Abstract
Study design:
Cross-sectional study.
Objectives:
To quantify three-dimensional (3D) reachable workspace in different groups of tetraplegic participants and to assess their reaching performance within this workspace.
Setting:
Northwest Regional Spinal Injuries Centre, UK.
Methods:
The 3D reachable workspace of three groups of tetraplegics (NON-OP, operated group (OP) and tetraplegic control group (CONTetraplegic) with varying levels of triceps function together with a healthy control group (CONHealthy)) was defined by reaching to five target positions (anterior, medial, lateral, superior and inferior) located on the periphery of their workspace. Joint angles and inter-joint co-ordination were analysed after a 3D reconstruction of the thorax, humerus and forearm. The performance related variables of movement time, peak velocity, time-to-peak velocity and curvature index were also examined.
Results:
The reachable volumes covered were consistent with the level of triceps function as CONHealthy covered a significantly greater volume than the tetraplegic groups and in turn the OP covered a larger workspace volume than NON-OP. The reduced workspace of tetraplegics was identified as being due to restrictions in workspace above shoulder height and across the body. Co-ordination data identified some differences in movement patterns but when reaching to targets on the workspace there were no significant differences between the OP and NON-OP groups.
Conclusion:
This study provided a detailed assessment of reachable workspace and target reaching. Tetraplegic participants found the superior and medial parts of the workspace were the most challenging directions. Standardised biomechanical analysis of tetraplegic upper-limb function is required for objective assessment.
Similar content being viewed by others
Introduction
Tendon transfer surgery is appropriate for tetraplegic individuals with a complete spinal cord lesion at the C5–C6 vertebral level, as paralysis of the triceps brachii muscle leaves them unable to actively extend the elbow. To restore elbow extension, Moberg1 suggested that the functionally expendable posterior deltoid muscle could be transferred to the triceps brachii tendon. This technique has since become commonplace and the success of the surgery is typically evaluated using questionnaires1, 2, 3 or by timing functional tasks.4, 5 Recently, three-dimensional (3D) motion analysis has emerged as a way to provide clinicians with additional objective information, which can be used to evaluate movement strategies and adaptive mechanisms after a tendon transfer.
Research using 3D motion analysis has examined the effect of the tendon transfer in tetraplegic individuals performing pointing6, 7, 8 and daily living activities.9 Although such tasks provide insight into altered movement control strategies and functional capabilities, the change in reachable workspace is unknown. Reachable workspace describes the volume within which an individual can reach and it is important in the objective assessment and rehabilitation of patients with upper-limb pathology.10 Clinical observation would suggest tendon transfer surgery increases reachable workspace but the extent and location of any increase is untested.
Reachable workspace provides a simple objective assessment measure but on its own it is insufficient to examine changes in patient function.11 Previous studies suggest that after tendon transfer tetraplegics can co-ordinate their arms similarly to healthy individuals but this has only been shown during two functional tasks9 or toward targets placed on a table.6, 7 Analysis of reaching within an individual's 3D workspace would allow tetraplegic patients’ unconstrained reaching ability to be fully and objectively evaluated. Considering this, the aims of this study were to quantify 3D reachable workspace in different groups of tetraplegic participants and to assess their reaching performance within this workspace.
Materials and methods
Participants
Eleven C5–C6 tetraplegic individuals and seven neurologically unimpaired individuals volunteered for this study. All tetraplegic participants were a minimum of 1 year post-injury and where applicable, 1 year post-surgery having completed a full rehabilitation programme. Tetraplegic participants were grouped according to their triceps brachii function (Table 1). Both arms were used for three tetraplegic participants. Eight arms had undergone a posterior deltoid to triceps tendon transfer operation (OP). Four arms had no active triceps contraction and had not undergone a tendon transfer operation (NON-OP). Two control groups were used; the tetraplegic control group (CONTetraplegic) contained three arms with full triceps activity and seven able-bodied participants formed the healthy control group (CONHealthy). The tendon transfer operation was performed by mobilising the posterior deltoid and anastomosis this to the triceps and olecranon process. The interface between the posterior deltoid and triceps was created by harvesting the tibialis anterior tendon and the anastomosis was reinforced by wrapping it with Mersilene mesh.
