Abstract
Study design:
Longitudinal cohort.
Objectives:
To determine whether changes in secondary health conditions (SHC) associated with spinal cord injury (SCI) were effectively modeled from a longitudinal or cross-sectional perspective, and whether the changes in SHCs were attributable to age or years post-injury (YPI).
Setting:
Toronto Rehabilitation Institute, Lyndhurst Centre.
Methods:
Telephone survey methods were used to collect data on (1) demographics, (2) impairment, (3) health status, and (4) self-reported SHCs at two time intervals (1995–1997; 2003–2004) from 344 adults with SCI. Generalized estimating equations were applied to model the longitudinal and cross-sectional effects.
Results:
Health status decreased over time (P<0.0005), whereas the number of SHCs increased (P<0.0001). Regardless of age or YPI, the longitudinal component of aging better predicted SHC occurrence and was associated with spasticity [odds ratio, OR=1.055 (95% confidence interval, CI, 1.018 to 1.093, P<0.01)], kidney problems [OR=1.154 (95% CI, 1.084 to 1.229, P<0.0001)], cardiac problems [OR=1.168 (95% CI, 1.060 to 1.286, P<0.01)], high blood pressure [OR=1.121 (95% CI, 1.058 to 1.188, P<0.0001)], chronic pain [OR=1.058 (95% CI, 1.021 to 1.096, P<0.01)], and arthritis/joint pain [OR=1.113 (95% CI, 1.075 to 1.152, P<0.0001)].
Conclusion:
Within a relatively short period of time, persons with SCI experienced substantive declines in health. The findings suggest that a longitudinal perspective is more sensitive for predicting the risk of self-reported SHCs than a cross-sectional one.
Similar content being viewed by others
Introduction
Despite the increase in the number of studies examining the relationship between aging and secondary health conditions (SHC) after spinal cord injury (SCI), there are several challenges to understanding the nature of this relationship.1 Some problems highlighted by Coll2 include whether changes in SHCs over time are suitably represented by cross-sectional analysis, whether they are related more to age or years-post injury (YPI), and whether the patterns of SHC occurrences are linear or nonlinear. One way of addressing these limitations is the use of relatively novel statistical methods designed to separate the cross-sectional and longitudinal effects within a longitudinal study.3
The separation of aging effects is illustrated in a recent paper by Coll,2 in which generalized estimating equations (GEE) analysis to a longitudinal data set from the National Model Systems SCI database was applied. GEE analysis uses the generalized linear model to estimate more efficient and unbiased regression parameter estimates, as it accounts for data consisting of repeated measures that may be correlated within a subject.4 Coll2 examined whether changes in SHC occurrences across three data collection phases were attributable to longitudinal age (years of aging between data collection intervals), cross-sectional age, or cross-sectional YPI. The models identified that the longitudinal effect of aging was associated with the majority of changes in SHCs over time. That is, regardless of current age or YPI, the outcome changed over time. For instance, the occurrence of pain and stiffness over various body regions (that is shoulder, elbow, hand, and hip) increased in the cohort across the data collection intervals.
When examining whether the changes in outcomes were more associated with age or YPI, the majority of SHCs were not associated with either of these effects. Only shoulder pain/stiffness was associated with age, neck and back pain/stiffness was associated with YPI, and smoking was associated with both age and YPI. As well, the occurrences of certain SHCs were nonlinear (that is, neck and back pain/stiffness, constipation, smoking, and nausea), suggesting that the risk of these SHCs was not constant. The findings of this study highlighted that longitudinal designs are warranted, as the cross-sectional variables failed to detect the effects of aging in predicting the risk of SHCs associated with SCI.
Given the limitations associated with longitudinal designs (for example subject attrition and cohort effects), along with conflicting results between longitudinal and cross-sectional analyses on aging (for example Charlifue et al.,5 Kerr and Thompson6), there is a need to apply analysis techniques that maximize the potential of longitudinal data to clarify how health status in persons with SCI changes over time. The purpose of this study was to (1) describe changes in health status in an aging Canadian cohort of SCI individuals, (2) determine whether changes in SHC occurrences are adequately represented by longitudinal and/or cross-sectional effects, and (3) assess whether these change are associated with cross-sectional age or YPI.
Materials and methods
Participants
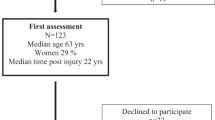
All participants were former patients of Toronto Rehab's Spinal Cord Rehabilitation Program, and were recruited from an existing long-term follow-up database and hospital health records. Data were collected through telephone survey at two time points: 1995–1997 (Time 1) and 2003–2004 (Time 2). At Time 1, data on 851 participants with SCI were collected. However, 176 participants had missing data that could not be verified from hard copies of the questionnaires and were excluded from the analysis. At Time 2, 344 participants were successfully re-contacted (see Table 1). Seventy participants had died, and 261 were lost to follow-up, representing a 38.9% attrition rate.
