Abstract
Study Design:
Case series.
Objectives:
To evaluate the risk of pump- and catheter-related complications of intrathecal drug delivery systems.
Setting:
Tertiary care center in Switzerland.
Methods:
The medical records of all in- and out-patient adults treated at our institution during a 12-year period were reviewed. All patients that had received intrathecal drug therapy via an implanted pump were invited to a structured interview.
Results:
One hundred patients, representing therapy with 175 implanted pumps and 132 intrathecal catheters over 552 years, participated in the study. During the observation period, 217 surgical procedures (including 100 primary pump implants) and 5863 pump refills were performed. The annual rate for complications requiring surgical measures was 10.5%, with 35% being pump related and 65% being catheter related. The incidence of infections in our patients was 0.7% per year; all infections appeared during the first 3 months after implantation of the first pump.
Conclusions:
Complication rates of the patients treated in our center, where we have long-term experience with the indication, implantation and continuous care of patients with intrathecal infusion systems, are in the lowest ranges when compared with other published studies. We consider intrathecal testing before implantation, standardized perioperative procedures and consequent long-term care of the patients in a specialized outpatient clinic to be essential factors for the avoidance of complications.
Similar content being viewed by others
Introduction
Spasticity is a common symptom of patients suffering from spinal cord injury, multiple sclerosis, primary lateral sclerosis, cerebral palsy and other neurological diseases. Some of these patients are unresponsive to oral antispastic therapy or experience intolerable side effects. The idea to treat these patients by direct application of the drug to the site of pharmacological action, and thus increase beneficial effects while lessening side effects, is promising. After Wang published a study on continuous intrathecal application of morphine for the treatment of chronic pain,1 Penn and Kroin were the first to describe the treatment of severe spasticity using intrathecal baclofen in 1984.2, 3
Meanwhile, a series of studies has shown the effectiveness of continuous intrathecal therapy for both spinal or cerebral spasticity3, 4, 5, 6, 7, 8 and chronic pain.9 The inadequate efficacy and intolerable side effects of oral and transdermal pharmacotherapy for the relief of symptoms in a considerable proportion of patients have led to the increased popularity of intrathecal therapies over the past two decades.
The Swiss Paraplegic Centre is one of the worldwide largest centers for the acute care and rehabilitation of patients with spinal cord injuries. Patients with chronic pain disorders and other neurological diseases are also treated in our institution; therefore, experience with the indication, implantation and long-term care of patients with implanted pump systems covers more than 15 years. Implanted systems for intrathecal drug therapy, like any other medical device, expose patients to specific problems and adverse events. Furthermore, the limited battery capacity of electric systems leads to foreseeable, repetitive surgical procedures. To evaluate battery longevity, the risk of pump- or catheter-related complications and their possible triggers, we retrospectively studied the patient cohort treated at our hospital.
Methods
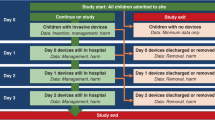
We reviewed the charts of all in- and out-patient adults that were treated at our institution during a 12-year period from January 1992 to December 2003. All charts of patients that had received intrathecal drug therapy via an implanted pump were analyzed. Data were requested from other hospitals only if the patient reported a pump- or catheter-related surgical procedure performed outside our center.
All identified patients were invited in written form to a structured interview. Nonresponding patients were contacted by phone. For patients interested in participating, but refusing a personal visit, the interview was completed over the telephone. Besides demographic and medical details, we asked for information on:
-
date and indication for the first implantation of a pump system;
-
date and indication for all following surgical procedures relating to the pump or catheter;
-
time interval between pump refills during the last year.
All answers were directly verified using the data from the patient's medical record. Data from patients not participating in the interview were obtained from patients' records. Replacement of a pump due to battery exhaustion after the expiration of 3 years was not considered to be a pump-related complication, because the lifespan of battery driven devices is limited.
Statistics
Results are expressed as mean, minimum and maximum. The relationship between two variables was tested using Pearson's product-moment coefficient. For comparison of two groups, the two-tailed t-test for independent samples was used. Differences were considered statistically significant for P<0.05. To illustrate the lifespan of pumps and catheters, a Kaplan–Meier estimator was used.
