An important factor favoring CSA is the lack of bulbar muscle involvement and the non-progressive nature of motor symptoms and signs that are restricted to a few myotomes.
The treatment of CSA remains controversial. Surgical treatment has included anterior cervical decompression and fusion or posterior decompression (laminoplasty with or without foraminotomy). Shinomiya et al.12 reported 10 CSA patients treated by anterior cervical decompression with good outcomes. Mori et al.15 reported that anterior surgical intervention is effective in patients with CSA unless MRI reveals the presence of a severe degenerative intramedullary lesion. Srinivasa et al.17 reported a good outcome for patients with distal CSA managed by central corpectomy, and considered a ventral decompression procedure such as central corpectomy to be ideal, as the spinal cord is involved. Fujiwara et al.13 reported that laminoplasty and foraminotomy were effective in treating most patients for CSA, with excellent or good results in 78% of cases. Sasai et al.18 reported that microsurgical posterior foraminotomy combined with laminoplasty is a beneficial treatment option, with improvement of deltoid muscle strength in approximately 80% of CSA cases.
On the other hand, there have been a few reports of conservative treatment with successful recovery. Kameyama et al.9 reported three cases of CSA treated by immobilization of the neck with improvement of motor symptoms and stabilization, and suggested that a pathophysiological basis of this syndrome may be multisegmental injury of the anterior horns caused by dynamic cord compression through circulatory insufficiency. Shibuya et al.16 observed motor recovery in three patients with CSA who received prostaglandin E1 treatment, and suggested that patients with anterior spinal artery syndrome might have been included among those diagnosed with CSA.
HBO, which is widely performed for patients in hypoxic condition, is an attractive method of treatment that has frequently been used for several neurological diseases.3, 4, 5, 6, 7 HBO therapy has been shown to decrease tissue edema, improve blood flow, and promote oxygen delivery, leading to an increase in the oxygen level in neuronal tissues and enhancement of cellular and metabolic functions.8 Arterial oxygen pressure and content were increased after HBO treatment, with a 20% improvement of oxygen supply to the ischemic periphery.19 Increased oxygen supply to the ischemic penumbra may result in improvement of energy failure in compromised tissue and reduce susceptibility to spreading depression.20 HBO therapy has also been clinically reported to promote neurological recovery after spinal cord injury or surgical treatment of cervical myelopathy.6, 7 We believe that HBO might facilitate the recovery of reversibly injured cells by improving the hypoxic condition of neural tissue at risk, though it has no effect on the recovery of irreversibly injured cells. In the CSA patients of the present study, we speculate that oxygen supply to reversibly injured anterior horn cells under hypoxic conditions by HBO treatment might result in improvement of energy failure and subsequent reinnervation of the atrophic muscles, leading to improvement of muscle strength.
Conclusion
To our knowledge, conservative treatment with HBO therapy for CSA patients has not previously been described. We believe that HBO therapy might improve ischemic injury of the anterior horns in CSA patients with short duration of symptoms. Although assessment of a larger number of cases is needed to evaluate the effectiveness of HBO therapy, the findings of the present case series suggest that conservative treatment with HBO therapy might be a useful treatment option before surgery for CSA patients with short duration of symptoms.
References
Keegan JJ . The cause of dissociated motor loss in the upper extremity with cervical spondylosis. J Neurosurg 1965; 23: 528–536.
Yanagi T, Kato H, Sobue I . Clinical characteristics of cervical spondylotic amyotrophy. Rinsho Shinkeigaku 1976; 16: 520–528.
Nighoghossian N, Trouillas P, Adeleine P, Salord F . Hyperbaric oxygen in the treatment of acute ischemic stroke. A double-blind pilot study. Stroke 1995; 26: 1369–1372.
Papazian O, Alfonso I . Hyperbaric oxygen treatment for children with cerebral palsy. Rev Neurol 2003; 37: 359–364.
