Abstract
Study design:
A retrospective analysis of prospectively collected data.
Objective:
A hemisection of the spinal cord is a frequently used animal model for spinal cord injury (SCI), the corresponding human condition, that is, the Brown-Sequard syndrome (BS), is relatively rare as compared with the central cord syndrome (CC). The time course of neurological deficit, functional recovery, impulse conductivity and rehabilitation length of stay in BS and CC subjects were compared.
Setting:
Nine European Spinal Cord Injury Rehabilitation Centers.
Methods:
Motor score, walking function, daily life activities, somatosensory evoked potentials and length of stay were evaluated 1 and 6 months after SCI, and were compared between age-matched groups of tetraparetic BS and CC subjects.
Results:
For all analyzed measures no difference in the time course of improvement was found in 15 matched pairs.
Conclusion:
In contrast to the assumption of a better outcome of subjects with BS, no difference was found between the two incomplete SCI groups. This is of interest with respect to the different potential mechanisms leading to a recovery of functions in these two SCI subgroups.
Similar content being viewed by others
Introduction
The consequence of trauma to the spinal cord is a partial or complete loss of motor, sensory and autonomic functions below the level of lesion. According to European and American databases the proportion of traumatic patients experiencing incomplete spinal cord injury (SCI) amounts to 52.8 and 44.3%, respectively.1 Within the spectrum of incomplete damage to the neural structures within the spinal canal, five distinct syndromes can be categorized: the central cord- (CC), the Brown-Sequard (BS), the anterior cord, the conus medullaris and the cauda equina syndromes.2, 3
A comprehensive overview of the clinical characteristics of these syndromes is provided elsewhere.4 Most common is the CC, occurring in approximately 9% of all traumatic SCIs.4 It is characterized by pronounced loss of motor function in the upper extremities due to a lesion of the central region of the cervical spinal cord.5 Typically, the CC results from a hyperextension of the cervical spine during a fall, mainly in older patients with a pre-existing cervical spondylosis.6 The prognosis for a functional recovery of the CC has been suggested to be rather favorable, depending on the age of the subject.5, 6, 7, 8, 9, 10, 11, 12
The BS is caused by an injury restricted to one side of the spinal cord resulting in an ipsilateral paresis and loss of deep sensation and a contralateral loss of pain and temperature sensation.13 The BS accounts for only about 3% of all traumatic SCI.4 A pure form of BS occurs rarely. Therefore, clinically the criteria for classifying a BS were broadened. The ‘Brown-Sequard-plus’ syndrome encompasses SCI subjects suffering from an asymmetric paresis combined with relatively pronounced analgesia on the less paretic side.14, 15 Patients with BS are suggested to have a favorable prognosis for functional recovery.4, 15, 16 According to textbooks,17 the BS is thought to have a better outcome than the CC. Such a difference in outcome is of interest with respect to the possibility of different mechanisms underlying spontaneous functional recovery after an incomplete SCI in humans. Furthermore, unilateral lesions of the spinal cord, that is, injuries that correspond to the BS, are frequently used in animal research as models to investigate new interventions for spinal cord repair.18
The aim of the present study was to determine whether different types of incomplete SCI differ in outcome. Specifically it was of interest to evaluate and compare the course of neurological, functional and electrophysiological measures in BS and CC subjects.
Materials and methods
This retrospective review encompassed data from a European network of nine SCI rehabilitation centers (EMSCI).19 Local Ethics Committee of all centers approved the data collection and all subjects gave written, informed consent.
Subjects and general procedures
All patients experienced traumatic or ischemic SCI and were referred to one of the participating centers. They were examined according to the EMSCI protocol.19 Patients with traumatic brain lesion, peripheral nerve damage or polyneuropathy were excluded.
For this study, the EMSCI database was screened for tetraparetic patients with either pronounced loss of motor function of the upper extremities (CC) or restricted to one side (BS). The criterion for differential paresis in this study was an arbitrarily defined difference in American Spinal Injury Association (ASIA) motor score (MS) of 19 or more points between the upper and lower extremities (CC), or the right and left side of the body (BS), respectively (see section Clinical, functional and electrophysiological measures). Previous studies applied different cut-off values, which in general were lower.3, 8, 11 The relatively greater difference in ASIA MS allowed us to include patients with clear representations of the respective syndromes. In order to ensure comparable groups regarding neurological level of lesion and age, we formed two matched groups from all patients who fulfilled the above-mentioned criteria.
