Abstract
Objective:
This study aimed to obtain guidelines for choosing between subtotal corpectomy (SC) and laminoplasty (LP) by analysing the surgical outcomes, radiological changes and problems associated with each surgical modality.
Study Design:
A retrospective analysis of two interventional case series.
Setting:
Department of Orthopaedic Surgery, Kagawa University, Japan.
Methods:
Subjects comprised 34 patients who underwent SC and 49 patients who underwent LP. SC was performed by high-speed drilling to remove vertebral bodies. Autologous strut bone grafting was used. LP was performed as an expansive open-door LP. The level of decompression was from C3 to C7. Clinical evaluations included recovery rate (RR), frequency of C5 root palsy after surgery, re-operation and axial pain. Radiographic assessments included sagittal cervical alignment and bone union.
Results:
Comparisons between the two groups showed no significant differences in age at surgery, preoperative factors, RR and frequency of C5 palsy. Progression of kyphotic changes, operation time and volumes of blood loss and blood transfusion were significantly greater in the SC (two- or three-level) group. Six patients in the SC group required additional surgery because of pseudoarthrosis, and four patients underwent re-operation because of adjacent level disc degeneration. In the LP group, the problem of elimination of postoperative axial symptoms remains to be solved.
Conclusions:
The merit of SC is the low frequency of axial symptoms. One-level SC can be considered to have similar degree of invasiveness as LP. Compared with SC, LP is more suitable for elderly patients with multilevel stenosis.
Similar content being viewed by others
Introduction
Surgical treatments for cervical spondylotic myelopathy (CSM) can be broadly divided into anterior and posterior methods. The current mainstream method is subtotal corpectomy (SC), which uses a high-speed air drill to excise the vertebral body for complete decompression of the spinal cord followed by strut bone grafting.1 In laminoplasty (LP), the spinal canal is expanded over a wide region while preserving the posterior elements, and posterior translocation of the spinal cord is possible to achieve decompression.2
Long-term outcomes of both methods have been reported separately.3, 4 However, very few studies have compared the anterior and posterior methods and discussed their advantages and disadvantages.5, 6
At our institution, the first choice of surgical treatment for CSM was, in principle, SC, to expand the spinal canal from an anterior approach7 between 1984 and 1989, but this has been changed to expansive open-door LP from a posterior approach since 1989.2 The objective of this study was to analyse the surgical results, radiological changes, and pre- and postoperative issues associated with SC and LP, to clarify guidelines for selecting the surgical modality.
Materials and methods
Patients
The subjects comprised 83 patients (48 men, 35 women) who underwent surgery for CSM between 1984 and 1999 and were followed for ⩾3 years. A total of 34 patients underwent SC and 49 patients underwent LP. The ages at surgery ranged from 42 to 73 years in the SC group and 39–79 years in the LP group. Mean follow-up duration was 11 years 11 months (range, 3–21 years 2 months) in the SC group and 8 years 3 months (range, 3–15 years 2 months) in the LP group.
Surgical indications and procedures
The severity of myelopathy was evaluated using the Japanese Orthopaedics Association (JOA) score. The JOA score quantifies neurological impairment by evaluating upper extremity function (4 points), lower extremity function (4 points), sensory (6 points) and urinary bladder function (3 points) (Table 1). The maximum score is 17. The evaluation revealed a motor function score of ⩽2 in the upper or lower extremities and total score ⩽12–13.
Spinal cord compression was proven by imaging studies, such as myelography, computed tomography myelography (CTM) and magnetic resonance imaging. In SC conducted in the 1980s, only CTM examination was available. Therefore, in comparing presurgical imaging findings of the two groups, CTM finding were mainly used. The vertical and horizontal diameters of the compressed spinal cord were measured on CTM, and the anterior–posterior compression ratio was calculated. A ratio ⩽40% was defined as compression.
Subtotal corpectomy removed 3 vertebral bodies in 12 patients (C3–7 in all cases), 2 vertebral bodies in 16 patients (C3–6 in 5 cases, C4–7 in 11 cases) and 1 vertebral body in 6 patients (C3–5 in 2 cases, C4–6 in 2 cases, C5–7 in 2 cases).
