Abstract
Study design:
The Symptom Checklist 90 Revised (SCL-90-R) was used to assign participants to either a good adjustment group or a poor adjustment group. Group differences were analyzed with χ2, t-tests and correlations on factors shown in previous research to be related to coping with spinal cord injury (SCI).
Objectives:
This study examines health locus of control (HLC) and attributions of cause and blame in relation to SCI. The replication of study findings in multiple settings is a cornerstone of the evidence base for developing interventions. Previous studies do not show a consensus on the role of attributions of cause and blame in persons with SCI. Similarly, their relationship to adjustment after SCI is unclear. Another attribution, HLC, is similarly analyzed in relation to adjustment.
Setting:
Republic of Ireland.
Methods:
Thirty people with SCI participated. They rated scales measuring psychological adjustment, locus of control (LOC) for health and attributions of cause and blame for the injury.
Results:
The well-adjusted group had a less external HLC. In addition, participants who were well adjusted endorsed the notion they could have avoided their accident significantly more than the poorly adjusted group. Similarly, they rated the belief that they could have caused the accident at a somewhat greater level. They did not, however, blame themselves any more or any less.
Conclusion:
Results are consistent with general LOC theory, and suggest an adaptive or protective internal LOC for accepting responsibility for the injury.
Similar content being viewed by others
Introduction
Locus of control (LOC) is defined as the extent to which the individual judges outcomes to be contingent on his or her behavior.1 Health locus of control (HLC) is the degree to which the individual believes health outcomes are the result of his own actions (internal LOC), luck or chance, or the influence of significant other people (external LOC).
A study of LOC in an spinal cord injury (SCI) sample indicated that persons with recent injuries manifested a more external LOC than an age, gender and education matched able-bodied control group.2 The researchers reported that 39% of the SCI sample had an external score on the LOC of behavior scale,3 as compared with 10% of the control group. A follow-up study of a number of the original participants showed by contrast to the 12-month data that there was only a trend for the SCI group to be more externally focused on LOC of behavior scores at 24 months.4 In an additional paper on the 24-month data, regression analysis found the experience of pain 2 years after injury and feeling out of control of one's life before hospital discharge were predictive of depression 2 years after injury.5
Cluster analysis using the Levenson Internal External Scale,6 showed that the first of three groups who attributed control more externally to chance had significantly higher depression and role dissatisfaction and lower life satisfaction. Those in the other two clusters had more internal attributions or a mix of internal and external attributions and they had better outcomes.7 Correlations between types of LOC and outcomes from studies cited here appear in Table 1.
It appears that individuals with an internal LOC in the sense of a general attributional style seem to be better adjusted than those with an external style. Health-specific measures of LOC have also been researched. Cluster analysis with the Ways of Coping Scale,8 showed that the first of the two groups showing higher self-blame and wishful thinking on the Ways of Coping Scale were less well adjusted.9 People falling into that group endorsed the Multidimensional Health Locus of Control scale (MHLC),10 evenly in terms of internality and externality and reported higher levels of depression and distress. By contrast, the second group, who were better adjusted, relied more on internal attributions than on external ones on the MHLC.
In a study using multiple regression with the MHLC, internality was positively correlated with overall satisfaction (r=0.36) whereas chance was negatively correlated with satisfaction (r=−0.22). In addition, internality was positively correlated with subjective well-being and powerful others were negatively correlated with health indicators.11
A similar study using the MHLC scale indicated internality was positively related to purpose in life, and that purpose in life was related to adjustment. Internal HLC was also related to good adjustment.12 Chance MHLC, was positively related to the negative outcome of neurosis and anxiety (see Table 1).
A clear body of research exists to show that for either general or health-specific measures of LOC, internality is correlated with better outcomes and externality in its various forms is associated with pathology. Seeing ones world as being amenable to change on the basis of one's own actions is evidence of a sense of personal control, and is healthy in our lives. A question remains around the relationship between personal adjustment and blame attributed either internally or externally for the accident that caused the SCI.
