Abstract
Study design:
International expert working group.
Objective:
To develop an International Bowel Function Basic Spinal Cord Injury (SCI) Data Set presenting a standardized format for the collection and reporting of a minimal amount of information on bowel function in daily practice or in research.
Setting:
Working group consisting of members appointed by the American Spinal Injury Association (ASIA) and the International Spinal Cord Society (ISCoS).
Methods:
A draft prepared by the working group was reviewed by Executive Committee of the International SCI Standards and Data Sets, and later by ISCoS Scientific Committee and the ASIA Board. Relevant and interested scientific and professional (international) organizations and societies (approximately 40) were also invited to review the data set and it was posted on the ISCoS and ASIA websites for 3 months to allow comments and suggestions. The ISCoS Scientific Committee, Council and ASIA Board received the data set for final review and approval.
Results:
The International Bowel Function Basic SCI Data Set includes the following 12 items: date of data collection, gastrointestinal or anal sphincter dysfunction unrelated to SCI, surgical procedures on the gastrointestinal tract, awareness of the need to defecate, defecation method and bowel care procedures, average time required for defecation, frequency of defecation, frequency of fecal incontinence, need to wear pad or plug, medication affecting bowel function/constipating agents, oral laxatives and perianal problems.
Conclusion:
An International Bowel Function Basic SCI Data Set has been developed.
Similar content being viewed by others
Introduction
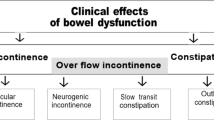
The majority of individuals with spinal cord injury (SCI) has neurogenic bowel dysfunction including constipation, fecal incontinence and abdominal pain or discomfort.1, 2, 3, 4 Colonic transit times are often prolonged,5, 6, 7, 8 and anorectal sensibility and voluntary control of the external anal sphincter is reduced or lost.5, 9, 10 The severity of colorectal and anal sphincter dysfunction depends on the completeness of SCI3 and constipation-related symptoms become significantly more severe with time since injury.1, 11
To facilitate a comparison of symptoms, treatment modalities, and outcomes between patients, various centers and countries it would be advantageous to collect data on bowel symptoms after SCI in the form of common international data sets. The Bowel Function Basic SCI Data Set should mostly be used in connection with the background information within the International SCI Core Data Set.12 For the purposes of research it is recommended that the Bowel Function Basic SCI Data Set be used in connection with the Bowel Function Extended SCI Data Set (Krogh et al., submitted).
Several scores for fecal incontinence and constipation exist but none have yet been generally accepted for use in individuals with SCI. Information necessary for computation of the St Marks score13 and the Wexner score14 for fecal incontinence, the Cleveland Constipation Scoring System15 and the Neurogenic Bowel Dysfunction Score16 is found within the combined Bowel Function Basic and Extended SCI Data Sets.
In accordance with the aim and vision of the International Spinal Cord Injury Data Sets,17 the aim of this study on the International Bowel Function Basic SCI Data Set is to present a standardized format for the collection and reporting of a minimal amount of information on bowel function in daily practice. Furthermore, the Bowel Function Basic SCI Data Set will make it possible to evaluate and compare results from various published studies on bowel dysfunction after SCI.
Methods
The first draft of the International Bowel Function Basic SCI Data Set was made by a working group consisting of members appointed by the American Spinal Injury Association (ASIA) and the International Spinal Cord Society (ISCoS), together with a representative of the Executive Committee of the International Spinal Cord Injury Standards and Data Sets.
The developmental process for the International Bowel Function Basic SCI Data Set followed the steps given below:
-
1)
The working group of the International Bowel Function Basic SCI Data Set finalised the first draft data set during a 3-day meeting in Copenhagen in November 2006. This was further elaborated by frequent e-mail contact among the group members including the development of a syllabus for the data set.
-
2)
The data set was reviewed by the members of the Executive Committee of the International SCI Standards and data sets.
-
3)
Comments from the committee members were discussed in the working group and appropriate changes were made to the data set.
-
4)
Members of the ISCoS Scientific Committee and ASIA Board were also asked to review the data set.
-
5)
Comments from the Committee/Board members were discussed in the working group and a response was made and further adjustments of the data set were carried out.
-
6)
Relevant and interested scientific and professional (international) organizations and societies (approximately 40) and individuals with an interest were also invited to review the data set. In addition, the data set was posted on the ISCoS and ASIA websites for 3 months to allow comments and suggestions.
