Abstract
Study design:
An in vivo study in a rat model of acute spinal cord contusion.
Objectives:
To assess the efficacy of novel therapies for acute spinal cord injury (SCI), methods to evaluate accurately the effects of these therapies should be developed. Although neurological examination is commonly used for this purpose, unstable clinical conditions and the spontaneous recovery of neurological function in the acute and subacute phases after injury make this measurement unreliable. Recent studies have reported that the phosphorylated form of the high-molecular-weight neurofilament subunit NF-H (pNF-H), a new biomarker for axonal degeneration, can be measured in serum samples in experimental SCI animals. Therefore, we aimed to investigate the use of plasma pNF-H as an indicator of the efficacy of minocycline, a neuroprotective drug, for treating SCI.
Setting:
This study was carried out at Saitama, Japan.
Methods:
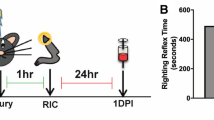
Spinal cord injured rats received either minocycline or saline intraperitoneally. The plasma pNF-H levels and functional hind limb score were determined after the injury.
Results:
Minocycline treatment reduced plasma pNF-H levels at 3 and 4 days post-injury (dpi). Rats with lower plasma pNF-H levels at 3 dpi had higher hind limb motor score at 28 dpi.
Conclusions:
pNF-H levels may serve as a biomarker for evaluating the efficacy of therapies for SCI.
Similar content being viewed by others
Introduction
The sensorimotor dysfunction that occurs after spinal cord injury (SCI) results from both the primary mechanical insult and secondary damage, which includes multiple components such as inflammatory reaction, delayed neuronal and glial cell death, and axonal degeneration.1, 2 These biological processes continue for several days, and can therefore be targeted in therapeutic intervention. Various therapeutic strategies have been developed to ameliorate tissue loss arising due to secondary damage.3
Appropriate assessment methods are required to determine the efficacy of novel neuroprotective therapies. The American Spinal Injury Association assessment scale is a standardized tool that is used widely to assess neurological state (grade A–E) and motor score in SCI patients. However, the spontaneous neurological recovery in acute and subacute SCI patients may limit the reliability of assessments of the initial state.4 Further, as the degree of spontaneous recovery varies among patients in clinical trials of SCI therapies, it is unclear whether the neurological improvement is because of the therapeutic intervention or spontaneous recovery. Therefore, a novel technique that is independent of neurological status is required for monitoring progressive tissue damage; this development will facilitate further clinical trials of SCI therapies.
The severity or stage of a disease is usually determined by measuring the levels of certain biomarkers in blood or cerebrospinal fluid. In the clinical field of traumatic brain injury, several proteins that are synthesized in neurons and glial cells, such as S100B, neuron-specific enolase, myelin basic protein and glial fibrillary acid protein, have been proposed as surrogate markers that can be used in clinical trials.5, 6 However, there are only a few reports on biomarkers in SCI patients.7, 8
Recently, studies in experimental SCI animals and aneurismal subarachnoid hemorrhage patients revealed an association between the level of the phosphorylated form of the high-molecular-weight neurofilament subunit NF-H (pNF-H) in blood and prognosis.9, 10 Because NF-H is one of the major structural complexes in axons, increased levels of the phosphorylated form of the protein, which is resistant to proteases, indicate increased axonal damage. In contrast to the other neural-cell-derived biomarkers such as serum S100B and neuron-specific enolase, whose levels peak within 24 h after injury, serum pNF-H levels peak 3 days after SCI.9, 11 This temporal pattern may reflect progressive axonal loss due to secondary damage. A previous study in experimental SCI rats reported a relation between the serum pNF-H level and the intensity of the initial impact (primary insults) delivered by the SCI device.9 However, whether pNF-H can be used as a marker to evaluate the efficacy of therapeutic interventions against secondary damage in SCI remains unknown. In this study, we measured the plasma pNF-H levels in SCI rats treated with minocycline, a neuroprotective drug.3, 12, 13
Materials and methods
Surgical procedures
All surgical procedures were approved by the ethical committee of Research Institute, National Rehabilitation Center. Experimental SCIs were induced in adult 10- to 12-week-old Sprague–Dawley rats (body weight, 280–320 g). Animals were anesthetized by intraperitoneal injection of barbiturate. Thereafter, the lower thoracic lamina was exposed, and the lamina was removed at the level of Th10. Contusion injuries were then induced by using the Infinite Horizon SCI device (Precision Systems and Instrumentation, Lexington, KY, USA). The intensity of the device was set to 1.5 N (150 kdyn), which induces moderate contusion injury. After the surgical procedure, the rats were allowed to recover on a warm blanket. From the day after the surgery, urination was assisted manually until voluntary urination was restored.
