Abstract
Mutation-induced activation of Wnt-β Catenin signaling pathway is frequent in CRC. The E3 ubiquitin ligase, RNF43, has been reported to negatively regulate the Wnt signaling pathway and RNF43 mutations are frequently seen in CRC. However, its role in Middle Eastern CRC remains unclear. Therefore, we employed Exome and Sanger sequencing technology to assess the frequency of RNF43 mutations and its association with other clinico-pathological features in Middle Eastern CRC. RNF43 mutations were found in 5.9% (13/220) of CRC cases and was inversely correlated to APC and TP53 mutations. A strong association of RNF43 mutations with right sided and sporadic microsatellite instable (MSI) CRC was observed. No association was identified between RNF43 mutation and other clinico-pathological features including BRAF mutation, age, tumor histological subtype, tumor grade or patients’ prognosis. Multivariate logistic regression analysis revealed that MSI status and wild type APC were independent predictor of RNF43 mutation. We conclude that RNF43 mutations occur in Middle Eastern CRC at comparable frequencies with BRAF mutations and represent a distinct molecular subtype which further enhances our understanding of how different mutational subsets of Wnt tumor suppressor genes link to distinct tumor characteristics, which might be considered for treatment strategies for CRC patients.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the second leading cause of cancer-related deaths worldwide1,2. Increased awareness and surveillance have led to decreased incidence of CRC in Western countries, in contrast to the Middle East, where the incidence of CRC is on the rise3,4,5,6. In Saudi Arabia, CRC ranks first among the most frequent malignancies in men7, representing a huge health burden in this part of the world. Consequently, identifying new prognostic markers and therapeutic targets for CRC in this population are highly needed to improve our understanding of cancer occurrence and disease progression.
Mutation induced activation of Wnt signaling pathway is a well-known driver event in CRC8,9. Emerging evidence suggests that specific mutations in Wnt pathway could have different functional and phenotypic ramifications9,10. E3 ubiquitin-protein ligase, RNF43, negatively regulates the Wnt pathway11. Inactivation of RNF43 through RNF43 mutations can lead to permanent activation of Wnt pathway in cancer cells12. Recent studies have shown that RNF43 mutation is a key mutational target in sporadic microsatellite unstable CRC13,14,15.
Interestingly, RNF43 mutations are shown to be associated with distinct tumor locations and subtypes. RNF43 mutations are enriched in microsatellite unstable tumors and right sided CRC16,17. Recent work showed that RNF43 is associated with aggressive tumor biology along with BRAF mutation in right sided CRC18, further supporting a distinct pathogenic mechanism and regional preference for Wnt pathway alterations. Moreover, it has been reported that RNF43 mutation was seen more frequently in sporadic microsatellite unstable (MSI) CRC than in hereditary MSI, which could suggest that sporadic MSI face more selective pressure for RNF43 inactivation14,19.
However, all these studies have been conducted on CRC from different ethnic backgrounds. Data about the role of RNF43 in Middle Eastern CRC is not known. Therefore, we conducted this study to investigate the role of somatic RNF43 mutation in a large cohort of 220 cases using exome sequencing and Sanger sequencing to identify the prevalence, clinico-pathological association and molecular correlation in Middle Eastern CRC.
Materials and methods
Patient selection and tumor samples
Archival samples from 220 CRC patients diagnosed between 2000 and 2015 at King Faisal Specialist Hospital and Research Center (Riyadh, Saudi Arabia) were included in the study. Clinico-pathological data were collected from patient medical records, which are summarized in Table 1.
DNA isolation
DNA samples were extracted from formalin-fixed and paraffin-embedded (FFPE) CRC tumor tissues utilizing Gentra DNA Isolation Kit (Gentra, Minneapolis, MN, USA) according to the manufacturer’s protocols as elaborated in the previous studies20.
Whole-exome and targeted capture sequencing
Whole exome sequencing (WES) was performed on 113 CRC cases using SureSelectXT Target Enrichment by Illumina Novaseq 6000. Quality metrics were performed on raw data using FastQC and aligned to human reference genome (hg19) using Burrows-Wheeler Aligner (BWA)21. The generated bam files were marked for PCR duplicates; local realignment was carried out and to obtain high quality base calls, base-quality recalibration were performed using Picard (http://broadinstitute.github.io/picard/) and GATK22 tools respectively.
Somatic mutation calling was performed by MuTect223 and mutations were annotated with different databases using ANNOVAR24. The single nucleotide variants (SNVs) and indels that passed the standard MuTect2 filters were processed for further analysis, and the somatic variants with minor allele frequency (MAF) of > 0.01 in dbSNP, the NHLBI exome sequencing project, 1000 Genomes and our in-house exome database of ~ 800 normals were removed from the analysis. All the mutations were also checked and viewed using Integrated Genomics Viewer (IGV) to filter out false positives.