This study was approved by the Research Ethics Board of Toronto Rehab, and we certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed.
Measures
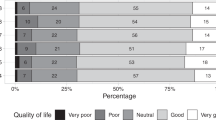
The AT Jousse Long-Term Follow-Up Questionnaire is a nonstandardized survey designed to collect data on (1) socio-demographics, (2) mortality, (3) impairment, (3) health status, (4) SHCs, and (5) mobility. At Time 2, the questionnaire was updated to collect data on quality of life (see Tonack et al.7).
Socio-demographics and impairment
The variables of interest were age, gender, marital status, employment, and level of education (data on education were only collected at Time 2). Impairment data included self-report etiology of injury/disease, date of injury/disease onset, level of injury/lesion, and severity (motor and sensory complete or incomplete).
Health status and secondary health complications
A 10-point numeric scale was used to assess health status, with 1 being ‘poor’ and 10 being ‘excellent’. SHC occurrence(s) were collected by asking participants, ‘Have you had any of the following conditions in the past year?’: spasticity, pressure ulcers, bladder infections, kidney problems, bowel problems, cardiac problems, high blood pressure, respiratory complications, arthritis/joint pain, chronic pain, and psychological distress. Data on additional SHCs were collected at Time 2, and can be found in Hitzig et al.8
Procedure
At the Time 1 interval, data were collected through telephone interview and were stored in a database. Before the Time 2 data collection interval, the data from Time 1 were transferred into a new database system, and data integrity was verified by examining existing hard copies of the Time 1 data case-report forms. The new long-term follow-up database had several programed control checks to minimize data entry error. The data were screened and verified with hard copies of the questionnaire and/or health records.
At the Time 2 interval, information letters were mailed to potential participants, who were then contacted by trained telephone interviewers to obtain informed consent for participation. After the first month of interviews, randomly selected questionnaires were reviewed to assess the reliability and consistency of the data by cross-referencing injury characteristics with the participants' health records. Hospital charts were reviewed to obtain missing data regarding date of birth, date of injury, and/or impairment.
Analysis
Descriptive statistics were used to report the demographic and impairment characteristics of the cohort and the frequency of SHCs at Time 1 and Time 2 (n=344). Chi-square (χ2) analyses and dependent samples t-tests were conducted to assess changes in SHC occurrence and health status. As well, Pearson correlation coefficients were calculated to see whether the total number of SHCs was associated with health status for each time interval: 1995–1997 and 2003–2004, respectively.
We adopted a modeling strategy similar to that of Coll,2 who adapted the models of Neuhaus and Kalbfleisch.3 In our model, age and years post-injury (YPI) were partitioned into cross-sectional and longitudinal components to evaluate whether changes in SHCs were longitudinal in nature or if they could be effectively modeled by cross-sectional analysis. To estimate cross-sectional differences among participants, along with the longitudinal changes within participants, we modeled age by using the chronological age of the participant at Time 1 (Cross-sectional Age) and the time difference between the two interviews (Longitudinal Age). A significant Cross-Sectional Age effect indicates a cross-sectional difference in which participants who differ in age would be expected to also differ in a selected outcome. A significant Longitudinal Age effect reveals that the outcome is better modeled longitudinally, and shows, on average, that a person who gains a year of age can expect to have a changed outcome. If the effects of Cross-Sectional and Longitudinal Age are equal, then the outcome can only be effectively accounted for by using a cross-sectional model. For YPI, we used the YPI of the sample at Time 1. Given the broad age and YPI span of the cohort, the use of first age and YPI, along with the time term (Longitudinal Age), is a suitable means for describing the data.9
On the basis of the earlier stated modeling rationale, GEE were used to investigate whether longitudinal changes in SHCs are represented sufficiently by cross-sectional analysis. For each dichotomous outcome (SHC=1 or absence=0), the effects of Cross-Sectional Age, YPI, and Longitudinal Age were evaluated, while controlling for impairment and employment status. Impairment was dichotomized into severity (complete=0 vs incomplete=1) and level (paraplegia=0 vs tetraplegia=1). Employment status (working=1 and not working=0) was controlled because χ2 analyses detected associations between employment status (at both Time 1 and Time 2) with a number of the SHC outcomes. Further, t-tests revealed that persons who were not working (unemployed or retired) had significantly more SHCs and lower self-perceptions of health than persons who were working (employed and/or student and/or volunteer).