The tibialis anterior tendon was secured to the triceps by attaching a length of Mersilene mesh to the end of the tibialis anterior tendon. It was then zigzagged through the aponeurosis of the triceps, passed through a hole in the olecranon process and then zigzagged back. The operated limb was immobilised with the elbow in extension for 4 weeks post-surgery.
Upper extremity model
Three-dimensional movement analysis was undertaken using an eight camera opto-electronic system (Qualisys, Gothenburg, Sweden) sampling at 120 Hz. Anatomical co-ordinate systems were defined for the thorax, humerus and forearm using 18 retro-reflective markers in a 1-s static trial. To indicate the end of the hand, a marker attached to a plastic wand was positioned over the most distal phalanx of the middle finger. The thorax was defined anatomically using markers on the left and right acromion processes, sternum and left and right anterior superior iliac spines. The humerus was defined anatomically using the glenohumeral joint centre and markers on the medial and lateral epicondyles. The glenohumeral joint centre was calculated in Visual 3D v.3.90.21 (C-Motion, Germantown, MD, USA) using the method described by Schwartz and Rozumalski12 and the protocol of Begon et al.13 The forearm was defined anatomically using the distal humerus and the radial and ulna styloid processes. The dynamic movement of the humerus and forearm was tracked using two technical clusters of four markers each. During dynamic trials the acromion, elbow and wrist markers were removed. Relative motion between segments was expressed using Euler angles (Figure 1). The ISB recommended Cardan sequences were used for the humerus relative to the thorax (Y–X–Y) and the forearm relative to the humerus (X–Y–Z).14
3D wosrkspace and reaching targets
Each individual defined their 3D workspace by moving their arm through their full hemispheric range of motion. They started by reaching from the sternum to their extreme workspace and continued to move the plastic wand through their workspace for 60 s. Trunk movement was minimised by a chest strap and verbal guidance was provided to ensure that all reachable areas of the workspace were covered. Reachable volume was calculated in Matlab (v.7.4.0287, The MathWorks Inc., Natick, MA, USA) using the Quickhull algorithm.15 Delaunay triangulation was used to create a convex hull of the workspace and then reachable volume was calculated by measuring the volume of the intersection of the halfspaces defined by each facet of the convex hull. Reachable volume was then expressed as a percentage relative to a hemisphere of radius one arm length (the distance from the glenohumeral joint centre to the elbow joint centre added to the distance from the elbow joint centre to the marker on the plastic wand).
To further characterise each participant's workspace, a custom written Matlab programme identified five targets (anterior, medial, lateral, superior and inferior) on each individual's workspace surface. Each target was the furthest point the pointer trajectory had reached in the specified direction (Figure 2). A reflective marker was positioned at each target location but at 105% of arm length to make the physical target just out of reach. Each participant performed a minimum of eight reaches to each target location at a self-determined pace. The start position of the reaching hand was the sternum. All patients were seated in their own wheelchairs and the CONHealthy group sat on a similar chair.
An example of how a 60-s pointer marker trajectory was used to define a workspace and then subsequent target locations. The black rings on the periphery of the workspace represent the identified targets that this individual would reach toward. The axes are scaled to one arm length with 0, 0 being the glenohumeral joint centre.
Data processing
All marker trajectories were low-pass filtered (Butterworth fourth-order zero-lag) at 10 Hz. When appropriate, data collected from left arms were mathematically mirrored to match the right arm data. Range of motion was the absolute value of the change in joint angle during movement time. Movement time began when the velocity of the pointer marker exceeded 0.05 m s–1 and ended when the velocity of the difference between the pointer and target markers was below 0.05 m s –1. Kinematic data were normalised to 101 points and then averaged over individual trials. For a comparison between groups, ‘movement time’, ‘peak velocity’ and ‘time-to-peak velocity’ were quantified along with the ‘curvature index’, which was defined as the ratio of the cumulative distance travelled by the pointer marker between the start and end position and the Euclidean distance.6
Statistical analyses
Statistical procedures were undertaken using SPSS v.14 (SPSS Inc., Chicago, IL, USA) using an alpha level of α=0.05. Differences in relative reachable volume were examined using a Kruskal–Wallis test (H-statistic) with post hoc Mann–Whitney U-tests with Bonferroni correction.