In all patients, the laminae was expanded from C3 to C7 in the LP group. When the level of compression in the LP group was classified using the same criteria as the SC group, compression involved 4 intervertebral segments (C3/4–6/7) in 16 patients, 3 intervertebral segments in 22 patients (C3/4–5/6 in 10 cases, C4/5–6/7 in 12 cases) and 2 intervertebral segments in 11 patients (C3/4–4/5 in 5 cases, C4/5–5/6 in 4 cases, C5/6–6/7 in 2 cases), with no marked difference in level of compression between the two groups.
For SC by an anterior approach, a high-speed drill was used to remove the vertebral bodies. After decompression, autologous strut bone grafting was carried out. After surgery, a halo vest was worn as external fixation for 12–16 weeks by all patients.7
Laminoplasty was performed as an expansive open-door LP according to the methods described by Hirabayashi et al.2 A neck collar was worn as external fixation for 6–8 weeks after surgery.
Items of clinical evaluation
For clinical evaluation, recovery rate (RR) was calculated from the JOA scores before and after surgery using the formula proposed by Hirabayashi,8 and was assessed at 1, 5 and 12 years after surgery. RR (%)=(postoperative JOA score−preoperative JOA score/normal (17)−preoperative JOA score) × 100. Duration of disease (time from the onset of myelopathy to time of surgery), association of onset with a history of minor trauma (yes versus no), frequency of C5 root palsy after surgery, (operation time (OP) and volumes of blood loss (BL), and blood transfusion (BT) were compared between the LP group and one-, two- and three-level SC groups), re-operation in the cervical region and surgical details, pre- and postoperative axial pain (AP) and shoulder stiffness (yes versus no), and severity were also assessed. AP was assessed on a scale of grades 0–3, referring to the criteria of Yoshida et al.9 (Table 2).
Items of imaging evaluation
Sagittal cervical alignment (SCA) was evaluated on lateral plain radiography taken in neutral position while standing or sitting, and the vertebral body angle θ between the inferior border of the C2 vertebral body and the superior border of the C7 vertebral body was measured using the method described by Cobb.10 A θ angle of 10° or greater was assessed as lordotic (type L), −5° or greater but less than 10° as straight (type S), and less than 5° as kyphotic (type K). In addition, a θ angle greater than 25° or reverse swan neck morphology was assessed as hyperlordotic (type HL) (Figure 1).
Method of measurement of sagittal plane cervical spine alignment. The vertebral body angles (θ) for C2–7 were measured using Cobb's method. θ <5° was assessed as kyphotic, ⩾−5° but <10° as straight, and ⩾10° as lordotic (type K). In particular, θ >25° or exhibiting reverse swan neck alignment was assessed as hyperlordotic (type HL).
The preoperative cervical range of motion was determined by measuring the angles of intersection of the lines passing through the posterior side of the C2 and C7 vertebrae, during flexion and extension, and then adding the two angles.
Bone union was assessed as complete when the gap between the grafted bone and vertebral body became blurred, continuity of trabecular bone was observed, or the anterior curvature angle of the fused vertebrae remained unchanged. Pseudoarthrosis was diagnosed when the above findings were not achieved at ⩾6 months after surgery.
The above parameters were compared between SC and LP groups. For statistical analysis, the χ2-test and Mann–Whitney's U-test, as well as one-way analysis of variance and Scheffe's F-test were used. Values of P<0.05 were considered significant.
Results
Comparison of presurgical characteristics
Mean age at surgery was 60.4±8.4 years in the SC group and 64.8±11.7 years in the LP group, with no significant difference between the two groups. Mean duration of disease was 12.1±10.3 months in the SC group and 17.6±38.1 months in the LP group, and with no significant difference. A history of minor trauma probably associated with disease onset was found in 3 patients (8.8%) in the SC group and 11 patients (22.4%) in the LP group, with no significant difference (Table 3).
Mean preoperative JOA score was 8.6±2.9 in the SC group and 7.9±2.4 in the LP group. Mean scores for upper extremity function, lower extremity function, sensation and urinary bladder function were 2.3±0.8, 1.8±1.0, 2.4±1.7 and 2.1±0.8, respectively, in the SC group, and 2.1±0.9, 1.5±0.8, 2.3±1.3 and 2.1±0.7, respectively, in the LP group. No significant differences between groups were seen in total score or scores for individual items (Table 3).