Standardized implantation procedures
At our institution, standardized procedures for the indication, the surgical procedure of implantation and the continuous refills of pumps are established. Patients are selected for evaluation after at least a 6-week trial, where the patient cannot be maintained on noninvasive methods of spasm/pain control, such as oral antispasmodic or analgesic drugs, either because these methods fail to adequately control the spasticity/pain or produce intolerable side effects. After additional psychiatric evaluation, the effectiveness of intrathecal drug therapy is tested with continuous application of the intrathecal medication via a percutaneous lumbar microcatheter and an external syringe pump for several days. During a stay as an in-patient, the oral medication is reduced and finally terminated. The response is considered acceptable if pain relief (including effects on the activities of daily living tested by our physiotherapists) and patient acceptance are good and the degree of side effects is tolerable. The temporary spinal catheter (usually inserted at the L4/5 or L5/S1 level) is removed and a permanent catheter (typically inserted at the T12/L1 level) and a pump are implanted. For 24 h, patients receive antibiotic prophylaxis with cefazolin and bed rest. Pumps are filled before implantation, with first refills not earlier than 14 days postoperatively. Pumps are refilled only by specially trained employees of our pain clinic, using sterile refill kits offered by the pump manufacturer.
Statement of ethics
The authors certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
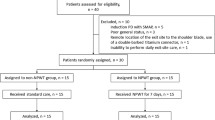
In total, 142 patients meeting the inclusion criteria were identified. The invitation to participate in the interview was accepted by 100 patients. Of the remaining 42 patients, 7 had died, 3 had moved abroad, to 5 the letter could not be delivered because the address was unknown and the remaining 27 refused to participate in the study. Six of the deceased patients died outside our institution, and we are unaware of their causes of death. One patient suffering from multiple sclerosis died from progression of this neurological disease.
The average age of the 42 patients (25 male, 17 female) not participating in the interview was 56 years. Data from this group included 48 pumps and 45 catheters, representing a total of 199 years. The average time to pump replacement due to battery exhaustion was 56 months. There were 18 surgical procedures due to 3 infections, 4 pump dysfunctions, 1 pump revision due to cicatrization and 10 catheter replacements. In the patients who were not interviewed, the annual rate for complications requiring surgical measures was 9.0%. There were no statistically significant differences between the group participating in the interview and the refusal group.
Demographic data from the 100 interviewed patients are listed in Table 1; the age of the participating men and women did not differ. The underlying diseases of the patients are listed in Table 2. Patients stated spasticity to be the major indication for pump implantation in 38 cases, pain in 48 cases and both spasticity and pain in 14 cases.
During the observational period, 46 of the patients had one pump, 36 had two pumps, 15 had three pumps and 3 had four consecutive pumps. Over the same time, 75 of the patients had one catheter, 19 had two catheters, 5 had three catheters and 1 had four catheters. In total, we present data on 175 implanted pumps and 132 intrathecal catheters, representing a total of 552 years (6623 months) of pump system experience. During this time, a total of 5863 pump refills have been performed.
The total number of surgical procedures (including 100 primary pump implants) was 217. The indications for surgical procedures due to pump or catheter dysfunction are listed in Table 3. In nine cases, multiple measures, such as explantation of pump and catheter due to infection or the correction of a pump position when pump replacement was necessary due to battery exhaustion, were reported. Pump replacement due to battery exhaustion was necessary after an average of 55 months. The total number of device-related complications was 58 (126 indications listed in Table 3, minus 4 infections affecting both devices, minus 64 pump changes due to battery exhaustion) in 552 years (10.5% per year). Of these complications, 35% were pump-related (14 pump defects, 4 pump revisions, 4 pump infections) and 65% were catheter-related (36 catheter defects, 4 catheter infections). The lifespan of all implanted pumps is plotted in Figure 1, the lifespan of all implanted catheters is plotted in Figure 2.
All infections appeared during the first 3 months, between the 20th and the 80th day after pump implantation. In all cases, patients after implantation of their first pump system were affected. Medical procedures were at the origin for three of the catheter leaks. In the first case, the catheter was damaged during the implantation of an electrode for a bladder stimulator; in the second case, the catheter was damaged during a paravertebral infiltration with a local anesthetic in an external ambulatory service. In the third patient, the catheter showed a number of holes during the revision because it had formed a loop in front of the pump and had obviously been hit several times when the pump was refilled.
In the vast majority of patients, programmable pumps (Medtronic 8615, Medtronic Inc., Minneapolis, MN, USA) with a reservoir volume of 18 ml were used, and only seven of the pumps were models with a reservoir volume of 10 ml. The distribution of the annual frequency of pump refills is shown in Table 4. There was no correlation between the number of pump refills and the lifespan of the battery (r=−0.018) or the number of necessary surgical procedures (r=−0.030). Patients who had pain as the major indication for pump implantation had a higher frequency of pump refills than patients with spasticity (P=0.033).