-
7)
Comments were discussed by the working group and, where appropriate, minor adjustments to the data set were made.
-
8)
To conclude this part of the consultation members of the ISCoS Scientific Committee, Council and ASIA Board received the data set for final review and approval.
-
9)
Endorsement of the data set will be obtained by the relevant (international) organizations and societies.
The Bowel Function Basic SCI Data Set is applicable to adult individuals with traumatic or non-traumatic supraconal, conal or cauda equina lesions. To ensure that data are collected in a uniform manner each variable and each response category within the variables have been specifically defined. Use of a standard format is essential for combining data from multiple investigators and locations. Various formats and coding schemes may be equally effective and could be used in individual studies or by the agreement of the collaborating investigators.
Results
The complete data set form is included in the appendix. The complete data syllabus, data sheet and training cases will be available at the respective websites of ISCoS (www.iscos.org.uk) and ASIA (www.asia-spinalinjury.org).
Date of data collection
As the collection of data on bowel function may be carried out at any time since SCI, the date of data collection is imperative to compute time since injury and to identify the data collected in relation to other data collected on the same individual at various time points (i.e., in the International SCI Core Data Set).12
Gastrointestinal or anal sphincter dysfunction unrelated to SCI
This is gastrointestinal or anal sphincter dysfunction concomitant and thus unrelated to changes in bowel function because of SCI.
Functional gastrointestinal disorders, especially irritable bowel syndrome and chronic idiopathic constipation, are very common in the general population. The prevalence depends on the exact definitions used but vary from 5% up to approximately 20%.18 The presence of functional or other gastrointestinal disorders before SCI may affect symptoms and treatment outcome. Anal sphincter lesions, that is, because of childbirth, are common and may contribute to fecal incontinence. Many types of gastrointestinal and anal sphincter dysfunction exist and it is therefore impractical to give an exact list of such conditions within the data set. Instead, clinicians or researchers are asked to specify gastrointestinal or anal sphincter dysfunction unrelated to SCI.
Surgical procedures on the gastrointestinal tract
For the overall assessment of bowel function in individuals with SCI, the information about surgical procedures on the gastrointestinal tract is important. This variable covers any surgical procedure on the gastrointestinal tract before or after the SCI. It also includes perianal surgery. It is impractical to list the most important or the common procedures because of the large number of possible surgical procedures.
Awareness of the need to defecate
Many individuals with SCI lack any awareness of the need to defecate. Others have indirect symptoms. These are mainly abdominal cramping or discomfort and spasms of the abdominal muscles or lower extremities. Autonomic symptoms including headache, perspiration, piloerection and chills before or during defecation are common, especially in individuals with lesions above Th6.3 Autonomic symptoms are often unpleasant to the individual and may indicate insufficient bowel emptying. Lack of awareness of the need to defecate is especially common in individuals with complete lesions and increases the risk of fecal incontinence. Symptoms may change with time and in this data set they are given for the last 4 weeks.
Defecation method and bowel care procedures
Individuals with SCI may use a combination of bowel emptying procedures. For practical purposes one should be defined as the main method. Supplementary methods should be performed at least once every week. More than one supplementary method can be used. The choice of defecation method and bowel care procedures may change with time and in this data set they are given for the last 4 weeks. Digital ano-rectal stimulation is digital triggering of rectal contractions and anal relaxation, and thus rectal emptying. Digital evacuation is the need to dig out stools with a finger. Mini enema (or Clysma) contains 150 ml or less and enema contain >150 ml.
In individuals having a colostomy, this is always considered the main method for defecation. The list of bowel emptying procedures is given in the appendix.
Average time required for defecation
Time needed for defecation is clinically very important and strongly associated with impact on the quality of life.16 The time given is from first transferring to the toilet or commode until the end of defecation and transferal to wheel chair or raising from the toilet. If bladder emptying, body washing, shaving and so on is also performed while sitting at the toilet, time for these is subtracted. For individuals performing bowel management while lying in the bed, time required is from beginning to end of bowel management not including time for bladder management, body washing and so on. Time needed for defecation is the assessed average time for each defecation within the last 4 weeks.
Frequency of defecation
The frequency of defecation varies widely. However, in the general population more than 94% defecate between three times per day and three times per week.19 Among individuals with SCI approximately 3% defecate less than once every week. Extremely few individuals would not have defecated within the last 4 weeks. However, to be able to compute the Cleveland Constipation Scoring System15 this option is included. Infrequent defecation is an indicator of insufficient bowel management and is associated with impact on the quality of life.16 This variable does not distinguish between spontaneous or assisted defecation.
