Abstract
Objectives:
To investigate the relationship between medications known to cause fatigue in spinal cord injury (SCI) and fatigue severity and to describe the pattern of prescription of these medications.
Study design:
Retrospective chart review.
Setting:
GF Strong Rehabilitation Centre, Vancouver, British Columbia, Canada.
Methods:
Medical charts of 136 individuals admitted to the GF Strong Outpatient SCI Program between December 2004 and May 2007 were reviewed. Data collected included information on medications, clinical and demographic characteristics and Fatigue Severity Scale (FSS) scores. Multiple linear regression techniques were used to analyse the data.
Results:
Fifty-two percent of the subjects had clinically relevant fatigue. As a group, the subjects were taking 147 different medications; 41/147 medications were identified as causing fatigue. The two most commonly prescribed categories of medications were antispasticity medications (75 subjects) and analgesic medications (61 subjects). Although several variables were found to contribute to the FSS scores including the use of fatigue-causing medications, the presence of pain (7.6% of variance) and the use of fatigue-causing analgesics (4.2% of variance) explained the most variance in the scores.
Conclusion:
Fatigue is prevalent in outpatients with SCI. Fatigue-causing medications contribute to a higher FSS score. Clinicians treating persons with SCI should be aware that fatigue is a common and significant problem. Clinicians should be aware that fatigue may be exacerbated by the use of medication and should enquire about the effects of medication on fatigue when assessing and prescribing new medications.
Similar content being viewed by others
Introduction
Fatigue, defined as an overwhelming sense of tiredness, lack of energy and a feeling of total exhaustion,1 is a silent barrier that can magnify an existing physical impairment, such as spinal cord injury (SCI), and further reduce participation in work, leisure, social activities and reduce quality of life.1 Studies of individuals with SCI2, 3, 4 have identified fatigue as a problem and recently, we reported that the prevalence of fatigue severe enough to interfere with function was 57% in a sample of outpatients with SCI.5
Rehabilitation practitioners are limited in their ability to address fatigue because there is insufficient research on the diagnosis and treatment of fatigue in SCI and therefore, evidence-based approaches are lacking. Variables such as completeness of injury, spasticity, pain and number of medications have been identified as potential contributors to fatigue in SCI.5 However, only the completeness of the injury has been found to be important in multivariable analyses.5 Medications have not been shown to be important in these analyses, which is interesting to us, as fatigue is listed as a side effect for many medications. Moreover, many individuals with SCI are often on several medications that may contribute to fatigue.5
There is limited research on the influence of medications on fatigue in SCI and most literature simply reports the number of medications5, 6 or a select list of known fatigue-causing medications.5 This is a relatively crude and limited approach to measuring the impact of this potentially important variable.5 An earlier study on patients with multiple sclerosis showed that medications had an impact on measurements of fatigue;6 therefore, we hypothesize similar findings in individuals with SCI who take fatigue-causing medications.
The purpose of this study was to investigate the relationship between the use of medications and the severity of fatigue in individuals with SCI. The specific objectives of the study were to (1) describe the number and type of fatigue-causing medications taken by individuals with SCI, (2) assess the relationship between the number and type of fatigue-causing medications and self-reported fatigue among individuals with SCI and (3) determine whether fatigue-causing medications were important in predicting fatigue in the presence of other factors in individuals with SCI.
Materials and methods
Sample
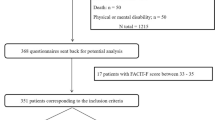
In this chart review, individuals with SCI who were admitted to the outpatient SCI program at GF Strong Rehabilitation Centre (a tertiary spinal cord rehabilitation facility) between 1 December 2004 and 31 May 2007 (n=215) were included. Individuals were excluded if there was incomplete information about fatigue severity (n=11), missing admission information (n=5) or a diagnosis other than traumatic SCI (for example spina bifida (n=63)). The final sample consisted of 136 individuals (63% of the accessible outpatients).
Protocol
All data were abstracted from medical charts using a form we created and used in an earlier study5 to record the variables of interest. If the variables were not available in a subject's chart, the data were considered missing and the individual was excluded. Data were abstracted by three individuals who were training to become health professionals. Double abstraction for recruited subjects was conducted until consistent abstraction was completed (n=10). All applicable governmental and institutional regulations concerning the ethical use of human subjects were followed during the course of this research.
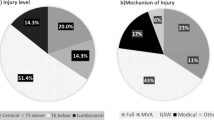
Measurement
Variables collected included general demographic information (age, gender, marital status and employment status), medical history and injury-related information (completeness of lesion, ASIA impairment scale and level, mechanism and duration of injury). The reason for referral was based on the primary need articulated at admission and classified either as medical, equipment, social or functional (for example assistance for activities of daily living) and recorded as a binary (yes/no) response. The presence of pain and spasticity were also recorded as yes/no. Information about living arrangements, attendant care and current mobility aid use was recorded. The names and dosages of all medications taken at the time the fatigue information was collected were recorded. Clinically relevant variables (pain, spasticity, medications, fatigue severity and so on) were systematically collected on acceptance into the SCI outpatient program. Each outpatient received a package of forms that they completed and returned to the program before the first appointment.
