Abstract
Study design:
Cross-sectional, observational study.
Objectives:
To quantify, in adults with chronic spinal cord injury (SCI): (1) presence of metabolic syndrome versus the general North American population (GP) and (2) 10-year coronary heart disease (CHD) risk using Framingham risk scoring (FRS).
Setting:
Ontario, Canada.
Methods:
Fasting anthropometric and biochemical data were collected from 75 adults with chronic SCI. Metabolic syndrome was determined using four internationally recognized definitions and FRS using the most recent (2001) algorithm.
Results:
Prevalence of metabolic syndrome was up to 5.4 times lower in SCI participants compared to GP, and FRS categorized 3.1% of participants as being at high 10-year CHD risk. However, high-sensitivity C-reactive protein (CRP) values indicated 36.7% of participants as being at high CHD risk.
Conclusion:
Current metabolic syndrome definitions and FRS may underestimate true CHD risk in people with SCI. Tools that better identify CHD risk require validation in the SCI population. CRP may be a potential factor to consider in the development of SCI-specific screening tools.
Similar content being viewed by others
Introduction
Medical advances in acute management of traumatic spinal cord injury (SCI) have resulted in an increased lifespan in this population. While encouraging, cardiovascular diseases (CVD) have become one of the leading causes of death in long-term SCI1 with increased rates of morbidity related to CVD, particularly coronary heart disease (CHD), relative to the able-bodied (AB) population.2 Persons with SCI experience body composition changes (decreased lean body mass, increased fat mass) and more sedentary lifestyles than AB persons,3 as well as increased rates of impaired glucose tolerance, insulin resistance and diabetes and reduced high-density lipoprotein cholesterol (HDL-C).2 All of these may explain the increased risk for CVD.
Despite these metabolic changes, there are currently no clinically relevant, validated tools to identify adults with SCI at risk for CHD. Practical screening tools such as Framingham Risk Scoring (FRS) or diagnosis of metabolic syndrome may simplify identification of persons with SCI at high CHD risk. Only two studies have identified the prevalence of metabolic syndrome in persons with SCI. Relative to AB populations, the prevalence in SCI was either lower4 or no different.5 However, despite the multitude of metabolic syndrome definitions in the literature, both Lee et al. and Liang et al. used only one definition; the National Cholesterol Education Panel (NCEP)6 and the National Heart Lung and Blood Institute/American Heart Association (NHLBI/AHA),7 respectively. In addition, neither research group reported FRS.
Should tools such as FRS and/or metabolic syndrome definitions help to identify CHD risk, health care interventions could be provided in a more timely manner, potentially leading to improved prevention and/or treatment in this high-risk population. The objectives of our study were to (1) quantify metabolic syndrome in adults with chronic SCI using four internationally recognized definitions and to compare these to metabolic syndrome in the general North American population (GP) and (2) quantify 10-year CHD risk using the most recent (2001) FRS algorithm.
Materials and methods
Participants
The Study of Health and Activity in People with Spinal Cord Injury (SHAPE-SCI) was a multicenter study in Ontario, Canada, the purpose of which was to determine the role of physical activity in the health and quality of life of people with SCI, and for which the complete methodology has been published.8 The chronic disease risk factor data reported herein were collected from a subset of SHAPE-SCI participants, all of whom lived within a 200 km radius of Hamilton, Ontario, Canada. Eligible participants were ⩾18 years of age and had experienced a traumatic SCI at least 12 months prior to study enrollment. The SHAPE-SCI and substudy protocols were approved by the Research Ethics Boards of Hamilton Health Sciences and University of Guelph, Ontario, Canada. All study participants gave written, informed consent, and substudy participants were provided with a nominal honorarium for participation.