To determine whether the risk of an SHC was related more to age or YPI, an analysis of the models without the Longitudinal Age term was conducted. For these models, a significant age effect indicates that age is the primary factor, whereas the opposite is held true if YPI is significant.
The use of GEE methods is a more appropriate means for analyzing longitudinal data. Longitudinal studies are those in which the outcome variable is repeatedly measured on the same individual on several occasions. As a result, the observations collected over time are not independent of each other, and techniques based on this assumption, such linear or logistic regression analyses cannot be directly used in longitudinal studies.10
Results
Changes in health status
The frequency of each self-reported SHC increased (P<0. 0001) over time except for bowel problems, which decreased (P<0.0001; see Figure 1). The mean total number of SHCs was higher at Time 2 (t (344)=−6.855, P<0.0005; M=4.1; s.d.=1.96) than at Time 1 (M=3.4; s.d.=1.91). Similarly, the mean health status at Time 1 (M=7.3; s.d.=1.82) decreased (t (338)=2.320, P<0.0005) by Time 2 (M=7.1; s.d.=1.76). There was an association between total number of SHCs and perceived health status at Time 1 (r=−0.40; P⩽0.001) and at Time 2 (r=−0.37; P⩽0.001). Hence, poorer perceptions of health were associated with a higher number of self-reported SHCs.
Cross-sectional and longitudinal aging and YPI effects
The resulting odds ratios (ORs; per 1 year of change) from the GEE analysis of the cross-sectional and longitudinal aging and YPI effects are presented in Table 2. When the OR is >1.0, the more likely the event (SHC) is expected to occur with increasing age or YPI. Conversely, when the OR is <1.0, the likelihood of the SHC occurring with increasing age or YPI is low.
More than half of the SHCs examined were positively associated with Longitudinal Age. The outcomes with only significant longitudinal effects included spasticity [OR=1.055 (95% confidence interval, CI, 1.018 to 1.093, P⩽0.01)], kidney problems [OR=1.154 (95% CI, 1.084 to 1.229, P⩽0.0001)], high blood pressure [OR=1.121 (95% CI, 1.058 to 1.188, P⩽0.0001)], chronic pain [OR=1.058 (95% CI, 1.021 to 1.096, P⩽0.01)], and arthritis/joint pain [OR=1.113 (95% CI, 1.075 to 1.152, P⩽0.0001)]. Regardless of YPI or age, the risk for these SHCs increased over time.
Both the longitudinal [OR=1.168 (95% CI, 1.060 to 1.286, P⩽0.01)] and cross-sectional [OR=1.054 (95% CI, 1.020 to 1.089, P⩽0.01)] effects were positive and significant for cardiac complications. Hence, the risk of cardiac problems increases with age and with time.
Only a few cross-sectional effects were detected for the SHCs modeled. For Cross-Sectional Age, a negative association was detected with bladder infections [OR=0.974 (95% CI, 0.974 to 0.990, P<0.01)], whereas a positive association was found with respiratory complications [OR=1.027 (95% CI, 1.004 to 1.051, P<0.05)]. This indicates that the risk of bladder infections decreased with age, whereas the risk of respiratory complications increased. As well, the occurrence of pressure ulcers was positively associated with YPI [OR=1.022 (95% CI, 1.001 to 1.044, P⩽0.05)]. Hence, the risk of having a pressure ulcer increases with duration of SCI.
In regard to whether the change in a particular SHC was related more to age or to YPI, the majority of cross-sectional effects were not significant. Similar to the models including the longitudinal component, positive Cross-Sectional Age effects were detected with cardiac [OR=1.052 (95% CI, 1.019 to 1.085, P<0.01)] and respiratory [OR=1.027 (95% CI, 1.004 to 1.051, P<0.05)] complications. As well, a negative association was found with bladder infections [OR=0.974 (95% CI, 0.958 to 0.990, P<0.01)]. No significant YPI effects were detected.
Discussion
The findings of this study suggest that aging with an SCI, even across a relatively short period of time, is associated with significant decreases in self-reported health status. Within a 5- to 8-year period, the perceived health status of the cohort decreased, whereas the total number and individual number of self-reported SHCs increased. Interestingly, the more frequent but relatively ‘benign’ conditions, such as bladder problems and spasticity, showed smaller increases over time than the less frequent SHCs that have implications for co-morbidities and life expectancy. Although still relatively low, the reports of cardiac complications and high blood pressure doubled between Time 1 and Time 2. This is particularly concerning given the prevalence of metabolic syndrome,11 and the mortality and morbidity associated with cardiac events among persons with SCI.12 Similarly, there were noticeable increases in the frequency of joint/arthritis pain and kidney problems. With regard to the GEE analyses, the regression-adjusted ORs revealed significant and positive associations between Longitudinal Age and the majority of the SHCs examined. Hence, irrespective of age or YPI, the odds of reporting high blood pressure, chronic pain, arthritis/joint pain, spasticity, and kidney problems increased over time for the cohort.