Fatigue
Information on fatigue severity was captured using the Fatigue Severity Scale (FSS). This nine-item self-report scale is used widely to assess disabling fatigue in individuals with neurological disorders. It has been shown to be valid and reliable in SCI.7 The FSS assesses the impact of fatigue and functional outcomes related to fatigue.8 The FSS requires respondents to rate each item using a seven-point scale ranging from one (completely disagree) to seven (completely agree). A mean score of four or more has been used to indicate that an individual is experiencing significant fatigue.1, 7, 9 Anton et al.10 reported that the FSS is internally consistent (Cronbach α=0.89) and reliable on retesting (intraclass correlation coefficient=0.84); support for validity for a sample of individuals with motor complete SCI was demonstrated.10
Medication classification
To classify medications as fatigue causing or not, five physiatrists with SCI expertise categorized each drug identified in the chart review. Each physician was asked to independently indicate whether the medication never, seldom, often, or always caused clinically significant fatigue. They were instructed not to consult secondary sources of medication information. A master list was compiled from their responses and consensus was deemed present if four out of the five clinicians agreed that the medication was either non-fatigue causing (never or seldom), or fatigue causing (often or always). When consensus was not achieved, the group was brought together to discuss each drug. To confirm the results, each medication was compared with reports from the Compendium of Pharmaceuticals and Specialties for fatigue, somnolence, drowsiness, weakness, sedation or asthenia as an adverse effect.11 The Compendium of Pharmaceuticals and Specialties is a collection of monographs written by pharmaceutical companies, published by the Canadian Pharmacists Association and consulted frequently by Canadian physicians. For medications with more than one potential clinical indication, the medication was grouped into a functional category according to its primary clinical indication in the treatment of subjects with SCI.
Analysis
The appropriate parametric and non-parametric statistics such as means, standard deviations and proportions were calculated to describe the participants’ demographic, impairment, clinical and drug-related characteristics (objective 1). We report the fatigue level using the mean FSS and a cut FSS score of ⩾4 to indicate ‘severe fatigue’.1, 7, 9
Pearson's correlation coefficients and t-tests were used to assess the bivariable relationship between fatigue and the number/type of fatigue-causing medications (objective 2). Correlation coefficients and t-tests were also used to identify other variables that would be statistically controlled when assessing the independent contribution of fatigue-causing medications in predicting fatigue (objective 3) using linear regression analyses. With one exception, all the variables that were found to be statistically associated with fatigue (correlation coefficient of r>0.2) or statistically significant (P<0.05) mean fatigue group scores using a t-test or ANOVA were included in the final multiple linear regression model. The variable that was not included was use of fatigue-causing medications in favour of use of fatigue-causing analgesics, and use of fatigue-causing medications excluding those for pain. This prevented colinearity and better differentiated the medications variable. All binary variables entered into the regression model were coded No=0 and Yes=1. Analyses were conducted using SPSS version 15.
Results
Sample and injury characteristics
The mean age of the mostly male (77%) sample was 43.7 (s.d.=12.9) years (Table 1). The mean duration of injury was 14.1 (s.d.=12.0) years and the mean age at injury was 29.7 (s.d.=13.4) years. The reasons for referral to the program (some subjects report multiple reasons) were primarily medical (n=74), functional (n=65) and either mobility (n=67) or activities of daily living (n=6) equipment related. A small number of subjects (n=6) were referred for social reasons.
Fatigue severity scale
The mean FSS score was 4.2 (s.d.=1.7), with 52% of the sample scoring greater than the cut score of 4. The mean scores were the highest for the FSS items related to ‘alteration in motivation’ and ‘interference with physical functioning’.
Fatigue-causing medications and FSS scores
From the total list of medications (n=147) that the subjects were taking, clinicians concluded that 41 medications clearly caused fatigue and 102 medications did not. No consensus was reached with four medications: flunarizine, trimebutine, citalopram and Chinese medicine. A total of six subjects took medications from the ‘no consensus’ category; however, because of the potential ambiguity in judging these medications, these data were excluded from analyses. Excluding these individuals from the rest of the analyses did not alter the overall results, so we left these subjects in the study but acknowledge that the ‘no consensus’ medications should be scrutinized for possible effect in larger studies.