Methods
Substudy data collection took place in participants’ homes. Demographics (sex, age, ethnicity), level and completeness of spinal cord lesion, and brief family and personal medical histories (including information on current medications) were collected from each participant by trained interviewers using a structured questionnaire. All anthropometric measurements were completed by two trained research assistants, after participants had fasted for at least 10 h. Each measure was taken twice and averaged if individual measures differed by ⩽5%. If the difference was >5%, a third determination was made and the two closest measures were averaged. Participants were weighed in light clothing and wearing no shoes, using a portable, digital, wheelchair scale (Health O Meter 2450KL, Brooklyn, NY, USA). Measures were taken in kg to one decimal place. At each visit, the accuracy of the scale was determined using two 6.8 kg weights. Participants then transferred from their wheelchairs to a spine board (National Lifesaving Society item EQ-10, Edmonton, Alberta, Canada) that lay on top of their beds to provide a hard, flat surface on which to measure length. Participants’ feet were placed in dorsal flexion and head in the Frankfurt Plane. As in the general SCI population, leg contractures in our sample were common and prevented some participants from straightening their legs, even with assistance. To maintain measurement consistency for the whole sample, length for all participants was measured to the nearest decimal place, on the right side of the body alongside the spine board, in segments from heel to crown using a flexible, nonelastic tape measure with a spring attachment for constant tension (Gulick II Tape Measure, Gays Mills, WI, USA).
Body mass index (BMI, in kg m−2) was assessed using World Health Organization (WHO) classifications.9 Percent fat mass (%FM) was determined using whole-body bioelectrical impedance analysis (BIA; Bioelectrical Body Composition Analyzer Quantum II, RJL Systems, Clinton Twp., MI, USA) and electrode placement of Lukaski et al.10 Fat-free mass (kg) was calculated using NHANES III equations,11 and FM by subtracting fat-free mass from weight. Lohman and Going's age-specific obesity cutoffs were used to assess %FM.12
Waist circumference (WC) was measured at the level of the iliac crest to the nearest decimal place using the same nonelastic, flexible measuring tape used for length. Participants were supine with arms abducted 30° from midline. The iliac crest was land-marked with a pen and the circumference recorded after normal expiration. Values were interpreted against National Institutes of Health cutoffs.13
Venous blood samples were collected in empty vacutainer tubes with the exception of those for glucose, in which there was anticoagulant. All tubes were immediately placed on ice in a lightfast cooler and were analyzed at the McMaster Medical Centre Department of Laboratory Medicine, Hamilton, on the day of collection. All specimens were centrifuged for 15 min at 3000 r.p.m. Samples for insulin were separated and frozen at −80 °C until analysis, the next business day.
Insulin was measured using a solid-phase, two-site chemiluminescent immunometric assay (IMMULITE 2000/2500; Intermedico, Holliston, MA, USA). Insulin values of six participants were lower than detectable by assay (<15 pmol l−1); these were assigned a value of 14 pmol l−1 during statistical analyses. Glucose was measured using the hexokinase method (Roche Modular ISE 1800; Roche, Laval, Québec, Canada). Insulin resistance was determined using the homeostasis model assessment for insulin resistance (HOMA-IR),14 where HOMA-IR=(glucose mmol l−1 × insulin mU l−1)/22.5.
Total cholesterol (TC) and triglycerides (TG) were determined using an enzymatic colorimetric test and HDL-C using a homogeneous enzymatic colorimetric test (Roche). Low-density lipoprotein cholesterol (LDL-C) values were determined using the Friedewald equation.15 High-sensitivity C-reactive protein (CRP) was measured using particle enhanced immunonephelometry (CardioPhase hsCRP; Dade Behring, Mississauga, Ontario, Canada). CRP cut points of 3.1–9.9, 1.0–3.0 and <1.0 mg l−1 classified participants as high, average and low CHD risk, respectively.16 Those whose CRP values were indicative of acute inflammation (⩾10 mg l−1)16 were excluded from CRP statistical analyses. CRP values between participants with versus without self-reported infections and taking versus not taking statins were not significantly different (data not shown); these participants were therefore included in CRP statistical analyses. Blood pressure (BP) was measured on the right arm, in the sitting position after a 5 min rest, by auscultation using a stethoscope and sphygmomanometer.