In an early study (1977), participants rated (on a 0–5 scale) the extent to which they blamed themselves, and the extent to which they believed they could have avoided what happened.13 Participants also assigned a percentage of blame to themselves, others, environment and chance. These ratings were combined into a single self-blame score. Staff members rated the coping of the participants in the study. A multiple regression suggested that blaming oneself was paradoxically a successful predictor of staff ratings of good coping. Endorsement of self-implicating avoidability, or blaming another, was related to staff ratings of poor coping. Individuals were more likely to blame themselves if they believed they could have avoided the accident.
In a subsequent 1988 study,14 the same procedure for creating a composite self-blame score was used. A comparison was drawn between those who attributed up to 10% of the blame internally (low self-blame group) and those who attributed 11% or more of the blame internally (high self-blame group). In contrast to the 1977 study, analysis found that self-blame correlated with poor coping (see Table 2). However, individuals were again more likely to blame themselves if they believed they could have avoided the accident.14
A European 1988 study compared a group of people injured for <18 months with a group injured for more than 24 months.15 Participants rated their level of concern with attributions of cause and avoidability. For people in the recently injured group, self-rated concern with avoidability correlated with medical staff ratings of poor coping (r=0.85). However, there was little correlation with the rating of coping from the psychologist (r=0.17). For the longer injured group, self-rated concern with avoidability was correlated with good coping as rated by a psychologist (r=0.79), yet, there was little correlation with medical staff ratings (r=0.19). Concern with cause was not significantly correlated with any ratings of coping, and blaming oneself was not addressed in the study. Several previous studies rely on ratings of coping by staff members rather than examining the self-rated coping of participants. This may introduce additional uncontrolled factors or biases and is perhaps a more questionable methodology than self-report.
A 1996 study,16 distinguished between attributions of cause and attributions of blame. The researchers investigated causality using a set of probes that did not use the word blame. Items such as ‘My own behavior caused my accident’ were rated on a 1–7 scale. Avoidability was addressed by rating the statement ‘I feel I could have avoided my accident and therefore my SCI’. Items relating to blame but not using the terms ‘cause’ or ‘caused’ such as ‘I am to blame for my accident’ were also rated. Results again showed a correlation between blaming oneself and self-avoidability (r=0.54). This was of the same order as the correlation between blaming oneself and perceiving self-causation (r=0.66). This 1996 study began to separate out some of the confounding variables of earlier research yet suffered for not addressing the link between adjustment and self-rated attributions of cause and blame. Correlations for attributions of cause and blame and outcomes from studies cited here are listed in Table 2.
It is noteworthy that to a large degree, and unlike studies of LOC, research on attributions of cause or blame in SCI has failed to reach a consensus on several questions. These include whether self-blame or particular attributions for one's own role in causing or avoiding the SCI are adaptive.
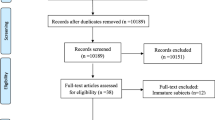
Materials and methods
Participants
All participants (N=30) were wheelchair users and had a traumatic SCI. Injuries were the result of a specifiable acute onset rather than disease or congenital factors. Ten people had sustained a complete injury and 20 people had sustained an incomplete injury. None of the participants had suffered either moderate or severe head injuries. There were 25 men and 5 women. The sample had an average age of 45.37 (range 24–63). They had an average time since injury of 11.63 years (range 2–30). They had an average age at injury of 33.73 years (range 12–58).
Instruments
The SCL-90-R,17 is a self-report inventory that screens for a range of psychopathology. Ninety items are rated on a five-point distress scale ranging from 0 (not at all) to 4 (extremely). There are nine symptom dimensions; somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation and psychoticism. Test–retest reliability for 1 week ranges from 0.78 to 0.90 and internal reliability ranges from 0.77 to 0.90. The SCL-90-R was used to assign participants to one of two adjustment groups. If the respondent has a Global Severity Index score (on Norm B, the non-patient norm) ⩾T score of 63, or if any two primary dimension scores are ⩾T score of 63, then the individual is considered a positive risk or case.
The MHLC Form C,18 assesses the degree to which health-related outcomes are observed by the individual as a result of his own actions, luck or chance, or the influence of significant other people such as health professionals or family members. Form C is designed to be condition specific unlike the earlier scale.10 The 18 items are rated on a six-point scale ranging from 1 (strongly disagree) to 6 (strongly agree). The four subscales are internally consistent with alpha reliabilities of 0.79–0.82 for the chance subscale, 0.70–0.71 for the powerful others subscale, 0.71 for the doctors subscale, and 0.85–0.87 for the internal subscale.18 Test–retest reliability over 1 month was 0.80 for the internal subscale, 0.72 for the chance subscale, 0.58 for the doctors subscale and 0.40 for the other people subscale. Factor analysis of 290 patients with arthritis or pain or diabetes or cancer confirmed a four-factor solution. In this study, participants rated items based on beliefs regarding general health after SCI rather than the unchanging SCI itself.