Peak velocity and time-to-peak velocity data were parametric and were tested using the mixed design analysis of variance (F-statistic) with post hoc Bonferroni correction. Movement time and curvature index were analysed using non-parametric statistics. Within-subject effects were examined using Friedman's analysis of variance (χ2 statistic) and Wilcoxon signed-ranks tests with Bonferroni correction. Between-subject effects were assessed with the Kruskal–Wallis test and Mann–Whitney U-tests.
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Reach volume
There was a significant main effect for reachable volume H3=16.73, P<0.05. The CONHealthy group (90.9±9.2%) had the greatest reachable volume, which was significantly greater than the CONTetraplegic (74.9±3.9%), OP (61.5±17.2%) and NON-OP (47.2±23.5%) groups. The CONTetraplegic, NON-OP and OP groups were not significantly different.
Target locations and range of motion
To account more specifically for the reductions in volume shown by the tetraplegic participants, the target locations were compared (Table 2). The OP and NON-OP tetraplegic groups were less capable of reaching to full arm length in the directions of the medial and superior targets. In comparison, the anterior, lateral and inferior targets could be reached by all the tetraplegic groups as well as the CONHealthy group (Figure 3). These data, therefore, show an uneven reduction in the volume across the targets.
The largest range of motion differences observed between the NON-OP and OP groups came when reaching to the medial and superior targets. Reaching across the body to the medial target required a large plane of humeral elevation angle and the least elbow extension (Table 3). The NON-OP and OP groups had a reduced plane of humeral elevation angle and reduced elbow extension, which shifted their medial targets to a more anterior location. The OP group could reach further across and closer to their body than NON-OP as indicated by the mean medial target location in Figure 3.
A lack of humeral elevation in the tetraplegic participants (Table 3) caused a lower vertical position of the superior target (Figure 3) compared with the CONHealthy group. The NON-OP group had 17.2° less elbow extension and 28.9° less humeral elevation than OP (Table 3), which meant that their superior target was in a more anterior location (Figure 3). The anterior position of the superior target, however, was the most variable co-ordinate.
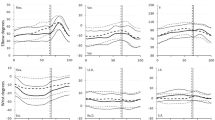
Co-ordination
The NON-OP and OP groups both elevated the humerus in the starting position when reaching the anterior target (Figure 4). This allowed some tetraplegic participants from the OP group to reach to the anterior target by maintaining the humeral elevation angle and only extending the elbow. This therefore makes their co-ordination profile purely horizontal in Figure 4. All tetraplegic participants preferred to start their reaching with a more retracted humerus compared with the CONHealthy group causing a greater range of motion in the plane of humeral elevation.
One NON-OP tetraplegic participant had to decrease the humeral elevation angle, presumably to allow gravity and the inertia of the lower arm to extend the elbow when reaching to the anterior target (Figure 4a). This strategy contrasted with all other tetraplegics who further elevated the humerus from the starting position.
To reach the superior target some of the NON-OP and OP participants required further adjustment of the humeral elevation angle after they had fully extended the elbow. This adjustment is illustrated in Figures 5a and b by a sharp curve toward the end of the movement range. The NON-OP group's lateral target was more anteriorly and inferiorly positioned. A lack of complete elbow extension meant that both the NON-OP and OP groups required a negative plane of elevation to reach this target (Figure 6).