Golden ZL, Neubauer R, Golden CJ, Greene L, Marsh J, Mleko A . Improvement in cerebral metabolism in chronic brain injury after hyperbaric oxygen therapy. Int J Neurosci 2002; 112: 119–131.
Asamoto S, Sugiyama H, Doi H, Iida M, Nagao T, Matsumoto K . Hyperbaric oxygen (HBO) therapy for acute traumatic cervical spinal cord injury. Spinal Cord 2000; 38: 538–540.
Ishihara H, Matsui H, Kitagawa H, Yonezawa T, Tsuji H . Prediction of the surgical outcome for the treatment of cervical myelopathy by using hyperbaric oxygen therapy. Spinal Cord 1997; 35: 763–767.
Al-Waili NS, Butler GJ, Beale J, Abdullah MS, Hamilton RW, Lee BY et al. Hyperbaric oxygen in the treatment of patients with cerebral stroke, brain trauma, and neurologic disease. Adv Ther 2005; 22: 659–678.
Kameyama T, Ando T, Yanagi T, Yasui K, Sobue G . Cervical spondylotic amyotrophy. Magnetic resonance imaging demonstration of intrinsic cord pathology. Spine 1998; 23: 448–452.
Fujiwara K . Cervical spondylotic amyotrophy with intramedullary cavity formation. Spine 2001; 26: E220–E222.
Ito T, Tsuji H, Tamaki T, Miyasaka H, Toyoda A . The clinical consideration of the dissociated motor loss syndrome (Keegan) in diseases of the cervical spine. Nippon Seikeigeka Gakkai Zasshi 1980; 54: 135–151.
Shinomiya K, Komori H, Matsuoka T, Mutoh N, Furuya K . Neuroradiologic and electrophysiologic assessment of cervical spondylotic amyotrophy. Spine 1994; 19: 21–25.
Fujiwara Y, Tanaka N, Fujimoto Y, Nakanishi K, Kamei N, Ochi M . Surgical outcome of posterior decompression for cervical spondylosis with unilateral upper extremity amyotrophy. Spine 2006; 31: E728–E732.
Sasaki S, Iwata M . Atypical form of amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 1999; 66: 581–585.
Mori K, Yamamoto T, Nakao Y, Maeda M . Cervical spondylotic amyotrophy treated by anterior decompression. Three case reports. Neurol Med Chir (Tokyo) 2006; 46: 366–370.
Shibuya R, Yonenobu K, Yamamoto K, Kuratsu S, Kanazawa M, Onoue K et al. Acute arm paresis with cervical spondylosis: three case reports. Surg Neurol 2005; 63: 220–228.
Srinivasa Rao NV, Rajshekhar V . Distal-type cervical spondylotic amyotrophy: incidence and outcome after central corpectomy. J Neurosurg Spine 2009; 10: 374–379.
Sasai K, Umeda M, Saito T, Ohnari H, Wakabayashi E, Iida H . Microsurgical posterior foraminotomy with laminoplasty for cervical spondylotic radiculomyelopathy including cervical spondylotic amyotrophy. J Neurosurg Spine 2006; 5: 126–132.
Sunami K, Takeda Y, Hashimoto M, Hirakawa M . Hyperbaric oxygen reduces infarct volume in rats by increasing oxygen supply to the ischemic periphery. Crit Care Med 2000; 28: 2831–2836.
Hossmann KA . Viability thresholds and the penumbra of focal ischemia. Ann Neurol 1994; 36: 557–565.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tofuku, K., Koga, H., Yone, K. et al. Conservative treatment with hyperbaric oxygen therapy for cervical spondylotic amyotrophy. Spinal Cord 49, 749–753 (2011). https://doi.org/10.1038/sc.2010.185
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.185
Keywords
This article is cited by
-
Effects of hyperbaric oxygen therapy on postoperative recovery after incomplete cervical spinal cord injury
Spinal Cord (2022)
-
Cervical spondylotic amyotrophy: a systematic review
European Spine Journal (2019)