Abstract
Study design:
A case report.
Objectives:
To report and discuss a case of pseudoaneurysm of the aortic arch presenting as hemoptysis following a cervical spondylodiscitis. The pseudoaneurysm was remote and any direct extension of the abscess was not observed from the cervical lesion.
Setting:
Hamamatsu Medical Center.
Case report:
A 73-year-old male being treated with antibiotics for a cervical spodylodiscitis deteriorated tetraplegia. Following a posterior decompression of the cervical spine and subsequent neurological recovery, hemoptysis occurred and a pseudoaneurysm of the aortic arch was identified. Emergent vascular graftings combined with dèbridement of the pseudoaneurysm and the infected cervical intervertebral disc were performed. The patient recovered gradually and the cervical spondylodiscitis disappeared.
Conclusions:
The septicemia originating from the remote cervical spondylodiscitis was thought to contribute to this pseudoaneurysm. Attention should be paid to the systemic septicemia as well as the focal spinal infection. As for cervical spondylodiscitis, posterior decompression without drainage cannot be recommended as the initial treatment.
Similar content being viewed by others
Introduction
Mycotic pseudoaneurysm was defined as a dilation of an arterial wall resulting from infection.1 Mycotic pseudoaneurysms concomitant with spinal osteomyelitis were usually the result of direct abscess extension2, 3 from the adjacent spinal lesion and were diagnosed easily. Here, we report on a rare case of pseudoaneurysm of the aortic arch following a remote cervical spondylodiscitis.
Case report
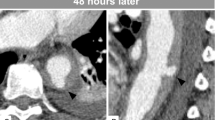
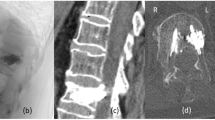
A 73-year-old male was admitted for a severe neck pain concomitant with high fever. He had no history of disease except hypertension. The findings of the neurological examination were normal. Laboratory screening showed leukocytosis (18.4 × 103 per 100 ml) and marked elevation of C-reactive protein (22.63 μg per 100 ml). Magnetic resonance imaging (MRI) revealed a pus-like mass originating from the C5/C6 disc. Therefore, cervical spondylodiscitis was diagnosed. Klebsiella pneumoniae was detected in the blood culture, and ceftriaxone was administered. On the fifth day in hospital, the patient began to complain of hypesthesia and weakness of his hands. Next day, the weakness progressed to the forearms, arms and to the lower limbs as well. The second MRI revealed an epidural abscess extending into the spinal canal (Figure 1). Emergent decompression surgery was performed that evening. Through a posterior approach, double hinge laminoplasty was performed at C3–C7. Suction was attempted through the posterolateral corner of the spinal canal; however, the needle could not reach the abscess. On the seventh day in hospital, the muscle power in his extremities began to recover. However, leukocytosis (11.0 × 103 per 100 ml) and C-reactive protein elevation (10.35 μg per 100 ml) persisted despite continuous ceftriaxone treatment. A third MRI revealed a remaining abscess surrounding the C5/C6 disc. We therefore planned an additional anterior débridement and fusion of the C5/C6. On the seventeenth day, the patient began to complain of bloody sputum. He did not complain of any chest or back pain; however, the frequency and the amount of hemoptysis increased. A chest X-ray showed a saccular shadow, which was not seen on admission in the left upper pulmonary lobe (Figure 2). A thoracic computed tomography scan confirmed a ruptured aortic arch at a calcified wall (Figure 3). The cervical surgery was replaced with an emergent vascular treatment. Vascular grafts were placed first by vascular surgeons from the ascending aorta to the bilateral femoral arteries. Then the ruptured aortic arch and surrounding pulmonary parenchyma were removed. They were not obviously infected. Following these procedures, orthopedic surgeons performed the anterior débridement of the cervical spine. A volume of 5 ml of yellow serous fluid erupted from the C5/C6 disc. Because ventricular fibrillation occurred, bone graft was not performed. The patient was transferred to the intensive care unit immediately after the skin closure and his cardiovascular condition improved gradually. Bacterial examination of the aortic arch was negative. A Gram-positive organism was detected from the cervical pus, but was not specifically identified because the amount of the organism was very small. Within 3 months C-reactive protein decreased to a normal level. Cervical MRI revealed the disappearance of the abscess. The patient had hypesthesia in both hands, but could walk using a cane. No recurrence of infection has been seen for 2 years postoperatively.
Discussion
There has been no report of a case of mycotic pseudoaneurysm remote from the spinal infection site, especially from the cervical spine. The athelosclerotic lesion of the aorta could have caused it accidentally. The patient though had been quite healthy and had no history of any cardiovascular event before admission. Atherosclerotic plaques or direct vascular injury facilitates colonization by circulating organisms.4 This saccular appearance which developed during hospitalization is very characteristic of mycotic pseudoaneurysm.5 Considering these circumstances, we speculate that the septicemia originating from cervical spondylodiscitis contributed to this pseudoaneurysm. Actually, the organism detected from the cervical pus was different from Klebsiella. We speculate that continuous cefriaxone treatment for 2 weeks obscured the bacterial test. The collected pus was approximately 5 ml; however, we could detect only a very small amount of Gram-positive organism. This might be due to a contamination.
Infections in the cervical spine have a higher risk of complications, and surgical treatment is often required in addition to antibiotic therapy. Because of the rapid progress of the paralysis, we chose a laminoplasty to rescue the whole spinal cord first. The posterior components were compromised by this laminoplasty and subsequent spinal instability might have prolonged the spondylodiscitis as well as the septicemia. Anterior drain with fusion should be done earlier.
Conclusion
Although mycotic pseudoaneurysm is a very rare complication of spondylodiscitis, the mortality rate is very high.3 As for cervical spondylodiscitis, posterior decompression without drainage cannot be recommended as the initial treatment.
References
Osler W . The Gulstonian lectures on malignant endocarditis. Br Med J 1885; 1: 467–469.
Rubery PT, Smith MD, Cammisa FP, Silane M . Mycotic aortic aneurysm in patients who have lumbar vertebral osteomyelitis: a report of two cases. J Bone Joint Surg Am 1995; 77: 1729–1732.
McHenry MC, Rehm SJ, Krajewski LP, Duchesneau PM, Levin HS, Steinmuller DR . Vertebral osteomyelitis and aortic lesions: case report and review. Rev Infect Dis 1991; 13: 1184–1194.
Scheld WM, Sande M . Endocarditis and intravascular infections. In: Mandell GL, Douglas RG, Bennet JE (eds). Principles and Practice of Infectious Diseases, 3rd edn. Churchill Livingstone: New York, 1990, pp 670–706.
Kirkpatrick JN, Ring M, Lang RM . Expanding the differential diagnosis of hemoptysis: mycotic aortic aneurysms. Rev Cardiovasc Med 2003; 4: 180–183.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Satake, K., Iwase, T., Kouyama, A. et al. Pseudoaneurysm of the aortic arch associated with cervical spondylodiscitis. Spinal Cord 46, 762–764 (2008). https://doi.org/10.1038/sc.2008.78
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.78