Frequency of fecal incontinence
Fecal incontinence is defined as involuntary passage of stools. It has profound influence on the quality of life and may cause severe restriction on social activities. The frequency of fecal incontinence is variable even within subjects, so it is assessed over a period of 3 months. This variable does not distinguish between incontinence to solid or liquid stools. Distinction between incontinence to solid stools, liquid stools and flatus is important but will be covered by the Bowel Function Extended SCI data set.
Need to wear pad or plug
This variable describes the need to wear a pad because of fecal incontinence or combined fecal and urinary incontinence. The need to wear a pad only for urinary incontinence is not included. The need to wear a pad indicates insufficient bowel management. The use of anal plug is mainly relevant for individuals with conal or cauda equina lesions.
Medication affecting bowel function/constipating agents
A number of drugs affect gastrointestinal motility. The most commonly used among individuals with SCI are probably anticholinergics and narcotics. Other common examples are calcium antagonists, diuretics, serotonin reuptake inhibitors and spasmolytics. Many drugs affect gastrointestinal function and it is impractical to give an exact list of them all. It does not only include orally taken agents but also patches, suppositories and injections. It does not include laxatives.
Constipating agents, especially loperamide, taken by a minority of individuals with SCI against fecal incontinence should also be listed here.
Oral laxatives
Oral laxatives are commonly used by individuals with SCI.3 A large number of oral laxatives exist either as drops or tablets and it is impractical to give a full list within the frames of this data set. Commonly used bulking or osmotic agents are lactulose, psyllium, magnesium and sorbitol. Commonly used irritant laxatives are bisacodyl and sodium picosulphate. Cisapride, the most commonly used oral prokinetic agent earlier, is now withdrawn from common use and is rarely used in persons with SCI.
Perianal problems
Owing to straining and assisted defecation hemorrhoids, fissures and rectal prolapse are more common among individuals with SCI than in the general population.
Anal soiling may contribute to perianal sores. In this data set perianal sores are located within the crena ani or the perineum and not on the buttocks or lower back. For practical purposes no distinction is made in this data set between rectal mucosal prolapse and full-wall rectal prolapse. Perianal problems may change with the time and only those present within the last year should be noted.
Discussion
The data within this International Bowel Function Basic SCI Data Set will be seen in conjunction with the data in the International SCI Core Data Set,12 which among others includes information on date of birth and injury, gender, the cause of spinal cord lesion, and neurologic status. To make this basic data set as useful as possible in a clinical setting we have kept the number of items as small as possible. However, the working group finds that the 12 items included cover the most clinically relevant information about neurogenic bowel dysfunction in the individuals with SCI. More detailed information will be provided when using the International Bowel Function Extended SCI Data Set. This information will probably be too extensive for widespread clinical use and is mainly intended for clinical studies. The working group recognizes the fact that the information within the bowel data sets could be extended by other clinical important information whenever appropriate.
To facilitate the use of the International SCI Data Sets this Bowel Function Basic Data Set and its data collection (the form is included in the Appendix) have been developed much along the lines of the International Lower Urinary Tract Function Basic SCI Data Set.20
Several scores have been developed for fecal incontinence and constipation but none have yet been generally accepted for use in individuals with SCI. To make results from studies using the SCI Bowel Data Sets, as comparable as possible with results from other patient groups, information covering the most relevant and commonly used scores will be provided by the combined International Bowel Function Basic and Extended SCI Data Sets.
Further study is still needed to validate and translate this data set, and the authors invite all those who are interested to participate in this open and ongoing process.
References
Stone JM, Nino-Murcia M, Wolfe VA, Perkash I . Chronic gastrointestinal problems in spinal cord injury patients: a prospective analysis. Am J Gastroenterol 1990; 84: 1114–1119.
Glickmann S, Kamm MA . Bowel dysfunction in spinal cord injury patients. Lancet 1996; 347: 1651–1653.
Krogh K, Nielsen J, Djurhuus JC, Mosdal C, Sabroe S, Laurberg S . Colorectal function in patients with spinal cord lesions. Dis Colon Rectum 1997; 40: 1233–1239.