All participants were categorized into those with >20%, 10–20% or <10% 10-year risk for CHD according to FRS using traditional risk factors including gender, age, TC, HDL-C and systolic BP.6 Participants were also classified as positive or negative for metabolic syndrome using four internationally recognized definitions (presented in the Appendix) including the World Health Organization (Metabolic SyndromeWHO);17 the original National Cholesterol Education Program (Metabolic SyndromeNCEP);6 the original National Heart, Lung, and Blood Institute/American Heart Association (Metabolic SyndromeNHLBI/AHA)7 and the original International Diabetes Federation (Metabolic SyndromeIDF) definition18 (in our analysis, Europid cut points for WC were used for Caucasians, Native Canadians and those of unknown ethnic origin (⩾94 cm in men and ⩾80 cm in women; n=63), while ethnic South and Central Canadian cut points were used for Hispanic Canadians (⩾90 cm in men, ⩾80 cm in women; n=1)). The only modification we made was to Metabolic SyndromeWHO. In the current study, and with respect to glucose regulation, only fasting glucose (FG) and self-reported diabetes mellitus data were collected. Therefore, these were the only two measures used to identify impaired glucose regulation as neither 2-h post-glucose load nor hyperinsulinemic euglycemic conditions were performed as suggested in Metabolic SyndromeWHO.17 In addition, waist-to-hip ratio and urinary albumin excretion rate were not measured and were therefore excluded from Metabolic SyndromeWHO diagnosis.
Statistical analyses
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS version 14.0, Chicago, IL, USA). Only descriptive data are reported for both the percentage of participants with metabolic syndrome and the distribution of 10-year CHD risk according to FRS. The κ-values are calculated to determine interrater reliability and in this case were applied to test agreement between the four metabolic syndrome definitions where κ=0.40–0.59, κ=0.60–0.79 and κ⩾0.80 refer to moderate, substantial and good agreement, respectively.19 Correlations were computed between duration of injury and individual CVD risk factors using Pearson's and Spearman's correlation coefficients for normally and nonnormally distributed data, respectively.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
A total of 75 participants participated in the substudy. Of these, 10 were excluded based on self-reported CHD and/or diabetes mellitus and/or were receiving pharmacological treatment for these conditions. Of the remaining 65 participants, 4 had not fasted for at least 10 h; 3 were unable to provide blood samples; 1 was missing WC data and 1 was missing data to calculate BMI. Therefore complete data for 56 participants were available for determination of metabolic syndrome using Metabolic SyndromeNCEP, Metabolic SyndromeNHLBI/AHA and Metabolic SyndromeIDF definitions, 57 for Metabolic SyndromeWHO definition and 61 participants for determination of 10-year CHD risk using FRS.
Background characteristics are presented in Table 1. The group was predominantly male (80.0%) and Caucasian (93.8%). Mean age was 41.7±11.7 years (range 21–79 years) and average duration of injury was 15.0±10.6 years (range 1–47 years). Of the 33 (50.8%) participants with tetraplegia, 9 (27.3%) and 24 (72.7%) had complete and incomplete lesions, respectively. Of the 32 (49.2%) participants with paraplegia, 13 (41.9%) and 18 (58.1%) had complete and incomplete lesions, respectively; completeness of lesion unknown for one participant. The majority of participants (92.3%) ambulated with a wheelchair (manual or power), and the remainder with braces (3.1%), walker (1.5%), cane (1.5%) or crutches (1.5%). Participants with CHD and/or diabetes excluded from statistical analysis were older (47.1±11.8 years; range 28–70 years), but had been living with SCI for a similar duration (14.9±10.4 years; range 2–34 years) versus those without.
Anthropometric and biochemical data are presented in Table 2. All variables fell within normal limits, with the exception of CRP, %FM and WC (for female participants). Mean CRP (3.4±3.0 mg l−1) was consistent with high CHD risk. Mean %FM indicated that both male (25.7±7.3%) and female participants (39.4±7.6%) were obese. Mean WC values for female participants (93.4±18.1 cm), but not for male (89.7±13.3 cm), were also indicative of health risk. Duration of injury was not related to any of the CVD risk factors except for FG (r=0.272, P=0.037).