It is difficult to determine whether the increases in these particular SHCs are accelerated because of SCI13 or are normative, as the able-bodied population is also at risk of increased cardiovascular health-related problems, renal impairment, respiratory ailments, and joint/arthritis pain with advancing age.14 There is some compelling evidence for the former,15, 16 but further work is required to clarify these relationships17 and to determine whether they are unique to one body system or consistent across several biological systems.18 Unfortunately, the findings of our study cannot account for the rate of change in SHCs of the cohort, as we only collected data at two time intervals. As a result, we do not know whether the occurrence of these SHCs get progressively worse over time, or whether they follow a nonlinear progression. Regardless, the increase in prevalence of conditions such as musculoskeletal pain can cause greater functional impairments, and can lead to the development of depressive symptoms over time.19
When trying to determine whether the occurrence of a particular SHC was associated more with age or YPI, it was not surprising that the only associations detected were with cardiac and respiratory complications. These SHCs are modeled effectively from a cross-sectional perspective, as they are typical conditions found in the aging able-bodied population as well.14 The finding that pressure ulcers were associated with increased duration of SCI is consistent with other studies, but there are likely other influential factors (for example difficulty with practicing good skin care) contributing to the increased risk of developing a pressure ulcer over time.20 Similarly, there were several associations detected between certain SHCs and impairment (for example a complete injury was associated with pressure ulcers and bladder infections, and spasticity was associated with tetraplegia), indicating that the development of certain conditions (for example bowel problems) is a consequence of the nature and severity of the SCI itself.21
Our findings are comparable to those of Coll,2 whose data were also better represented by longitudinal effects than by the cross-sectional ones. Overall, only three of the self-reported SHCs were associated with Cross-Sectional Age, and none were associated with YPI. However, the magnitude of the longitudinal regression-adjusted ORs predicting the occurrence of an SHC was much higher in Coll's study than in ours. This discrepancy may be attributed to the fact that Coll2 examined a different set of SHCs across three rather than two time intervals, which were of longer duration than those in this study.
There were also methodological limitations that may have affected our conclusions. Our data consist of self-reported impairment and SHC occurrence. Self-report data exclude the clinician perspective, and do not capture the severity or impact of the SHC. Although definitions of study terms were provided to respondents if requested, these were not standardized at either Time 1 or Time 2. We are currently using the Secondary Conditions Scale22 in our current phase of data collection (Time 3) to address these issues.
This study also had problems typically associated with longitudinal designs, including interim participant mortality and attrition, and changes in data collection procedures, which we have outlined in the methods. This study may also be subject to several forms of bias, such as observer expectation bias and reporting bias.23
At this time, we are beginning to understand the implications of aging with an SCI on an individual's health, and the findings of this study highlight that a cross-sectional approach is a limited means for advancing our knowledge on the topic. The use of appropriate statistical methods, such as GEE analysis, in longitudinal studies is critical for identifying whether changes attributed to aging are inherent in living with an SCI or whether there are modifiable risk factors that can be targeted to minimize future problems. The prevalent SHCs associated with aging reported in this study are obvious targets for secondary and tertiary prevention initiatives.
References
Adkins RH . Research issues in aging studies associated with SCI. Top Spinal Cord Inj Rehabil 2001; 6: 128–135.
Coll JR . Cross-sectional and longitudinal effects of aging for the secondary conditions of spinal cord injury. Top Spinal Cord Injury Rehab 2007; 12: 15–22.
Neuhaus JM, Kalbfleisch JD . Between- and within-cluster covariate effects in the analysis of clustered data. Biometrics 1998; 54: 638–645.
Liang KY, Zeger SL . Longitudinal data analysis using generalized linear models. Biometrika 1986; 73: 13–22.
Charlifue SW, Weitzenkamp DA, Whiteneck GG . Longitudinal outcomes in spinal cord injury: aging, secondary conditions, and well-being. Arch Phys Med Rehabil 1999; 80: 1429–1434.
Kerr W, Thompson M . Acceptance of disability of sudden onset of paraplegia. Paraplegia 1978; 10: 94–102.