Data assessments
Examinations were performed at 1 and 6 months after SCI by specialized and trained physicians (neurological examination and neurophysiological recordings) and therapists (walking and daily life functional tests). The results of these examinations were sent anonymously to a central database.
Clinical, functional and electrophysiological measures
MS was assessed according to the international standard classification of the ASIA.2 Total MS and MS of more and less impaired extremities of the body were used for comparison of the two groups. While total MS and its recovery are expected to be similar in both groups of patients, one would assume a substantial difference in the distribution of the voluntary muscle strength as measured with the MS. Therefore, MS sum was calculated for upper (more impaired) and lower limbs (less impaired) for CC subjects, and for the weak (more impaired) and the strong (less impaired) sides for patients presenting with BS, respectively.
Walking function was assessed using the Walking Index for Spinal Cord Injury-II (WISCI-II)20 and the 10-Meter Walk Test (TMW).21
The degree of disability during daily task performance (that is, self-care, respiration and sphincter management as well as mobility) was examined using the Spinal Cord Independence Measure (SCIM-II).22
Neurophysiological recordings were obtained from ascending (somatosensory evoked potentials, SSEP) pathways. For the present study, signal amplitudes were used for analysis.19 As shown recently,1 SSEP amplitudes reflect to some extent the recovery of function in incomplete SCI, while spinal conductivity does little change during the course of an SCI. Analogous to the analysis of the MSs, the amplitudes of the more and less affected extremities were separately explored.
Data analysis
The level for statistical significance for all analyses was set at P=0.05.
χ2-test and t-test were used to control for equality of groups regarding sex, age and neurological level.
Differences between 1 and 6 months after SCI were calculated to evaluate changes in the outcome measures. These changes were compared within and between the two groups.
Given the limited number of participants, non-parametric methods were used, that is, for within-group comparisons Wilcoxon's signed-rank test and for between-group comparisons Mann–Whitney U-test.
Not all data was available for all patients for both the time points. For every comparison, we, therefore, checked whether matching was violated by the drop-outs using the above-mentioned methods (that is, χ2-test for sex and neurological level, and t-tests for age).
Microsoft Excel 2002 (Microsoft, Redmond, WA, USA) and SPSS for Windows 14.0 (SPSS Inc., Chicago, IL, USA) were used for analysis.
Results
Sample characteristics
Two groups were formed: (i) Fifteen subjects with BS and (ii) 15 subjects with CC. In the BS group the mean MS difference between the strong and weak side was 26.93±5.69 points. In addition, the sensory criterion relating to pain (contralateral reduction of ASIA pin-prick sensation) was present in 9/15 individuals and touch sensation (ipsilateral ASIA light touch) was reduced in 2/15 patients. In CC subjects the difference in MS between lower and upper extremities was 23.14±3.84 points.
The groups were similar regarding age, neurological level of the lesion and sex (Table 1). This was true also for all comparisons that did not include the whole sample. The etiology of the SCI was traumatic, except for two cases in the BS group where ischemia was the reason for paralysis.
ASIA MS
The total MS improved significantly from the first to the sixth month after SCI for both BS and CC groups. Between groups, there was no difference in total MS at the first or the sixth month.
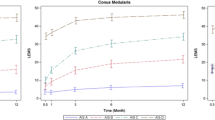
In the BS group, the MS of arms and legs improved on both more and less impaired sides, but to a greater degree on the more affected side. The same observation was made in the CC group. The MS of the arms (more impaired) and legs (less impaired) improved significantly, but recovery was more pronounced in the arms. No difference between BS and CC was found for the sum scores from the more and the less affected limbs (Table 2a and Figure 1).
Mean values of the ASIA MSs examined 1 and 6 months after SCI for patients with CC and BS (*P⩽0.05, **P⩽0.01; ***P⩽0.001). The dashed lines represent the maximum values of the MSs. ASIA, American Spinal Injury Association; BS, Brown-Sequard syndrome; CC, central cord syndrome; MS, motor score; SCI, spinal cord injury.
In order to recognize the influence of a possible ceiling effect on the course of recovery, MS values of the early examination (that is, 1 month after SCI) were evaluated. Only 2/15 patients scored 25 points on the upper extremity MS (UEMS) and 6/15 on the lower extremity MS (LEMS) on the less impaired side of the BS group. In the CC group only 2/15 patients achieved maximum scores in LEMS in the early examination.