Kinematic data
As shown in previous studies,6 there were few differences in descriptive variables between tetraplegic participants. From statistical analysis (Table 4) no significant differences were found between NON-OP and OP for movement time, peak velocity, time-to-peak velocity and curvature index. Significant within-subject effects were found for movement time, curvature index and peak velocity. All groups took significantly more time when reaching to the superior target. The anterior target had the lowest curvature index and the inferior target had the greatest.
Discussion
Comparison between the NON-OP and OP groups would suggest that the tendon transfer has a beneficial effect during reaching because of the better performance by the OP group for reachable volume, target location and joint co-ordination. Strong support although, has not been found and this is the consequence of using a cross-sectional study with low participant numbers and high variability because of differing ages and the individuality of patients’ lesion and surgery. To further quantify the re-learning and adaptation to the transfer, longitudinal studies are required but the challenge with collecting such information is to have sufficiently sensitive assessment techniques to detect the subtle process of movement re-learning. 3D motion analysis provides such a technique.
This study found differences in the magnitude and shape of the reachable workspace in the different groups tested. Smaller reachable volumes in the NON-OP and OP groups were caused by a reduced range of motion when reaching superiorly and medially. In the CONTetraplegic group, the reduction in workspace in the superior direction was primarily caused by reduced humeral elevation whereas in the NON-OP and OP groups it was both reduced humeral elevation and elbow extension that reduced workspace height. The tendon transfer restores active elbow extension but provides only 20% of normal triceps force16 and so may therefore not provide the strength required to position the arm at the extreme workspace. This would support our previous work,17 which showed reductions in workspace of 14% when a 1-kg resistance was applied to the wrist and it also highlights the weakness still present that prevents some post-surgery tetraplegics performing weight-relief manoeuvres. The reduction in range of motion to the medial target was predominantly determined by the plane of elevation angle. As humeral adduction is primarily performed by the pectoralis major, injury at C6 or above will especially impair the sternocostal head—the predominant humeral adductor. As the spinal roots of the pectoral nerves are from C5 to T1, the exact location of the lesion will determine the precise function of the pectoralis major.
All tetraplegic groups showed similar kinematic characteristics to the CONHealthy group when reaching to the anterior, lateral and inferior targets at the workspace periphery. This supports the data from previous pointing studies6, 7 but as they do not include reaching at or below shoulder height, they are insufficient to fully evaluate a patient's arm function. Reaches at these heights should be considered when undertaking assessment of tetraplegic participants clinically or experimentally in the future.
Remy-Neris et al.9 showed the improvement in co-ordination shown by post-tendon transfer tetraplegics during two arm raising tasks. After 16 months, the tetraplegic participants in their study had comparable range of motion and angular velocity to healthy control participants. The minimum post-surgery recovery of 2 years used in this study appears sufficient time for the OP group to improve range of motion but whilst some participants’ co-ordination mirrored that of the control groups, others were more similar to the NON-OP group. Generalised analysis across groups seems to mask the individuality of patients’ responses and adaptation to surgery.
As this study established the workspace in which tetraplegic patients can reach and the ability of tetraplegics to reach to this workspace, this study coupled with data from functional tasks9 and movement control6 has provided a greater understanding of the functional benefits of the tendon transfer. Future studies using EMG within the workspace would allow researchers to examine how the central nervous system adapts to the tendon transfer and activates the upper-limb muscles to reach effectively.
In conclusion, this study objectively quantified tetraplegic reachable workspace and used this workspace to identify areas of reaching weakness. The OP group had a larger reachable workspace compared with the NON-OP group, however, both the NON-OP and OP groups showed remarkably similar reaching performance to the two control groups. The 3D movement analysis has an important role in providing post-surgery feedback for identifying specific areas of competence and difficulty experienced by patients. Future studies should use a longitudinal or case study design to compensate for high within-group variability.
References
Moberg E . Surgical treatment for absent single-hand grip and elbow extension in quadriplegia—principles and preliminary experience. J BoneJoint Surg 1975; 57: 196–206.
Fattal C . Motor capacities of upper limbs in tetraplegics: a new scale for the assessment of the results of functional surgery on upper limbs. Spinal Cord 2004; 42: 80–90.