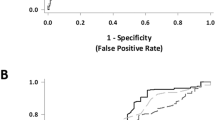
The percentage of metabolic syndrome in the study sample was 3.6, 12.3, 15.8 and 19.3% according to the criteria of Metabolic SyndromeWHO, Metabolic SyndromeNCEP, Metabolic SyndromeNHLBI/AHA and Metabolic SyndromeIDF, respectively (Figure 1). The κ-agreement between definitions varied from no agreement beyond chance between Metabolic SyndromeWHO and Metabolic SyndromeIDF (κ=0.099, P>0.05) to moderate agreement between Metabolic SyndromeWHO and Metabolic SyndromeNHLBI/AHA (κ=0.324, P<0.01) and Metabolic SyndromeWHO and Metabolic SyndromeNCEP (κ=0.412, P<0.001) to substantial agreement between Metabolic SyndromeNCEP and Metabolic SyndromeIDF (κ=0.608, P<0.001) and Metabolic SyndromeNHLBI/AHA and Metabolic SyndromeIDF (κ=0.758, P<0.001) and finally to good agreement between Metabolic SyndromeNCEP and Metabolic SyndromeNHLBI/AHA (κ=0.855, P<0.001). The prevalence of metabolic syndrome in the GP is 19.4%,20 34.5%21 and 39.0%,21 according to Metabolic SyndromeWHO, Metabolic SyndromeNCEP and Metabolic SyndromeIDF, respectively, 2.0–5.4 times higher than the SCI study sample (Figure 1).
Reduced HDL-C levels (31.0%) followed by elevated TG (26.7%) and obesity (24.6%) were the most common metabolic syndrome risk factors in the study sample when averaged across all definitions, followed by hypertension (23.8%) and finally elevated FG (10.2%) (Figure 2).
FRS identified 80.3, 16.4 and 3.1% of participants to be at low (<10%), moderate (10–20%) and high (>20%) 10-year CHD risk, respectively, with a mean risk of 4.8±6.3%.
Discussion
This is the first study in community-dwelling persons with SCI to quantify metabolic syndrome using multiple definitions, and to calculate 10-year CHD risk using the most recent FRS algorithm. The most important finding was that persons with SCI are at seemingly low risk for CHD. However, rather than reflecting a truly decreased risk for CHD, this may be due in part to insensitivity of these tools in this population.
Although persons with SCI have increased morbidity (2) and mortality (1) related to CVD, metabolic syndrome was lower in this sample population compared to the larger GP. Similarly, FRS indicated relatively low CHD risk in our sample population. Rather than reflecting a truly decreased risk of CHD, this may be due to the fact that current metabolic syndrome definitions and FRS, all derived in AB populations, include metabolic risk factors that preclude accurate CHD risk assessment in SCI. Similar concerns regarding the application of common CVD risk assessment tools derived in the AB population to persons with SCI have been expressed by others.4, 5, 22 For example, impaired glucose tolerance, but not elevated FG, is common in the SCI population.2 Metabolic syndrome definitions include FG and thus not surprisingly fail to identify persons for whom glucose-related aberrations occur in the nonfasted state. Similarly, mean %FM of our participants was consistent with the definition of obese;12 however metabolic syndrome definitions include BMI or WC, both of which have questionable sensitivity in the SCI population when using AB cutoffs.23, 24 Finally, mean BP of our study sample was low-to-normal. Although BP is a strong predictor of CHD risk in the AB population, an inverse relationship has been described between the level of spinal cord lesion and reduced BP25 such that BP may not be predictive of CHD risk. Clearly, the use of AB derived metabolic risk factors and/or their associated cutoffs require reevaluation in the SCI population. This is supported by our finding of varying agreement across metabolic syndrome definitions, likely due to the various risk factors and corresponding threshold limits included in each definition. Inclusion of novel CHD risk factors, such as hsCRP, may help identify persons with SCI at risk for CHD. This work is currently underway in our group.