Walking function
Both groups of subjects showed significant improvement in walking function (Table 2 and Figure 2). There was no statistical difference between the groups regarding the initial and final values in the TMW and WISCI-II tests.
Spinal cord independence measure
There was significant improvement in the total scores of the Spinal Cord Independence Measure and its sub-scores in both the groups. No difference between BS and CC was found in the values obtained at 1 and 6 months after SCI, or in the mean changes (Table 2 and Figure 3).
SSEPs
No significant change was observed in SSEP amplitudes of N. ulnaris and N. tibialis. In the BS group there was a positive trend in improvement (P=0.051) of the summed amplitudes of N. ulnaris and N. tibialis on the more affected side. However, there was no group difference in initial and final values (Table 2 and Figure 4). The clinical examination provides a rather rough measure of the sensory deficit. Therefore, no correlation with SSEP can be expected.
Rehabilitation length of stay
Subjects with CC stayed shorter in rehabilitation than BS subjects (113.5±81. 8 versus 131.9±52.2 days). However, this difference was not statistically significant.
Discussion
The aim of this study was to explore the extent to which the neurological, functional and electrophysiological recovery differs between BS and CC subjects, which might be due to a different anatomical damage of spinal tracts associated with these two types of incomplete SCI. Studies with reasonable number of participants comparing specifically the outcome of BS and CC are rare. In humans, the incidence of the BS is lower as compared with that of CC, but lateral hemisections of the spinal cord are frequently used in animal research to model SCI. However, no clear-cut criteria are defined for BS and CC. Therefore, we followed the algorithm proposed elsewhere.4 Compared with the MS, the evaluation of sensory scores is generally less reliable.23 Nevertheless the differential sensation criterion of the BS group was fulfilled in most subjects.
A bimodal age distribution of patients with CC suggested that this group might consist of two different populations regarding etiology and outcome.7, 9, 11, 12, 14 At the time of the analysis, the EMSCI network included approximately 1000 SCI patients. From this population, only 30 patients who were matched regarding age and neurological level of lesion fulfilled our inclusion criteria. The age of our sample was slightly greater than the age at injury of the general SCI population.24
In two BS patients the reason for the SCI was ischemia. We did not consider this fact further since the results of a previous study suggest that the outcome is similar in ischemic and traumatic SCI.25
It was assumed that BS has a better outcome than the CC.17 Such a difference might also be expected on the basis of animal experiments.26, 27 The mechanisms underlying functional recovery after unilateral SCI (BS) in animals, for example, compensatory sprouting of spared fiber tracts above and below the lesion site, might also play a role in the human situation.26 Interestingly, BS and CC subjects recovered to about the same extent suggesting equally efficient mechanisms of functional recovery in these two anatomically dissimilar types of SCI. However, one has to be aware that the human BS can only insufficiently reflect the hemisection animal model. However, the small patient group studied here can hardly allow drawing serious conclusions about the mechanisms underlying the recovery of function after an SCI.
Course of motor deficit
In line with the literature, recovery of motor deficits was seen in both syndromes.5, 10, 11, 13, 17, 18, 19 Notably, the change in MS was significant on both the more and the less impaired limbs. Nevertheless, the rate of recovery was greater on the more than the less affected limbs, which might be due to two facts: (1) A greater gradient on the more affected side might lead to stronger effects on neuronal plasticity to become maximally exploited and (2) on the less affected side a ceiling effect might lead to less powerful recovery, that is, the less impaired limbs may have already early achieved scores near maximum. However, even when subjects who achieved maximum scores already in the early examination were excluded, the result did not change.
Recovery of walking function
In line with the literature,12 the favorable recovery of walking function in CC subjects corresponds to the fact that arms are more impaired than legs in this syndrome by definition. Most incomplete SCI subjects regain ambulatory function.8, 10, 13 However, in our sample, approximately two-thirds of CC and only one-third of BS patients became unrestricted walkers within the first 6 months after an SCI. Overall the difference in the outcome of walking function was not significant. The observation that walking function in BS subjects changes to a similar extent, was also noted elsewhere.8, 5 While in the study by McKinley the sub-score ‘mobility’ of the Functional Independence Measure (FIM) was similar at admission, patients with BS achieved even higher discharge values as compared with those with CC.4 In our study, patients with BS had lower admission and discharge values in the WISCI-II test, but showed similar changes as patients with CC.