Mean presurgical range of motion of the cervical spine was 44.3±12.0° in the SC group and 42.0±13.8° in the LP group, with no significant difference between the two groups (Table 3).
Among patients who could be surveyed for AP, preoperative assessment in the SC group (20 patients) was grade 0 in 15 patients, grade 1 in 4 patients and grade 2 in 1 patient, whereas that in the LP group (41 patients) was grade 0 in 19 patients, grade 1 in 16 patients and grade 2 in 7 patients, with no significant differences between groups (Table 3).
Comparison of operative parameters and postoperative outcomes
Mean postoperative RR were 55.5±25.3% in the SC group and 61.4±21.2% in the LP group at 1 year after surgery, with almost the same RR in both groups. At subsequent 5- and 12-year follow-ups, the mean RR were 49.3±29.3 and 41.0±26.6%, respectively, in the SC group, and 52.4±28.1 and 50.9±25.9% in the LP group, with no significant differences between groups (Figure 2). Postoperative C5 palsy occurred in 3 patients in the SC group and 5 patients in the LP group, with no significant difference in prevalence between groups.
Mean OP was (one-level, 265±51 min; two-level, 334±73 min; three-level, 371±89 min) in the SC group and 175±60 min in the LP group. Mean volume of BL was (one-level, 662±553 ml; two-level, 1292±942 ml; three-level, 1818±1607 ml) in the SC group and 404±426 ml in the LP group. Mean volume of BT was (one-level, 487±386 ml; two-level, 917±994 ml; three-level, 1330±1063 ml) in the SC group and 134±318 ml in the LP group. OP was significantly longer in the SC group, and volumes of BL and BT were also significantly greater in the SC group compared with the LP group (P<0.05). When the LP group was compared with the one-level SC group, no significant differences in volumes of BL and BT were seen between the two groups (Figure 3).
Comparison of operation time (OP), amount of blood loss (BL) and volume of blood transfusion (BT) for subtotal corpectomy (SC) and laminoplasty (LP). OP was significantly longer in the SC group. No significant differences were identified in volumes of BL or BT between the one-level SC and LP groups. Asterisk P<0.05. Values are mean±s.d.
Changes in SCA over time were as follows. In the SC group, there were 8 cases of type HL, 19 cases of type L and 7 cases of type S before surgery. In the LP group, there were 14 cases (including 3 cases of reverse swan neck type) of type HL, 26 cases of type L and 9 cases of type S before surgery. No significant differences in the distribution of various types of alignment before surgery were apparent between groups (Figure 4).
Changes in cervical sagittal alignment over time in the subtotal corpectomy (SC) and laminoplasty (LP) groups. Preoperative alignment did not differ significantly between SC and LP groups. Alignment at last follow-up included significantly higher proportions of straight type and kyphotic type in the SC group.
Regarding changes in SCA over time after surgery, in the SC group, the distribution of alignment types at the last follow-up shifted to one case of type HL, nine cases of type L, fifteen cases of type S and nine cases of type K.
In the LP group, distribution of alignment type at the last follow-up shifted to 14 cases (including 5 cases of reverse swan neck type) of type HL, 22 cases of type L, 10 cases of type S and only 3 cases of type K. Comparing postoperative alignment types between groups, the SC group showed significantly (P<0.05) higher proportions of type S and type K at all times of follow-up from 1 year after surgery (Figure 4).
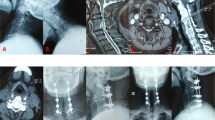
In the SC group, postoperative pseudoarthrosis occurred in 6 of 34 patients. In all the six patients, additional surgery involving posterior interspinous wiring was performed 6–12 months after surgery, and union was eventually completed in all patients. However, in all the six cases, the fused vertebrae were fixed in a kyphotic position. In the SC group, myelopathy due to adjacent level disc damage occurred in 6 of 34 patients. In all the six patients, spinal cord compression occurred at the upper adjacent level. Of the 34 patients, 4 (2 cases of one-level and 2 cases of two-level) were indicated for LP through a posterior approach (Figure 5).