The insensitivity of metabolic syndrome definitions was mirrored in our FRS-related findings. The FRS algorithm includes both smoking status and TC as CVD risk factors; however, Krum et al.26 found that the increased risk of CVD in SCI compared to the AB population cannot be explained by differences in TC or smoking. This would therefore make it difficult for FRS to capture the increased risk of CHD in those with SCI.
Aside from potentially insensitive metabolic markers and/or cutoffs, other factors may have contributed to seemingly lower metabolic syndrome in the current study. First, given the lack of recent Canadian metabolic syndrome prevalence data, prevalence in the GP was based on data from the United States with Canadian obesity rates lower than those of the United States,27 it is most likely that metabolic syndrome would also be elevated in the United States, offering a partial explanation for metabolic syndrome being lower in the current sample population. Second, given that prevalence increases with age, metabolic syndrome was higher in the older GP, potentially contributing to the disparity.
While our study contributes to the literature on chronic diseases in the SCI population, we recognize that it is limited by the cross-sectional nature and small sample size, particularly of women, which precluded a subanalysis by gender. Prospective research that investigates CHD risk factors in men and women against hard end points, such as coronary events, is required in the SCI population to help improve the identification of those at high risk of CHD. We also recognize that some medications may have confounded values for selected biochemical markers, however in excluding participants taking medications for CHD and/or diabetes-related risk factors, we have likely accounted for the most important confounders. Finally, we suggest that future studies investigate the effect of different bladder regimens on CRP values in this population.
In summary, current metabolic syndrome definitions and FRS may underestimate true CHD risk in persons with chronic SCI. We suggest that alternative biological markers be used and/or that cutoffs for current markers—all established in AB populations—be revised for persons with SCI. CRP may be a potential factor to consider in the development of SCI-specific screening tools. CRP is explored more fully in our second article included in this issue of Spinal Cord (Gibson, Buchholz, Martin Ginis, SHAPE SCI Research Group).
References
DeVivo MJ, Krause JS, Lammertse DP . Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1411–1419.
Bauman WA, Spungen AM . Carbohydrate and lipid metabolism in chronic spinal cord injury. J Spinal Cord Med 2001; 24: 266–277.
Kocina P . Body composition of spinal cord injured adults. Sports Med 1997; 23: 48–60.
Lee MY, Myers J, Hayes A, Madan S, Froelicher VF, Perkash I et al. C-reactive protein, metabolic syndrome, and insulin resistance in individuals with spinal cord injury. J Spinal Cord Med 2005; 28: 20–25.
Liang H, Chen D, Wang Y, Rimmer JH, Braunschweig CL . Different risk factor patterns for metabolic syndrome in men with spinal cord injury compared with able-bodied men despite similar prevalence rates. Arch Phys Med Rehabil 2007; 88: 1198–1204.
Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005; 112: 2735–2752.
Martin Ginis KA, Latimer AE, Buchholz AC, Bray SR, Craven BC, Hayes KC et al. Establishing evidence-based physical activity guidelines: methods for the Study of Health and Activity in People with Spinal Cord Injury (SHAPE SCI). Spinal Cord 2007; e-pub ahead of print 34 July 2007.
World Health Organization. Obesity: preventing and managing the global epidemic. Report of WHO Consultation. World Health Organization: Geneva, Switzerland, 2000. WHO technical report series: 894.
Lukaski HC, Johnson PE, Bolonchuk WW, Lykken GI . Assessment of fat-free mass using bioelectrical impedance measurements of the human body. Am J Clin Nutr 1985; 41: 810–817.
Chumlea WC, Guo SS, Kuczmarski RJ, Flegal KM, Johnson CL, Heymsfield SB et al. Body composition estimates from III NHANES bioelectrical impedance data. Int J Obes Relat Metab Disord 2002; 26: 1596–1609.