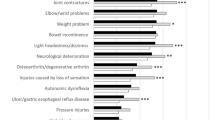
The sample took a mean of 4 (s.d.=2.9) medications, 2 (s.d.=1.6) fatigue-causing medications and 2 (s.d.=2.3) non-fatigue-causing medications. The subjects were split into four groups based on the medications taken: no medications (n=13), only non-fatigue-causing medications (n=23), only fatigue-causing medications (n=31) and both non-fatigue and fatigue-causing medications (n=69). The order of mean FSS scores of the groups was (from highest to lowest) both non-fatigue and fatigue-causing medication group, fatigue only group, no medications group and non-fatigue only group. The fatigue-causing medications were further broken down into functional categories as shown in Table 2. The greatest number of subjects was taking antispasticity medications (n=75) and analgesics (n=61). In the antispasticity category, 28 of the 75 subjects were taking greater than one antispasticity medication, whereas in the analgesic category, 27 of the 61 subjects were taking greater than one analgesic. Twenty-one subjects were taking one antidepressant, six were taking one antipsychotic and three were taking one gastrointestinal medication.
Clinical variables and FSS scores
Variables that were statistically significant when examining fatigue at the bivariable level included presence of pain, presence of spasticity, use of mobility aids, use of fatigue-causing medications, use of fatigue-causing analgesics and use of fatigue-causing medications excluding those for pain. The final regression model accounted for 19% of the variance in the FSS scores was explained by the variables listed in Table 3. The presence of pain (7.6%) and the use of fatigue-causing analgesics (4.2%) explained the most variance in the FSS scores.
Discussion
The majority of our sample had clinically significant fatigue based on their FSS scores, further supporting findings in the literature.2, 3, 4, 5 Our sample of individuals with SCI living in the community took an average of four prescribed medications, often including medications that contribute to fatigue. In fact, the majority used fatigue-causing medications, most commonly analgesics and/or antispasticity medications; however, only the number of analgesics remained statistically significant after controlling for other important variables.
Our second objective was to describe the relationship between medications known to cause fatigue and the FSS. Fatigue seen in individuals with SCI may be a side effect of prescribed medication;12 thus, it is important to look at medications to try to determine their contribution to fatigue in this population. Comparing the four groups of subjects, the group taking both the non-fatigue and fatigue-causing medications had the highest mean FSS score, followed by the group taking fatigue drugs only. It was also found that the no medication group had slightly higher FSS scores than the non-fatigue-causing medications group. These findings support our hypothesis that subjects taking fatiguing medications would have higher fatigue levels. The group taking both non-fatigue and fatigue causing may have had the highest FSS scores because there may have been unrecognized medication interactions or poorly controlled symptoms contributing to fatigue. It is possible that the group taking non-fatigue-causing medications have symptoms that are well controlled with their medications so they feel less fatigued. Although these findings do not establish a causal relationship between medication use and fatigue, the data indicate that clinicians need to be aware that fatigue in their patients is greater if they are taking fatigue-causing medications.
Although fatigue-causing analgesics remained statistically significant in the presence of other confounding factors in predicting fatigue with the FSS, the ‘other’ fatigue-causing medications did not contribute to the explained variance in the regression model. This finding is puzzling to us and could be explained by the fact that some fatigue-causing medications may also have positive effects on medical factors that contribute to fatigue, reducing clinical fatigue overall. For example, perhaps some fatigue-causing medications such as sedatives, antidepressants and antispasticity medications have a positive effect on the individual thereby reducing fatigue. Alternatively, this effect may be a statistical artifact because of the small number of individuals taking these ‘other’ fatigue-causing medications (lack of power) or because of the number of subjects taking analgesics.
There is no known literature investigating the relationship between medication use and fatigue in individuals with SCI and very few studies examining this relationship in other disabled populations. In one study, Oken et al.6 suggest that central nervous system (CNS)-active medications had a statistically significant influence on the general fatigue levels of individuals with multiple sclerosis. In our study, we classified medications as fatigue causing versus non-fatigue causing. Although most CNS-active medications are likely to cause fatigue, there are non-CNS-active SCI medications such as dantrolene that could also cause fatigue.11 By classifying our medications as fatigue causing versus non-fatigue causing, we ensured that we did not miss any potentially non-CNS-active fatigue-causing medications.
There are a number of limitations to our study. Most subjects tended to record only prescription medications on the outpatient questionnaire. We were not able to capture all over-the-counter medications that subjects may have been taking, including herbal remedies, analgesics, energy-inducing medications or caffeine intake (for example drinks or supplements containing caffeine). Moreover, we did not capture other illicit drugs such as marijuana, which may contribute to fatigue, and as outlined earlier, we were unable to obtain consensus regarding the fatigue status of four medications noted in this study. The dosages of medications were not considered as it was difficult to get the correct dosages from the outpatient questionnaires or the subject's chart because of changing dosages. Information regarding the medications was collected through subject self-report, which can be prone to recall bias. In addition, other comorbid medical conditions and complications that may additionally contribute to fatigue, such as sleep disorders, hypothyroidism, depression or medication interactions, may confound the association between medication use and FSS. Finally, we can only generalize our findings to individuals with SCI who are seeking outpatient services; therefore, they might be slightly different from the population as a whole.