The course of somatosensory recordings
Since the number of measurements was limited, the results of the neurophysiological recordings have to be considered carefully. The observation that SSEPs showed little change, that is, behaved differently from the recovery in function after an SCI, is in line with an earlier study of incomplete and complete SCI subjects.1 The SSEP recordings reflect the sensory deficits after an SCI, while the clinical examination provides only a rough measure (three items). Therefore, no close relationship between these measures can be expected.
Study limitations
In the animal model, the pure form of the BS syndrome can be investigated due to a controlled experimental lesion of the spinal cord (the lateral hemisection). The accuracy of these lesions can be verified by histological examinations. In contrast, the occurrence of pure BS in humans is rare. For practical reasons, the categorization to either the CC or BS group was based on MS. This might have led to some misclassifications since BS is further characterized by contralateral loss of pain and temperature sensation below the level of lesion,15 which was not present in all BS subjects included. In addition, classification of patients as having CC based on upper-to-lower limb MS differences without imaged verification of pathology, is at risk of including patients with bilateral corticospinal (that is, dorsifunicular) involvement rather than central neuropathology alone. This limits the interpretation about which tracts recover function.
Additionally, the samples of CC and BS subjects were of limited size, which raised the possibility that we accepted the null hypotheses, although there were real differences in the change of the measures evaluated.
Conclusions
This study shows that there is no difference in the functional recovery between BS and CC subjects over the first 6 months after an SCI, although spinal tracts were differentially affected.
The spinal cord seems to have the capacity to compensate for a damage that does not depend on the integrity of a specific tract.28 Finally, such a study of a sub-population of SCI subjects requires the formation of clinical networks, which apply standardized examinations at distinct time points, which is a prerequisite to enable the study of such a subpopulation of spinal cord-injured subjects.
References
Curt A, Van Hedel HJ, Klaus D, Dietz V . Recovery from a spinal cord injury: significance of compensation, neural plasticity, and repair. J Neurotrauma 2008; 25: 677–685.
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003; 26 (Suppl 1): S50–S56.
Hayes KC, Hsieh JT, Wolfe DL, Potter PJ, Delaney GA . Classifying incomplete spinal cord injury syndromes: algorithms based on the International Standards for Neurological and Functional Classification of Spinal Cord Injury Patients. Arch Phys Med Rehab 2000; 81: 644–652.
McKinley W, Santos K, Meade M, Brooke K . Incidence and outcomes of spinal cord injury clinical syndromes. J Spinal Cord Med 2007; 30: 215–224.
Roth EJ, Lawler MH, Yarkony GM . Traumatic central cord syndrome: clinical features and functional outcomes. Arch Phys Med Rehab 1990; 71: 18–23.
Bosch A, Stauffer ES, Nickel VL . Incomplete traumatic quadriplegia. A ten-year review. JAMA 1971; 216: 473–478.
Aito S, D’Andrea M, Werhagen L, Farsetti L, Cappelli S, Bandini B et al. Neurological and functional outcome in traumatic central cord syndrome. Spinal Cord 2007; 45: 292–297.
Dvorak MF, Fisher CG, Hoekema J, Boyd M, Noonan V, Wing PC et al. Factors predicting motor recovery and functional outcome after traumatic central cord syndrome: a long-term follow-up. Spine 2005; 30: 2303–2311.
Newey ML, Sen PK, Fraser RD . The long-term outcome after central cord syndrome: a study of the natural history. J Bone Joint Surg 2000; 82: 851–855.
Penrod LE, Hegde SK, Ditunno Jr JF . Age effect on prognosis for functional recovery in acute, traumatic central cord syndrome. Arch Phys Med Rehab 1990; 71: 963–968.
Tow AM, Kong KH . Central cord syndrome: functional outcome after rehabilitation. Spinal Cord 1998; 36: 156–160.
Harrop JS, Sharan A, Ratliff J . Central cord injury: pathophysiology, management, and outcomes. Spine J 2006; 6: 198S–206S.
Tattersall R, Turner B . Brown-Sequard and his syndrome. Lancet 2000; 356: 61–63.
Koehler PJ, Endtz LJ . The Brown-Sequard syndrome. True or false? Arch Neurol 1986; 43: 921–924.
Roth EJ, Park T, Pang T, Yarkony GM, Lee MY . Traumatic cervical Brown-Sequard and Brown-Sequard-plus syndromes: the spectrum of presentations and outcomes. Paraplegia 1991; 29: 582–589.