Minocycline treatment
Rats were randomly assigned into two groups (N=4 per group) and were administered an intraperitoneal injection of either control saline (control group) or minocycline (15 mg ml−1 in saline; treated group) (Sigma, St Louis, MO, USA). The injured rats received an initial dose of 90 mg kg−1 body weight minocycline immediately after the injury, followed 9 h later by a second dose of 45 mg kg−1 body weight. From the following day, either control saline or 45 mg kg−1 body weight minocycline was administered twice a day up to 3 days post injury (dpi).12, 14
To evaluate the motor recovery, animals were observed by one individual masked to the treatments on 1, 3, 7, 14, 21 and 28 dpi. Lower limb functions were assessed by the Basso, Beattie and Bresnahan scale.15
Measurement of blood pNF-H levels
Blood samples were taken from the tail vein of the injured rats on 1, 2, 3, and 4 dpi. The blood samples were anticoagulated using ethylenediamine tetraacetic acid and centrifuged at 3000 r.p.m. for 10 min to obtain plasma. The plasma samples were frozen and stored until the pNF-H assay was performed. The pNF-H assay was carried out using a commercially available enzyme-linked immunosorbent assay kit (ELISA-pNF-H; EnCor Biotechnology, Gainesville, FL, USA). The frozen plasma samples were allowed to thaw, and then diluted 1/5 with a dilution buffer. The samples were then loaded onto an enzyme-linked immunosorbent assay plate. The assay was performed according to the manufacturer’s protocol. To standardize the pNF-H value, we divided the absolute pNF-H concentration by the total protein concentration of each sample.
Statistical analysis
The hind limb function score was analyzed by the Mann–Whitney U-test. Quantitative plasma pNF-H values between the two groups were analyzed by repeated-measure analysis of variance. The relation between plasma pNF-H levels and hind limb function score was assessed by determining the Spearman’s rank correlation coefficient. Error bars indicate the standard error, and differences with a P-value of <0.05 were considered statistically significant.
We certify that all applicable institutional and governmental regulations concerning the ethical use of animals were followed during the course of this research.
Results
Minocycline improves hind limb motor function after incomplete spinal cord injury
To determine whether plasma pNF-H levels can be used as a marker for evaluating the efficacy of neuroprotective therapies for SCI, we analyzed the plasma pNF-H levels in experimental SCI rats treated with minocycline, a drug with proven neuroprotective effects.3, 12, 13, 14 As minocycline is known to prevent secondary damage in neural tissue by inhibiting microglial activation,3, 12 we assumed that the administration of this drug may also reduce biomarkers of tissue damage.
First, we confirmed the efficacy of minocycline treatment. Behavioral assessments at 28 dpi (Figure 1) revealed that minocycline-treated rats had better hind limb motor function than did the control rats (mean Basso, Beattie and Bresnahan score±standard error of the mean (s.e.m.): treated group, 14.5±0.6 vs control group, 12.4±0.4; P<0.05). The better hind limb function observed in the treated rats suggests that minocycline exerted neuroprotective effects after SCI in this rat model.
The functional recovery of hind limbs after spinal cord injury in both the treated and control groups. Thoracic spinal cord injured rats were treated with either minocycline (treated group: mino) or saline (control group: ctrl). The Basso, Beattie and Bresnahan (BBB) scale was used to assess the motor function of the hind limbs of the injured rats. At 28 dpi, the treated group showed better motor function, and the difference between the two groups was statistically significant (values are shown as mean±standard error of the mean; *P<0.05).