Attributions of cause and blame and perceptions of avoidability. Participants rated seven items similar to those used in a previous study,16 on a seven-point scale ranging from 1 (not at all true) to 7 (extremely true): ‘I believe that I caused the incident that led to my injury’. ‘I believe that another person or persons caused the incident that led to my injury’. ‘I believe that chance or fate caused the incident that led to my injury’. ‘I believe that I could have avoided the incident that led to my injury’. ‘I believe that another person or persons could have avoided the incident that led to my injury’. ‘I blame myself for my injury’. ‘I blame another person or persons for my injury’.
Procedure
Participants were sent a letter by Spinal Injuries Ireland, or the Irish Wheelchair Association, that informed them of the study aims, and requested co-operation. Subsequent to obtaining informed consent each person was interviewed on a prearranged date at his or her home. Each question was read out and responses were recorded. All interviews were conducted in person; there were no telephone interviews or postal surveys.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
The SCL-90-R operational definition of caseness was used to define the two adjustment groups
There was no evidence for a significant difference in gender between the two adjustment groups (χ2=0.028, df=1, P>0.05) or that type of injury (complete or incomplete) differed between groups (χ2=1.89, df=1, P>0.05). Similarly, there was no evidence that age differed between the groups (t=−0.39, df=28, P>0.05), or that age at injury differed between groups (t=−1.24, df=28, P>0.05), or that the time since injury differed between the two groups (t=1.84, df=28, P>0.05).
T-tests were also carried out on the data to test hypotheses with respect to HLOC scores. Kruskal–Wallace analysis of variances were carried out on the data for attributions of cause, blame and avoidability. Cronbach's α for the current sample was calculated for each subscale and is documented along with means, s.d. and t-values in Tables 3 and 4.
The well-adjusted group had a significantly lower others HLC score (t=−2.24, df=28, P=0.016). The well-adjusted group endorsed self-cause at a somewhat higher level (H=2.85, df=1, P=0.091) and endorsed self-avoidability at a significantly higher level than the less well-adjusted group (H=6.52, df=1, P=0.011).
Discussion
Results from the MHLC (Form C) indicate that the adjustment groups did not differ in beliefs regarding the effect of their actions, chance or their doctor's actions on their health. The less well-adjusted group endorsed their belief in the effect of other's actions at a greater level. The well-adjusted group was therefore less external in perceptions of control over health. Those people saw less of a role for their family and friends in the maintenance of their health after SCI than the people who were poorly adjusted. This is consistent with general LOC theory and HLC theory.
This research also investigated participants’ endorsement of attributions of cause and blame. We failed to observe a difference in self-blame between the adjustment groups. However, participants were asked to separate cause, blame and avoidability. The well-adjusted participants endorsed the belief that they could have avoided their accident at a significantly greater level than the poorly adjusted group. Another attribution ‘self-cause’ was different to the level of a trend. The trend in the data suggests that the well-adjusted group tended more toward the belief that they caused their own accident than the poorly adjusted group.
Further investigation is required to clarify if taking responsibility for the injury reflects a type of internal LOC with respect to the accident. If interpreted in this way, the results suggest that the well-adjusted group manifested a greater internal LOC with respect to aspects of the accident. They denied blaming themselves, yet weakly acknowledged a causal role, and strongly endorsed the possibility they could have avoided the accident. A longitudinal methodology would be required to establish any causal relationship between attributions and adjustment.
This study has a number of limitations. A drawback with the methodology is that there was no mechanism to objectively measure the extent to which persons who said they caused/could have avoided their accident actually caused/could have avoided their accident. There is a question of false positives and false negatives in this regard. This should be addressed as a key factor in any future study. In addition, the extremely small sample size makes generalization difficult. The sample size represents around 2 years worth of incidences of SCI in the Republic of Ireland in that around 12–15 people have a SCI annually. The sample of 30 was a self-selected volunteer sample, raising the possibility that people who were particularly poorly adjusted, or who were encountering significant personal challenges, chose not to participate.