Clinicians need to be aware of the fatigue level of individuals with SCI, as it may amplify the negative effects of SCI-related impairments on their physical, cognitive and emotional function and quality of life.3, 13, 14 Routine screening for fatigue using a detailed history and a simple tool such as the FSS can help clinicians determine the presence and severity of fatigue.
Conclusion
Clinically significant fatigue, as determined by the FSS, is prevalent in our sample. Individuals with SCI have multiple impairments that may limit activities and restrict participation. Many medications used in the management of SCI may contribute to fatigue. Although we were not able to establish a causal relationship, it is evident that individuals with SCI who are taking fatigue-causing medications had higher FSS scores. Of the fatigue-causing medications, the majority of patients were taking analgesics and antispasticity medications. These findings may guide clinicians regarding treatment decisions including the consideration of fatigue as a side effect when prescribing medications.
References
Herlofson K, Larsen JP . Measuring fatigue in patients with Parkinson's disease—the fatigue severity scale. Eur J Neurol 2002; 9: 595–600.
Gerhart KA, Weitzenkamp DA, Kennedy P, Glass CA, Charlifue SW . Correlates of stress in long-term spinal cord injury. Spinal Cord 1999; 37: 183–190.
McColl M, Arnold R, Charlifue S, Glass C, Savic G, Frankel H . Aging, spinal cord injury, and quality of life: structural relationships. Arch Phys Med Rehabil 2003; 84: 1137–1144.
McColl M, Charlifue S, Glass C, Lawson N, Savic G . Aging, gender and spinal cord injury. Arch Phys Med Rehabil 2004; 85: 363–367.
Fawkes-Kirby TM, Wheeler MA, Anton HA, Miller WC, Townson AF, Weeks CAO . Clinical correlates of fatigue in spinal cord injury. Spinal Cord 2008; 46: 21–25.
Oken BS, Flegal K, Zajdel D, Kishiyama SS, Lovera J, Bagert B et al. Cognition and fatigue in multiple sclerosis: potential effects of medications with central nervous system activity. J Rehabil Res Dev 2006; 43: 83–90.
Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD . The fatigue severity scale: applications to patients with multiple sclerosis and systematic lupus erythematosus. Arch Neurol 1989; 46: 1121–1123.
Dittner AJ, Wessely SC, Brown RG . The assessment of fatigue: a practical guide for clinicians and researchers. J Psychosom Res 2004; 56: 157–170.
Egner A, Phillips VL, Vora R, Wiggers E . Depression, fatigue, and health-related quality of life among people with advanced multiple sclerosis: results from an exploratory telerehabilitation study. NeuroRehabilitation 2003; 18: 125–133.
Anton HA, Miller WC, Townson AF . Measuring fatigue in persons with spinal cord injury. Arch Phys Med Rehabil 2008; 89: 538–542.
Canadian Pharmacists Association. Compendium of Pharmaceuticals and Specialties 2008: The Canadian Drug Reference for Health Care Professionals. Canadian Pharmacists Association: Ottawa, 2008.
Chadhauri A, Behan PO . Fatigue in neurological disorders. Lancet 2004; 363: 978–988.
Murray RF, Asghari A, Egorov DD, Rutkowski SB, Siddall PJ, Soden RJ et al. Impact of spinal cord injury on self-perceived pre- and postmorbid cognitive, emotional, and physical functioning. Spinal Cord 2007; 45: 429–436.
Barat M, Dehail P, de Seze M . Fatigue after spinal cord injury. Ann Readapt Med Phys 2003; 49: 365–369.
Acknowledgements
We acknowledge the UBC Faculty of Medicine Summer Student Research Program who provided funding to Andrea Lee for this project and the Canadian Institutes of Health Research who provide salary support for Dr Miller.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lee, A., Miller, W., Townson, A. et al. Medication use is associated with fatigue in a sample of community-living individuals who have a spinal cord injury: a chart review. Spinal Cord 48, 429–433 (2010). https://doi.org/10.1038/sc.2009.145
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.145
Keywords
This article is cited by
-
Polypharmacy and adverse drug events among propensity score matched privately insured persons with and without spinal cord injury
Spinal Cord (2018)
-
The course of fatigue after acute spinal cord injury
Spinal Cord (2017)
-
Medication profile and polypharmacy in adults with pediatric-onset spinal cord injury
Spinal Cord (2015)
-
Fatigue in persons with subacute spinal cord injury who are dependent on a manual wheelchair
Spinal Cord (2015)
-
Fatigue in persons who have lived with spinal cord injury for >20 years
Spinal Cord (2013)