A case of re-operation for adjacent level disc damage. (a) Preoperative plain radiography (lateral view, neutral position). (b) Postoperative plain radiography (lateral view, neutral position). Compared with the preoperative case, angle of lordosis in the fused region has decreased from 25 to 5°. (c) Magnetic resonance imaging after anterior surgery, showing progression of spinal canal stenosis in upper-level vertebrae, resulting in spinal cord compression. (d) Plain radiography after re-operation, showing posterior laminoplasty of C3–7.
Postoperative assessment of AP was grade 0 in 10 patients, grade 1 in 4 patients, grade 2 in 6 patients, and grade 3 in 0 case in the SC group, compared with grade 0 in 9 patients, grade 1 in 10 patients, grade 2 in 11 patients and grade 3 in 11 patients in the LP group. Significantly more intense AP and significantly increased prevalence of AP (P<0.05) were observed in the LP group.
Discussion
As shown in this study, compared with LP, SC achieved similar RR from early after surgery to long-term follow-up. However, two- or three-level SC is more invasive, as indicated by the longer OP and greater volumes of BL and BT. In addition, SCA also showed that many patients shifted to straight or kyphotic type after surgery.
A search of literature found two reports: one by Wada et al.6 in 2001 and the other by Edwards et al.5 in 2002. In these past studies, there was also no difference in postoperative RR between the two methods, but postoperative complications were more frequent in patients who underwent multilevel corpectomy due to the higher level of invasiveness. Edwards et al.5 found no harvest-site pain of autograft and no difference in AP between corpectomy and LP.
In our series, pseudoarthrosis occurred in six patients, and posterior interspinous wiring was performed in all the six cases. Pseudoarthrosis has been reported as a cause of indefinite complaints after surgery and is a factor in poor outcome.11 After harvesting of bone grafts, pain at the site of harvest or fracture of the iliac bone may occur.12 The greater the extent of fusion, the greater the effect on adjacent intervertebral disc, resulting in abnormal mobility, narrowing of intervertebral space and bone spur formation, all of which have been described in many reports.11, 13
Although supplementation with anterior instrumentation is currently being performed to maintain lordotic SCA and improve bone union rate,14 loosening and dislocation of screws and plates and lowered screw fixation in patients with osteoporosis have been reported.15 The surgical indications for CSM patients should be considered with caution, particularly in elderly patients.
Regarding indications for LP, patients exhibiting lordotic SCA reportedly achieve good decompression with this procedure.16 Elderly patients with increased cervical lordosis and marked compression of the posterior elements due to thickening of the yellow ligaments can thus be considered good candidates for LP (Figure 6).17
A 74-year-old woman who underwent expansive open-door laminoplasty. (a and b) Preoperative cervical alignment exhibiting cervical hyperlordosis with lordotic alignment of 42.5°. Magnetic resonance imaging (MRI) reveals multilevel intervertebral narrowing and spinal cord compression involving C3/4, 4/5 and 5/6. (c and d) Imaging findings 3 years after surgery. Cervical lordosis was 31.5°, and MRI shows maintenance of good spinal cord decompression.
Problems of LP include progression of cervical kyphosis and occurrence of delayed myelopathy.18 Intervertebral instability is involved in some cases of worsening of alignment, which can be prevented by combined use of spinal fusion.10 AP including shoulder stiffness and neck pain is another problem, shortening the period of external fixation and range of motion training can reportedly reduce AP.19 In this study, none of the patients who underwent SC had postoperative AP of grade 3 or above. Therefore, SC may be an option in non-elderly patients with preoperative mild lordosis and marked axial discomfort before surgery, if one-level corpectomy can address the condition.
The recent trend is to use a minimally invasive procedure, and to perform LP not necessarily for all five laminae (C3–7), but for four laminae (C3–6) depending on the condition of the patient.20 Considering the ongoing development of even less invasive posterior procedures and the simple postoperative care after laminoplasty, LP should be chosen actively in preference to SC for elderly patients who maintain cervical lordosis and show spinal compression at multiple levels.
Conclusion
The two groups did not differ significantly in various preoperative factors. Surgical outcome assessed by RR also did not differ between groups. The merit of SC is the low frequency of AP. Excluding OP, one-level SC can be considered to have a similar degree of invasiveness as LP. LP is indicated for elderly patients with multilevel stenosis and increased cervical lordosis.
Conflict of interest
The authors declare no conflict of interest.