Discussion
The presented data on 100 adults treated in one center with intrathecal medication via an implanted pump are, as to our knowledge, the most extensive and accurate information on the frequency of complications available to date. Comparing data from different studies is difficult because the results often describe very different time periods. We therefore decided to calculate and use the number of complications per year of treatment for comparison.
Several studies on 40–232 cases of adult patients with intrathecal drug delivery systems have been published. They showed complications requiring surgical measures with an annual frequency ranging from 10.9 to 49.4%. The infection rate per year was between 0.7 and 5.2%.3, 7, 10, 11, 12, 13, 14, 15 With a total observation period of 552 pump years, our study unequivocally covers the longest observation period. The annual rate for complications requiring surgical measures was 10.5%.
The annual rate of infections in our patients was 0.7%; however, due to the fact that only first implants between day 20 and day 80 were affected, a rate of 4% for the first year and 0% in the following years gives a more realistic picture. Other authors published annual infection rates varying between 0.7 and 10.3%.3, 7, 10, 11, 12, 13, 14, 15 These infection rates have to be compared with the infection rates of other procedures involving surgical implants, for example, between 0 and 6% (averaging 1.3–2.5% in a risk population) after hip or knee prosthesis in various American hospitals.16
The 64 routine pump exchanges due to battery exhaustion were performed after an average of 55 months. Other studies found equal time periods of 55–58 months.3, 10 The newest generation of programmable pumps developed by the same manufacturer are said to have a 5–24% longer battery lifespan, which could positively influence the number of surgical procedures per patient in the future. The frequency of pump refills correlates directly with the output that has to be delivered by a pump, and because every refill requires a reprogramming (which is also energy consuming), we expected a shorter lifespan in patients with high refill frequencies. This was not the case, as it seems that time since implantation is a more important factor.
The frequency of pump refills was between 4 (which is the fixed minimum, due to the limited activity of the drugs when stored in the reservoir of the pump) and 100 per year. When pain was the indication for intrathecal therapy, pump refills were clearly more frequent than in patients with spasticity. One reason might be that baclofen has a therapeutic effect in very small dosages in patients with multiple sclerosis.10 Another reason could be the drug mix frequently used for the treatment of chronic pain, which inevitably leads to a reduced concentration of the single components of the mixture. Only limited data are available on the long-term dose increase in patients with intrathecal therapy for pain and spasticity. One study observing 16 pain patients reported a ninefold increase in the daily morphine dosage after 2 years,17 while in a larger study of 120 patients an increase of only 74% after 3.4 years was reported.18 However, in 40 patients treated for spasticity, a 2.6-fold increase of the daily baclofen dosage was found.7 In any case, the difference in refill frequencies could also be explained due to a difference in the magnitude of increased dosages over time.
Each pump refill requires a transcutaneous puncture with a noncoring port access device needle. Although each of these punctures is potentially a source of infection, none of our patients suffered a pump or catheter infection over the long period. We also found no correlation between the frequency of refills and the rate of other complications. A possible reason for this is the consequent use of a standardized and sterile procedure when pumps are refilled in a specialized ambulatory care facility.
Some of the catheter complications were avoidable. Iatrogenic punctures damaging the catheter could be prevented by better information for other therapists about the existence of an implanted pump and catheter system and about the course of the catheter. Also, the occlusion of the catheter when a pump is twisted several times in the same direction seems to be an avoidable complication. One of the affected patients told the interviewer that he had been manually manipulating the pump (twiddler's syndrome). Besides better information of patients about the resulting complications, an improved fixation of the pump could also help to reduce the complication rate.
As in many other studies,3, 7, 11, 12, 13, 14, 15 we also observed a series of catheter disconnections at the pump. The pump manufacturer introduced a new connection technology in 2007, and it will be interesting to see whether this will improve the rate of catheter disconnections in the future.
Exclusion of the 42 patients not interviewed may have biased the results. Although there is a minor trend of increased infections and less overall complications in the group refusing participation, the groups are not statistically different from each other. However, additional information on complications treated outside our center gathered with the aid of a structured interview may have made the study more robust and resulted in some significant differences between the groups. Therefore, it remains unclear whether the calculated complication rates of the 100 participating patients underestimated the actual complication rates.