Lohman T, Going S . Assessment of body composition and energy balance. In: Lamb D, Murray R (eds). Perspectives in Exercise Science and Sports Medicine. Cooper Publishing Group: Carmel, 1998, pp 61–105.
National Institutes of Health. Practical Guide to Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. US Department of Health and Human Services: National Institutes of Health, Bethesda, MD, 2000. Report no. 00-4084.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Friedewald WT, Levy RI, Fredrickson DS . Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972; 6: 499–502.
Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon III RO, Criqui M et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 2003; 107: 499–511.
Alberti KG, Zimmet PZ . Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 1998; 15: 539–553.
International Diabetes Federation. Worldwide definition of the metabolic syndrome (online). 2006 (cited 2006 May 25). Available from: URL: http://www.idf.org.cerberus.lib.uoguelph.ca/webdata/docs/Metabolicsyndromeyndrome_FINAL.pdf. Accessed 02/17, 2006.
Landis JR, Koch GG . The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–174.
Cheung BM, Ong KL, Man YB, Wong LY, Lau CP, Lam KS . Prevalence of the metabolic syndrome in the United States National Health and Nutrition Examination Survey 1999–2002 according to different defining criteria. J Clin Hypertens.(Greenwich) 2006; 8: 562–570.
Ford ES . Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the US. Diabetes Care 2005; 28: 2745–2749.
Jones LM, Legge M, Goulding A . Factor analysis of the metabolic syndrome in spinal cord-injured men. Metabolism 2004; 53: 1372–1377.
Buchholz AC, Bugaresti JM . A review of body mass index and waist circumference as markers of obesity and coronary heart disease risk in persons with chronic spinal cord injury. Spinal Cord 2005; 43: 513–518.
Edwards LE, Bugaresti JM, Buchholz AC . Visceral adipose tissue and the ratio of visceral to subcutaneous adipose tissue are greater in adults with versus without spinal cord injury, despite matching waist circumferences. Am J Clin Nutr 2007, in press.
Chen D, Apple Jr DF, Hudson LM, Bode R . Medical complications during acute rehabilitation following spinal cord injury—current experience of the Model Systems. Arch Phys Med Rehabil 1999; 80: 1397–1401.
Krum H, Howes LG, Brown DJ, Ungar G, Moore P, McNeil JJ et al. Risk factors for cardiovascular disease in chronic spinal cord injury patients. Paraplegia 1992; 30: 381–388.
Tjepkema M . Nutrition: Findings from the Canadian Community Health Survey—adult obesity in Canada: measured height and weight (online). 2005 (2007 Aug 12). Available from: URL: http://www.statcan.ca/english/research/82-620-MIE/2005001/pdf/aobesity.pdf.
Acknowledgements
We gratefully acknowledge the participants of SHAPE SCI and Rebecca Bassett and Iwona Chudzik for their help with data collection. The study was funded by the Canadian Institutes for Health Research.
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Finnie, A., Buchholz, A., Martin Ginis, K. et al. Current coronary heart disease risk assessment tools may underestimate risk in community-dwelling persons with chronic spinal cord injury. Spinal Cord 46, 608–615 (2008). https://doi.org/10.1038/sc.2008.21
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.21
Keywords
This article is cited by
-
Rowing exercise increases cardiorespiratory fitness and brachial artery diameter but not traditional cardiometabolic risk factors in spinal cord-injured humans
European Journal of Applied Physiology (2023)
-
The neurological level of spinal cord injury and cardiovascular risk factors: a systematic review and meta-analysis
Spinal Cord (2021)
-
Cardiovascular disease risk in people with spinal cord injury: is there a possible association between reduced lung function and increased risk of diabetes and hypertension?
Spinal Cord (2017)
-
Coronary artery disease and hypertension in a non-selected spinal cord injury patient population
Spinal Cord (2017)
-
Coronary artery disease presenting with left upper quadrant pain in a patient with chronic cervical tetraplegia
Spinal Cord Series and Cases (2017)