Finnerup NB, Faaborg P, Krogh K, Jensen TS . Abdominal pain in long-term spinal cord injury. Spinal Cord 2008; 46: 198–203.
Beuret-Blanquart F, Weber J, Gouverneur JP, Demangeon S, Denis P . Large bowel transit time and anorectal manometric abnormalities in 19 patients with complete transection of the spinal cord. J Auton Nerv Syst 1990; 25: 109–112.
Menardo G, Bausano G, Corazziari E, Fazio A, Marangi A, Genta V et al. Large bowel transit in paraplegic patients. Dis Colon Rectum 1987; 30: 924–928.
Nino-Murcia M, Stone J, Chang P, Perkash I . Colonic transit in spinal cord injured patients. Invest Radiol 1990; 25: 109–112.
Krogh K, Mosdal C, Laurberg S . Gastrointestinal and segmental colonic transit times in patients with acute and chronic spinal cord lesions. Spinal Cord 2000; 38: 615–621.
MacDonagh R, Sun WM, Thomas DG, Smallwood R, Read NW . Anorectal function in patients with complete supraconal spinal cord lesions. Gut 1992; 33: 1532–1538.
Krogh K, Mosdal C, Gregersen H, Laurberg S . Rectal wall properties in patients with acute and chronic spinal cord lesions. Dis Colon Rectum 2002; 45: 641–649.
Faaborg PM, Christensen P, Finnerup N, Laurberg S, Krogh K . The pattern of colorectal dysfunction changes with time since spinal cord injury. Spinal Cord 2008; 46: 234–238.
DeVivo M, Biering-Sørensen F, Charlifue S, Noonan V, Post M, Stipling T et al. International spina cord injury core data set. Spinal Cord 2006; 44: 535–540.
Vaizey CJ, Carapeti E, Cahill JA, Kamm MA . Prospective comparison of faecal incontinence grading systems. Gut 1999; 44: 77–80.
Jorge JMN, Wexner SD . Etiology and management of faecal incontinence. Dis Colon Rectum 1993; 36: 77–97.
Agachan F, Chen T, Pfeiffer J, Reisman P, Wexner SD . A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum 1996; 39: 681–685.
Krogh K, Christensen P, Sabroe S, Laurberg S . Neurogenic bowel dysfunction score. Spinal Cord 2006; 44: 625–631.
Biering-Sørensen F, Charlifue S, DeVivo M, Noonan V, Post M, Stripling T et al. International spinal cord injury data sets. Spinal Cord 2006; 44: 530–534.
Jones R, Lydeard S . Irritable bowel syndrome in the general population. Br Med J 1992; 304: 87–90.
Drossman DA, Sandler RS, McKee DC, Lovitz AJ . Bowel patterns among subjects not seeking health care. Gastroenterology 1982; 83: 529–534.
Biering-Sørensen F, Craggs M, Kennelly M, Schick E, Wyndaele JJ . International; lower urinary tract function basic spinal cord injury data set. Spinal Cord 2008; 46: 325–330.
Acknowledgements
Coloplast A/S, Denmark has supported this study with this data set with an unconditional grant. We are thankful for comments and suggestions received from Susan Charlifue, Lawrence Vogel, Dan Lammertse, William Donovan, Inge Eriks Hoogland, Karen Smith and Peter Christensen.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix

Rights and permissions
About this article
Cite this article
Krogh, K., Perkash, I., Stiens, S. et al. International bowel function basic spinal cord injury data set. Spinal Cord 47, 230–234 (2009). https://doi.org/10.1038/sc.2008.102
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.102
Keywords
This article is cited by
-
Community dwelling life- and health issues among persons living with chronic spinal cord injury in North Macedonia
Spinal Cord (2022)
-
Are micro enemas administered with a squeeze tube and a 5 cm-long nozzle as good or better than micro enemas administered with a 10 cm-long catheter attached to a syringe in people with a recent spinal cord injury? A non-inferiority, crossover randomised controlled trial
Spinal Cord (2022)
-
Examining the complexity of functioning in persons with spinal cord injury attending first rehabilitation in Switzerland using structural equation modelling
Spinal Cord (2020)
-
The data set development for the National Spinal Cord Injury Registry of Iran (NSCIR-IR): progress toward improving the quality of care
Spinal Cord Series and Cases (2020)
-
Cross-sectional and prospective data-collection in North Macedonia—methodological considerations
Spinal Cord Series and Cases (2019)