Little JW, Halar E . Temporal course of motor recovery after Brown-Sequard spinal cord injuries. Paraplegia 1985; 23: 39–46.
Woosli RM, Young RR . The clinical diagnosis of disorders of the sinal cord. In: Young RM, Woosley RM (eds). Diagnosis and Management of Disorders of the Spinal Cord. Saunders: Philadelphia, 1995 pp 135–144.
Freund P, Schmidlin E, Wannier T, Bloch J, Mir A, Schwab ME et al. Nogo-A-specific antibody treatment enhances sprouting and functional recovery after cervical lesion in adult primates. Nat Med 2006; 12: 790–792.
Curt A, Schwab ME, Dietz V . Providing the clinical basis for new interventional therapies: refined diagnosis and assessment of recovery after spinal cord injury. Spinal Cord 2004; 42: 1–6.
Ditunno Jr JF, Ditunno PL, Graziani V, Scivoletto G, Bernardi M, Castellano V et al. Walking index for spinal cord injury (WISCI): an international multicenter validity and reliability study. Spinal Cord 2000; 38: 234–243.
van Hedel HJ, Wirz M, Dietz V . Standardized assessment of walking capacity after spinal cord injury: the European network approach. Neurol Res 2008; 30: 61–73.
Catz A, Itzkovich M, Steinberg F, Philo O, Ring H, Ronen J et al. The Catz-Itzkovich SCIM: a revised version of the Spinal Cord Independence Measure. Disabil Rehabil 2001; 23: 263–268.
Furlan JC, Fehlings MG, Tator CH, Davis AM . Motor and sensory assessment of patients in clinical trials for pharmacological therapy of acute spinal cord injury: psychometric properties of the Asia standards. J Neurotrauma 2008; 25: 1273–1301.
Spinal cord injury. Facts and figures at a glance. J Spinal Cord Med 2008; 31: 357–358.
Iseli E, Cavigelli A, Dietz V, Curt A . Prognosis and recovery in ischaemic and traumatic spinal cord injury: clinical and electrophysiological evaluation. J Neurol Neurosurg Psychiatry 1999; 67: 567–571.
Mendell LM . Modifiability of spinal synapses. Physiol Rev 1984; 64: 260–324.
Raineteau O, Schwab ME . Plasticity of motor systems after incomplete spinal cord injury. Nat Rev 2001; 2: 263–273.
Nathan PW . Effects on movement of surgical incisions into the human spinal cord. Brain 1994; 117 (Part 2): 337–346.
Acknowledgements
We thank the participating patients, D Klaus for data management and the following who contributed to the data presented: PD Dr R Abel (Krankenhaus Hohe Warte Bayreuth, Bayreuth, Germany), Dr J Benito (Institut Guttmann, Barcelona, Spain), Professor B Bussel (Hopital Raymond-Poincarè, Garches, France), Professor J Duysens (Rehabilitation Centre Nijmegen, Nijmegen, the Netherlands), Professor HJ Gerner (Orthopädische Universitätsklinik Heidelberg, Heidelberg, Germany), Professor J Harms (SRH Klinikum Karlsbad-Langensteinbach, Karlsbad-Langensteinbach, Germany) Dr T Meiners (Wicker-Klinik, Bad-Wildungen, Germany), Dr M Potulski (BG Unfallklinik Murnau, Murnau, Germany) and Dr K Röhl (BG Bergmannstrost, Halle, Germany). Furthermore, we thank Rachel Jurd for proofreading. This study was sponsored by the International Institute for Research in Paraplegia (project: EMSCI; no. P66) and the European Community Seventh Framework Programme (project: spinal cord repair, no. 201144).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Wirz, M., Zörner, B., Rupp, R. et al. Outcome after incomplete spinal cord injury: central cord versus Brown-Sequard syndrome. Spinal Cord 48, 407–414 (2010). https://doi.org/10.1038/sc.2009.149
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.149
Keywords
This article is cited by
-
Central cord syndrome definitions, variations and limitations
Spinal Cord (2023)
-
Comparison of outcomes between people with and without central cord syndrome
Spinal Cord (2020)
-
Modular control of gait after incomplete spinal cord injury: differences between sides
Spinal Cord (2017)
-
Is the outcome in acute spinal cord ischaemia different from that in traumatic spinal cord injury? A cross-sectional analysis of the neurological and functional outcome in a cohort of 93 paraplegics
Spinal Cord (2011)