References
Emery SE, Bohlman HH, Bolesta MJ, Jones PK . Anterior cervical decompression and arthrodesis for the treatment of cervical spondylotic myelopathy. Two to seventeen-year follow-up. J Bone Joint Surg Am 1998; 80: 941–951.
Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y . Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine 1983; 8: 693–699.
Irvine GB, Strachan WE . The long-term results of localised anterior cervical decompression and fusion in spondylotic myelopathy. Paraplegia 1987; 25: 18–22.
Satomi K, Nishu Y, Kohno T, Hirabayashi K . Long-term follow-up studies of open-door expansive laminoplasty for cervical stenotic myelopathy. Spine 1994; 19: 507–510.
Edwards II CC, Heller JG, Murakami H . Corpectomy versus laminoplasty for multilevel cervical myelopathy: an independent matched-cohort analysis. Spine 2002; 27: 1168–1175.
Wada E, Suzuki S, Kanazawa A, Matsuoka T, Miyamoto S, Yonenobu K . Subtotal corpectomy versus laminoplasty for multilevel cervical spondylotic myelopathy: a long-term follow-up study over 10 years. Spine 2001; 26: 1443–1448.
Okada K, Shirasaki N, Hayashi H, Oka S, Hosoya T . Treatment of cervical spondylotic myelopathy by enlargement of the spinal canal anteriorly, followed by arthrodesis. J Bone Joint Surg Am 1991; 73: 352–364.
Japanese Orthopaedics Association. Scoring system for cervical myelopathy. Nippon Seikeigeka Gakkai Zasshi 1994; 68: 490–503.
Yoshida M, Tamaki T, Kawakami M, Nakatani N, Ando M, Yamada H et al. Does reconstruction of posterior ligamentous complex with extensor musculature decrease axial symptoms after cervical laminoplasty. Spine 2002; 27: 1414–1418.
Shibuya S, Oka S, Arima N, Sugata Y, Norimatsu T . Expansive open-door laminoplasty for cervical myelopathy: Characteristics of pre-operative cervical alignment and surgical results. Rinshou Seikeigeka 2003; 38: 1069–1075. (Jpn).
Yonenobu K, Okada K, Fuji T, Fujiwara K, Yamashita K, Ono K . Causes of neurologic deterioration following surgical treatment of cervical myelopathy. Spine 1986; 11: 818–823.
Hu RW, Bohlman HH . Fracture at the iliac bone graft harvest site after fusion of the spine. Clin Orthop Relat Res 1994; 309: 208–213.
Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K . Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine 1993; 18: 2167–2173.
Wang JC, McDonough PW, Endow KK, Delamarter RB . Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine 2000; 25: 41–45.
Ryken TC, Clausen JD, Traynelis VC, Goel VK . Biomechanical analysis of bone mineral density, insertion technique, screw torque, and holding strength of anterior cervical plate screws. J Neurosurg 1995; 83: 325–329.
Sodeyama T, Goto S, Mochizuki M, Takahashi J, Moriya H . Effect of decompression enlargement laminoplasty for posterior shifting of the spinal cord. Spine 1999; 24: 1527–1532.
Shibuya S, Oka S, Arima N, Maruiwa H, Chiba K, Watanabe M et al. Pathophysiology and operative results of cervical spondylotic myelopathy in elderly patients. Rinshou Seikeigeka 2002; 37: 401–407. (Jpn).
Maruiwa H, Chiba K, Watanabe M, Shibuya S, Oka S, Arima N et al. Long-term results of expansive open-door laminoplasty for cervical spondylotic myelopathy. Rinshou Seikeigeka 2000; 35: 411–416.
Kawaguchi Y, Kanamori M, Ishiara H, Nobukiyo M, Seki S, Kimura T . Preventive measures for axial symptoms following cervical laminoplasty. J Spinal Disord Tech 2003; 16: 497–501.
Hosono N, Sakaura H, Mukai Y, Fujii R, Yoshikawa H . C3-6 laminoplasty takes over C3-7 laminoplasty with significantly lower incidence of axial neck pain. Eur Spine J 2006; 15: 1375–1379.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shibuya, S., Komatsubara, S., Oka, S. et al. Differences between subtotal corpectomy and laminoplasty for cervical spondylotic myelopathy. Spinal Cord 48, 214–220 (2010). https://doi.org/10.1038/sc.2009.114
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.114