Minocycline treatment modulates plasma pNF-H levels
Because minocycline reduces axonal damage in the injured spinal cord by preventing secondary damage, we assumed that the plasma pNF-H level in the treated group would be lower than that in the control group. The plasma pNF-H level and pNF-H/total protein ratio were determined from the blood samples (Figure 2). In both the groups, pNF-H was detected from 1 dpi and its levels peaked at 3 dpi; however, the pNF-H level at 3 dpi was lower in the treated group than in the control group (treated group, 0.088±0.018 μg g−1; control group, 0.112±0.011 μg g−1). Although this difference was not statistically significant (repeated-measure analysis of variance; P=0.27), the same trend was observed at 4 dpi. The reduction in the plasma pNF-H levels at 3 and 4 dpi may indicate the protective effects of minocycline against axonal damage in the treated group.
Changes in plasma pNF-H levels induced by minocycline treatment. The levels of plasma pNF-H in serial samples obtained from injured rats in both the treated (mino) and control (ctrl) groups were analyzed by an enzyme-linked immunosorbent assay. The absolute pNF-H values were divided by the total protein concentration of each sample (values are shown as mean±standard error of the mean). Even though the pNF-H level in the treated group was lower than that in the control group at 3 and 4 dpi, the difference was not statistically significant.
Plasma pNF-H levels at 3 dpi correlate with locomotor function recovery
As the plasma pNF-H level at 3 dpi was lower in the treated group than in the control group, we next examined whether the pNF-H level at 3 dpi can serve as a predictor of the recovery of hind limb function. Figure 3 shows a plot of the plasma pNF-H level (3 dpi) and hind limb motor score (28 dpi) for each rat in both groups. Statistical analysis revealed a negative correlation between these two parameters (Spearman’s rank correlation coefficient: rs=−0.78; P<0.05), indicating that a subject with a low pNF-H level is more likely to achieve a higher motor score at 28 dpi.
Correlation between plasma pNF-H level and recovery of hind limb function after spinal cord injury. The plasma pNF-H concentration at 3 dpi was plotted against the hind limb functional score at 28 dpi for each sample (both the treated and control groups). The regression line indicates a negative correlation between these two parameters.
Discussion
This study is the first to assess whether blood pNF-H levels reflect the neuroprotective effects of minocycline against SCI. We found that minocycline treatment reduced plasma pNF-H levels at 3 dpi, and this reduction was correlated with the functional motor score; this finding is consistent with the reported neuroprotective effects of the drug. Therefore, we suggest that plasma pNF-H levels can serve as a biomarker, to some extent, for monitoring the amelioration of tissue damage by SCI treatments.
We observed a reduction in plasma pNF-H levels in the treated group at 3 dpi, but the difference between the two groups was not statistically significant. This marginal reduction in the pNF-H level could be caused by either a minimal protective effect on the axons induced by minocycline or a timing error in blood sample collection. Most of the studies on minocycline treatment for SCI describe the difference in the histological findings between the treatment and control groups at 7 or 14 dpi.3 The plasma pNF-H level decreased after 3 dpi, and this finding was consistent with other reports.9 Further, we speculate that the pNF-H level at later time points would be influenced by restoration of the blood–brain barrier. Therefore, the comparison of the pNF-H levels at 7 or 14 dpi would not be feasible for evaluating the neuroprotective effect of therapeutic interventions. On the basis of these findings, we consider that blood pNF-H levels would best reflect the effects of neuroprotective drugs if the drugs exert their function within 3 days after SCI.
The association between serum pNF-H levels and prognosis has already been reported in studies with subarachnoid hemorrhage and amyotrophic lateral sclerosis patients.10, 16 To determine the utility of pNF-H as biomarker of clinical SCI, further studies with patients with varying degrees of SCI are required. Taking such biomarkers in clinical trials may reduce the number of the patients required, which accelerates the development of novel therapeutic approaches against the traumatic disorder.
References
McDonald JW, Sadowsky C . Spinal-cord injury. Lancet 2002; 359: 417–425.
Crowe MJ, Bresnahan JC, Shuman SL, Masters JN, Beattie MS . Apoptosis and delayed degeneration after spinal cord injury in rats and monkeys. Nat Med 1997; 3: 73–76.