Tonack M, Hitzig SL, Craven BC, Campbell KA, Boschen KA, McGillivray CF . Predicting life satisfaction after spinal cord injury in a Canadian sample. Spinal Cord 2008; 46: 380–385.
Hitzig SL, Tonack M, Campbell KA, McGillivray CF, Boschen KA, Richards K et al. Secondary health complications in an aging Canadian spinal cord injury sample. Am J Phys Med Rehabil 2008; 87: 545–555.
Morrell CH, Brant LJ, Ferrucci L . Model choice can obscure results in longitudinal studies. J Gerontol A Biol Sci Med Sci 2009; 64A: 215–222.
Twisk JWR . Longitudinal data analysis. A comparison between generalized estimating equations and random coefficient analysis. Eur J Epidemiol 2004; 19: 769–776.
Myers J . Cardiovascular disease after SCI: prevalence, instigators, and risk clusters. Top Spinal Cord Inj Rehabil 2009; 14: 1–14.
Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D et al. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord 2005; 43: 408–416.
Bauman WA, Spungen AM . Disorders of carbohydrate and lipid metabolism in veterans with paraplegia or quadriplegia: a model of premature aging. Metabolism 1994; 43: 749–756.
Aldwin CM, Gilmer DF . Health, Illness, and Optimal Aging. Sage Publications: Thousand Oaks, California, 2004.
Bauman WA, Spungen AM . Body composition in aging: adverse changes in able-bodied persons and in those with spinal cord injury. Top Spinal Cord Inj Rehabil 2001; 6: 22–36.
Garland DE, Adkins RH, Scott M, Singh H, Massih M, Stewart C . Bone loss at the os calcis compared with bone loss at the knee in individuals with spinal cord injury. J Spinal Cord Med 2004; 27: 207–211.
Thompson L, Yakura J . Aging related functional changes in persons with spinal cord injury. Top Spinal Cord Inj Rehabil 2006; 6: 69–82.
Adkins RH . Research and interpretation perspectives on aging related physical morbidity with spinal cord injury and brief review of systems. NeuroRehab 2004; 19: 3–13.
Richardson EJ, Richards JS, Sutphin SM . A longitudinal study of joint pain following SCI: concurrent trends in participation, depression, and the effects of smoking. Top Spinal Cord Rehabil 2007; 12: 45–55.
Garber SL, Rintala DH, Hart KA, Fuhrer MJ . Pressure ulcer risk in spinal cord injury: predictors of ulcer status over 3 years. Arch Phys Med Rehabil 2000; 81: 465–471.
Krause JS . Aging after spinal cord injury: an exploratory study. Spinal Cord 2000; 38: 77–83.
Kalpakjian CZ, Scelza WM, Forchheimer MB, Toussaint LL . Preliminary reliability and validity of a Spinal Cord Injury Secondary Conditions Scale. J Spinal Cord Med 2007; 30: 131–139.
Delgado-Rodríguez M, Llorca J . Bias. J Epidemiol Community Health 2004; 58: 635–641.
Acknowledgements
We thank Dr David Flora of York University (Department of Psychology and the Institute for Social Research) and E Manolo Romero Escobar, PhD Candidate, of York University (Department of Psychology) for their guidance and assistance with the statistical analyses. We also thank Michael Johnson, BA, Jennifer Greves, Dipl., Chad Greene, BSc, Kieva Richards, BSc, and Andrea Brown, BSc for their help on the project. Finally, we thank our participants for their time and support of our work. This project was supported by the Toronto Rehabilitation Institute, which receives funding under the Provincial Rehabilitation Research Program from the Ministry of Health and Long-Term Care in Ontario. The views expressed do not necessarily reflect those of the Ministry.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hitzig, S., Campbell, K., McGillivray, C. et al. Understanding age effects associated with changes in secondary health conditions in a Canadian spinal cord injury cohort. Spinal Cord 48, 330–335 (2010). https://doi.org/10.1038/sc.2009.135
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.135
Keywords
This article is cited by
-
Longitudinal effects of time since injury and age at injury on outcomes of people with spinal cord injury in Queensland, Australia
Spinal Cord (2022)
-
A longitudinal study of self-reported spasticity among individuals with chronic spinal cord injury
Spinal Cord (2018)
-
Impact of health problems secondary to SCI one and five years after first inpatient rehabilitation
Spinal Cord (2017)
-
Prevalence and associated factors of pain in the Swiss spinal cord injury population
Spinal Cord (2017)
-
Medication profile and polypharmacy in adults with pediatric-onset spinal cord injury
Spinal Cord (2015)