Vastamaki M . Short-term versus long-term comparative results after reconstructive upper-limb surgery in tetraplegic tatients. J Hand Surg 2006; 31: 1490–1494.
Vanden Berghe A, Van Laere M, Hellings S, Vercauteren M . Reconstruction of the upper extremity in tetraplegia: functional assessment, surgical procedures and rehabilitation. Paraplegia 1991; 29: 103–112.
Wuolle K, Van Doren C, Thrope G, Keith MW, Peckham PH . Development of a quantitative hand grasp and release test for patients with tetraplegia using a hand neuroprosthesis. J Hand Surg 1994; 19: 209–218.
Hoffmann G, Laffont I, Hanneton S, Roby-Brami A . How to extend the elbow with a weak or paralyzed triceps: Control of arm kinematics for aiming in C6-C7 quadriplegic patients. Neuroscience 2006; 139: 749–765.
Hoffmann G, Laffont I, Roby-Brami A . Coordination of reaching movements in patients with a cervical spinal cord injury. Curr Psychol Cogn 2002; 21: 305–340.
Laffont I, Briand E, Dizien O, Combeaud M, Bussel B, Revol M et al. Kinematics of prehension and pointing movements in C6 quadriplegic patients. Spinal Cord 2000; 38: 354–362.
Remy-Neris O, Milcamps J, Chikhi-Keromest R, Thevenon A, Bouttens D, Bouilland S . Improved kinematics of unrestrained arm raising in C5-C6 tetraplegic subjects after deltoid-to-triceps transfer. Spinal Cord 2003; 41: 435–445.
Klopcar N, Tomsic M, Lenarcic J . A kinematic model of the shoulder complex to evaluate the arm-reachable workspace. JBiomech 2007; 40: 86–91.
Crago P, Memberg D, Usey MK, Keith MW, Kirsch RF, Chapman GJ et al. An elbow extension neuroprosthesis for individuals with tetraplegia. IEEE Trans Rehabil Eng 1998; 6: 1–6.
Schwartz M, Rozumalski A . A new method for estimating joint parameters from motion data. J Biomech 2005; 38: 107–116.
Begon M, Monnet T, Lacouture P . Effects of movement for estimating the hip joint centre. Gait Posture 2007; 25: 353–359.
Wu G, van der Helm F, Veeger H, Makhsous M, Van Roy P, Anglin C et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion-Part II: shoulder, elbow, wrist and hand. J Biomech 2005; 38: 981–992.
Barber C, Dobkin D, Huhdanpaa H . The quickhull algorithm for convex hulls. ACM Trans Math Software 1996; 22: 469–483.
Friden J, Lieber R . Quantitative evaluation of the posterior deltoid to triceps tendon transfer based on muscle architectural properties. J Hand Surg 2001; 26: 147–155.
Robinson M, Barton G, Lees A, Sett P . The effect of a tendon transfer on the reachable volume of a tetraplegic. Gait Posture 2007; 26: 107.
Acknowledgements
The authors express their sincere thanks to Barbara Hoole for her assistance with the design of this study and the recruitment of participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Robinson, M., Barton, G., Lees, A. et al. Analysis of tetraplegic reaching in their 3D workspace following posterior deltoid-triceps tendon transfer. Spinal Cord 48, 619–627 (2010). https://doi.org/10.1038/sc.2009.193
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.193
Keywords
This article is cited by
-
Upper limb kinematics after cervical spinal cord injury: a review
Journal of NeuroEngineering and Rehabilitation (2015)
-
Surgical Rehabilitation of a Tetraplegic Hand: Comparison of Various Methods of Reconstructing an Absent Pinch and Hook
HAND (2014)
-
Reliability of movement workspace measurements in a passive arm orthosis used in spinal cord injury rehabilitation
Journal of NeuroEngineering and Rehabilitation (2012)
-
Sensory-motor equivalence: manual aiming in C6 tetraplegics following musculotendinous transfer surgery at the elbow
Experimental Brain Research (2010)