Stirling DP, Khodarahmi K, Liu J, McPhail LT, McBride CB, Steeves JD et al. Minocycline treatment reduces delayed oligodendrocyte death, attenuates axonal dieback, and improves functional outcome after spinal cord injury. J Neurosci 2004; 24: 2182–2190.
Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord 2007; 45: 190–205.
Honda M, Tsuruta R, Kaneko T, Kasaoka S, Yagi T, Todani M et al. Serum glial fibrillary acidic protein is a highly specific biomarker for traumatic brain injury in humans compared with S-100B and neuron-specific enolase. J Trauma 2010; 69: 104–109.
Berger RP, Beers SR, Richichi R, Wiesman D, Adelson PD . Serum biomarker concentrations and outcome after pediatric traumatic brain injury. J Neurotrauma 2007; 24: 1793–1801.
Marquardt G, Setzer M, Szelenyi A, Seifert V, Gerlach R . Significance of serial S100b and NSE serum measurements in surgically treated patients with spondylotic cervical myelopathy. Acta Neurochir (Wien) 2009; 151: 1439–1443.
Pouw MH, Hosman AJ, van Middendorp JJ, Verbeek MM, Vos PE, van de Meent H . Biomarkers in spinal cord injury. Spinal Cord 2009; 47: 519–525.
Shaw G, Yang C, Ellis R, Anderson K, Parker Mickle J, Scheff S et al. Hyperphosphorylated neurofilament NF-H is a serum biomarker of axonal injury. Biochem Biophys Res Commun 2005; 336: 1268–1277.
Lewis SB, Wolper RA, Miralia L, Yang C, Shaw G . Detection of phosphorylated NF-H in the cerebrospinal fluid and blood of aneurysmal subarachnoid hemorrhage patients. J Cereb Blood Flow Metab 2008; 28: 1261–1271.
Loy DN, Sroufe AE, Pelt JL, Burke DA, Cao QL, Talbott JF et al. Serum biomarkers for experimental acute spinal cord injury: rapid elevation of neuron-specific enolase and S-100beta. Neurosurgery 2005; 56: 391–397; discussion 391–397.
Yune TY, Lee JY, Jung GY, Kim SJ, Jiang MH, Kim YC et al. Minocycline alleviates death of oligodendrocytes by inhibiting pro-nerve growth factor production in microglia after spinal cord injury. J Neurosci 2007; 27: 7751–7761.
Pinzon A, Marcillo A, Quintana A, Stamler S, Bunge MB, Bramlett HM et al. A re-assessment of minocycline as a neuroprotective agent in a rat spinal cord contusion model. Brain Res 2008; 1243: 146–151.
Lee SM, Yune TY, Kim SJ, Park DW, Lee YK, Kim YC et al. Minocycline reduces cell death and improves functional recovery after traumatic spinal cord injury in the rat. J Neurotrauma 2003; 20: 1017–1027.
Basso DM, Beattie MS, Bresnahan JC . A sensitive and reliable locomotor rating scale for open field testing in rats. J Neurotrauma 1995; 12: 1–21.
Boylan K, Yang C, Crook J, Overstreet K, Heckman M, Wang Y et al. Immunoreactivity of the phosphorylated axonal neurofilament H subunit (pNF-H) in blood of ALS model rodents and ALS patients: evaluation of blood pNF-H as a potential ALS biomarker. J Neurochem 2009; 111: 1182–1191.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ueno, T., Ohori, Y., Ito, J. et al. Hyperphosphorylated neurofilament NF-H as a biomarker of the efficacy of minocycline therapy for spinal cord injury. Spinal Cord 49, 333–336 (2011). https://doi.org/10.1038/sc.2010.116
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.116
Keywords
This article is cited by
-
The developing landscape of diagnostic and prognostic biomarkers for spinal cord injury in cerebrospinal fluid and blood
Spinal Cord (2017)
-
Topography and Morphometric Characteristics of NF200+ Neurons in the Gray Matter of the Spinal Cord after Capsaicin Deafferentation
Neuroscience and Behavioral Physiology (2014)
-
Phosphorylated neurofilament subunit NF-H as a biomarker for evaluating the severity of spinal cord injury patients, a pilot study
Spinal Cord (2012)