References
Rotter JB . Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs: General and Applied 80 (1 Whole No 609) 1966.
Hancock K, Craig A, Tennant C, Chang E . The influence of spinal cord injury on coping styles and self-perceptions: A controlled study. Aust N Z J Psychiatry 1993; 27: 450–456.
Craig A, Franklin J, Andrews G . A scale to measure locus of control of behaviour. Br J Med Psychol 1984; 57: 173–180.
Craig AR, Hancock KM, Chang E . The influence of spinal cord injury on coping styles and self-perceptions two years after the injury. Aust N Z J Psychiatry 1994; 28: 307–312.
Craig AR, Hancock KM, Dickson HG . Spinal cord injury: a search for determinants of depression two years after the event. Br J Clin Psychol 1994; 33: 221–230.
Levenson HI . Activism and powerful others: distinctions within the concept of internal-external control. J Pers Assess 1974; 38: 377–385.
Chan RCK, Lee PWH, Lieh-Mak F . The pattern of coping in persons with spinal cord injuries. Disabil Rehabil 2000; 22: 501–507.
Folkman S, Lazarus RS . An analysis of coping in a middle aged community sample. J Health Soc Behav 1980; 21: 219–239.
Frank RG, Umlauf RL, Wonderlich SA, Askanazi GS, Buckelew SP, Elliott TR . Differences in coping styles among persons with spinal cord injury: a cluster-analytic approach. J Consult Clin Psychol 1987; 55: 727–731.
Wallston KA, Wallston BS, DeVellis R . Development of the multidimensional health locus of control (MHLC) scales. Health Educ Monogr 1978; 6: 160–170.
Krause JS, Stanwyck CA, Maides J . Locus of control and life adjustment: relationship among people with spinal cord injury. Rehabil Counsel Bull 1998; 41: 162–173.
Thompson NJ, Coker J, Krause JS, Henry E . Purpose in life as a mediator of adjustment after spinal cord injury. Rehabil Psychol 2003; 48: 100–108.
Bulman RJ, Wortman CB . Attributions of blame and coping in the ‘real world’: severe accident victims react to their lot. J Pers Soc Psychol 1977; 35: 351–363.
Nielson WR, MacDonald MR . Attributions of blame and coping following spinal cord injury: is self-blame adaptive? J Soc Clin Psychol 1988; 7: 163–175.
Van Den Bout J, Van Son-Schoones N, Schipper J, Groffen C . Attributional cognitions, coping behaviour, and self-esteem in inpatients with severe spinal cord injuries. J Clin Psychol 1988; 44: 17–22.
Davis CG, Lehman DR, Cohen-Silver R, Wortman CB, Ellard JH . Self blame following a traumatic event: the role of perceived avoidability. Pers Soc Psychol Bull 1996; 22: 557–567.
Derogatis LR . Symptom Checklist 90-R: Administration, Scoring and Procedures Manual, (3rd ed.) National Computer Systems, Inc.: Minneapolis, MN, 1994.
Wallston KA, Stein MJ, Smith CA . Form C of the MHLC scales: a condition-specific measure of locus of control. J Pers Assess 1994; 63: 534–553.
Acknowledgements
We thank Ms Joan Carthy and Mr Colm Hooly of Spinal Injuries Ireland and Ms Anne Winslow of the Irish Wheelchair Association.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Waldron, B., Benson, C., O'Connell, A. et al. Health locus of control and attributions of cause and blame in adjustment to spinal cord injury. Spinal Cord 48, 598–602 (2010). https://doi.org/10.1038/sc.2009.182
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.182
Keywords
This article is cited by
-
Forgiveness and acceptance of disability in people with traumatic spinal cord injury—the mediating role of disability appraisal. A cross-sectional study
Spinal Cord (2020)
-
Mediating effects of social support and self-concept on depressive symptoms in adults with spinal cord injury
Spinal Cord (2015)
-
Associations between psychological factors and quality of life ratings in persons with spinal cord injury: a systematic review
Spinal Cord (2012)
-
Psychological resources in spinal cord injury: a systematic literature review
Spinal Cord (2012)