Conclusions
Direct application of a drug to the site of pharmacological action necessitates the use of complex medical devices. Surgical procedures in conjunction with these implants expose patients to the risk of specific problems and adverse events. When compared with the infection risks of other surgical procedures, these risks seem to be acceptable. Battery-driven programmable pumps have to be replaced every 55 months, a time interval that will hopefully be significantly longer with new pump models.
Complication rates in patients treated in our center with long-term experience in the indication and implantation of intrathecal infusion systems and continuous care of patients with such devices are in the lowest ranges when compared with published studies. We consider intrathecal testing before implantation, standardized perioperative procedures and consequent long-term care of the patients in a specialized ambulatory care facility to be essential factors for the avoidance of complications.
References
Wang JK, Nauss LA, Thomas JE . Pain relief by intrathecally applied morphine in man. Anesthesiology 1979; 50: 149–151.
Kroin JS, Penn RD, Beissinger RL, Arzbaecher RC . Reduced spinal reflexes following intrathecal baclofen in the rabbit. Exp Brain Res 1984; 54: 191–194.
Penn RD . Intrathecal baclofen for spasticity of spinal origin: seven years of experience. J Neurosurg 1992; 77: 236–240.
Burns AS, Meythaler JM . Intrathecal baclofen in tetraplegia of spinal origin: efficacy for upper extremity hypertonia. Spinal Cord 2001; 39: 413–419.
Campbell WM, Ferrel A, McLaughlin JF, Grant GA, Loeser JD, Graubert C et al. Long-term safety and efficacy of continuous intrathecal baclofen. Dev Med Child Neurol 2002; 44: 660–665.
Creedon SD, Dijkers MPJM, Hinderer SR . Intrathecal baclofen for severe spasticity: a meta-analysis. Int J Rehabil Health 1997; 3: 171–185.
Plassat R, Perrouin Verbe B, Menei P, Menegalli D, Mathe JF, Richard I . Treatment of spasticity with intrathecal Baclofen administration: long-term follow-up, review of 40 patients. Spinal Cord 2004; 42: 686–693.
Sampson FC, Hayward A, Evans G, Morton R, Collett B . Functional benefits and cost/benefit analysis of continuous intrathecal baclofen infusion for the management of severe spasticity. J Neurosurg 2002; 96: 1052–1057.
Turner JA, Sears JM, Loeser JD . Programmable intrathecal opioid delivery systems for chronic noncancer pain: a systematic review of effectiveness and complications. Clin J Pain 2007; 23: 180–195.
Avellino AM, Loeser JD . Intrathecal baclofen for the treatment of intractable spasticity of spine or brain etiology. Neuromodulation 2000; 3: 75–81.
Coffey JR, Cahill D, Steers W, Park TS, Ordia J, Meythaler J et al. Intrathecal baclofen for intractable spasticity of spinal origin: results of a long-term multicenter study. J Neurosurg 1993; 78: 226–232.
Follett KA, Hitchon PW, Piper J, Kumar V, Clamon G, Jones MP . Response of intractable pain to continuous intrathecal morphine: a retrospective study. Pain 1992; 49: 21–25.
Guillaume D, Van Havenbergh A, Vloeberghs M, Vidal J, Roeste G . A clinical study of intrathecal baclofen using a programmable pump for intractable spasticity. Arch Phys Med Rehabil 2005; 86: 2165–2171.
Rawlins PK . Intrathecal baclofen therapy over 10 years. J Neurosci Nurs 2004; 36: 322–327.
Teddy P, Jamous A, Gardner B, Wang D, Silver J . Complications of intrathecal baclofen delivery. Br J Neurosurg 1992; 6: 115–118.
National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control 2004; 32: 470–485.
Kumar K, Hunter G, Demeria DD . Treatment of chronic pain by using intrathecal drug therapy compared with conventional pain therapies: a cost-effectiveness analysis. J Neurosurg 2002; 97: 803–810.
Winkelmüller M, Winkelmüller W . Long-term effects of continuous intrathecal opioid treatment in chronic pain of nonmalignant etiology. J Neurosurg 1996; 85: 458–467.
Acknowledgements
This study was supported by an unrestricted grant from Medtronic Inc., Switzerland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Flückiger, B., Knecht, H., Grossmann, S. et al. Device-related complications of long-term intrathecal drug therapy via implanted pumps. Spinal Cord 46, 639–643 (2008). https://doi.org/10.1038/sc.2008.24
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.24
Keywords
This article is cited by
-
Interaction between a smartphone and intrathecal baclofen pump case report
Spinal Cord Series and Cases (2023)