Sanger sequencing analysis
Sanger sequencing technology was utilized to sequence entire coding and splicing regions of exons 2, 4, 8 and 9 in RNF43 on 107 CRC cases. The pathogenic mutations detected by Exome sequencing/targeted capture sequencing analysis were further confirmed by Sanger sequencing analysis. Primer 3 online software was utilized to design the primers (available upon request). PCR and Sanger sequencing analysis were carried out as described previously25. Reference sequences were downloaded from the NCBI GenBank and sequencing results were compared with the reference sequences by Mutation Surveyor V4.04 (Soft Genetics, LLC, State College, PA) (Fig. 1).
We assessed the clinical and molecular features from patients harboring RNF43 mutations, using OMS guidelines26 as well as Bethesda and Amsterdam clinical guidelines27 for CRC, to characterize them as serrated polyposis syndrome or other syndromes.
Tissue microarray construction & immunohistochemistry
Tissue microarray (TMA) format was utilized for immunohistochemical analysis of samples. Construction of TMA was done as described previously28. Briefly, representative tumor regions from each donor tissue block were chosen and tissue cylinders with a diameter of 0.6 mm were punched and brought into recipient paraffin block with the help of a modified semiautomatic robotic precision instrument (Beecher Instruments, Wood-land, WI, USA). Two cores of CRC were arrayed from each case.
Tissue microarray slides were processed and stained manually. The immunohistochemistry (IHC) protocol was followed as mentioned before29. For antigen retrieval, Dako (Dako Denmark A/S, Glostrup, Denmark) Target Retrieval Solution pH 9.0 (Catalog number S2367) was used, and the slides were placed in Pascal pressure cooker for 8 min at 120 °C. The primary antibodies were diluted in a 1% solution of bovine serum albumin in phosphate buffered saline (PBS) and incubated overnight at room temperature. Primary antibodies used and their dilutions are listed in Supplementary Table S1. The Dako Envision Plus System kit was used as the secondary detection system with Diaminobenzidine (DAB) as chromogen. All slides were counterstained with hematoxylin, dehydrated, cleared and mounted. Negative controls included replacement of the primary antibody with no reacting antibodies of the same species. Only fresh cut slides were stained simultaneously to minimize the influence of slide aging and maximize reproducibility of the experiment.
Evaluation of mismatch repair protein staining was performed as described previously30. Briefly, MMR protein expression was evaluated using MSH2, MSH6, MLH1 and PMS2 proteins. Details of the primary antibodies used are provided in Supplementary Table S1. Tumor was classified as deficient MMR (dMMR) if any of the four proteins showed loss of staining in cancer with concurrent positive staining in the nuclei of normal epithelial cells. Otherwise, they were classified as proficient MMR (pMMR). β-catenin scoring was performed as described previously31. Briefly, β-catenin expression was considered to be positive when nuclear staining intensity was moderate or strong (Fig. 2).
IHC scoring was done by two pathologists, blinded to the clinico-pathological characteristics. Discordant scores were reviewed together to achieve agreement.
Statistical analysis
Contingency table analysis and Chi square tests were used to study the relationship between clinico-pathological variables and RNF43 mutation. Multivariate analysis was performed using logistic regression model, after adjusting for clinico-pathological variables like age, gender, histology, stage, grade, site of tumor, MMR status, APC mutation and TP53 mutation. The limit of significance for all analyses was defined as p value of < 0.05; two-sided tests were used in these calculations. The JMP14.0 (SAS Institute, Inc., Cary, NC) software package was used for data analyses.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards under the project (RAC # 2190016 dated 08 October 2019) by Research Advisory Council (RAC) of King Faisal Specialist Hospital and Research Center.
Consent to participate
Institutional Review Board of King Faisal Specialist Hospital and Research Centre provided ethical approval for the current study. Research Advisory Council (RAC) granted waiver of informed consent for use of retrospective patient case data and archival tissue samples under project RAC# 2190016.
Consent for publication
All authors have read and approved the submitted manuscript. The manuscript has not been submitted nor published elsewhere.
Results
Patient characteristics
Median age of the study cohort was 46.3 years (range = 13–90 years) with a male:female ratio of 1:1.2. Majority of the cases were adenocarcinoma (86.4%), whereas mucinous CRC accounted for 13.6% of the cases. most of the tumors were moderately differentiated (69.1%) and left sided (75.9%). Lymph node metastasis was noted in 47.7% (105/220) of CRCs and distant metastasis was seen in 17.7% (39/220). 33.2% (73/220) were dMMR by IHC (Table 1).
Mutations in known driver genes
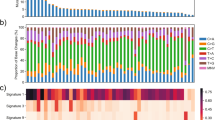
In our entire cohort of 220 cases, the mutations in known driver genes including APC, TP53, KRAS, BRAF and NRAS were observed in 58% (128/220), 51% (112/220), 46% (102/220), 4% (8/220) and 3% (6/220) respectively (Supplementary Fig. 1). The frequency of cases showing more than one APC mutations was 43.7% (56/128) including 45 cases of double mutation, nine cases of triple mutations and two cases of quadruple mutations. Most of the mutations in APC gene were truncating including stopgain (52%), frameshift (40%) and only 8% missense mutations. The mutation classification in TP53 gene include missense (68%), frameshift (10%), stop gain (18%), inframe (2%) and splicing (2%). No significant association was seen between RNF43 and BRAF mutations since only one case was identified to carry mutation in RNF43 and BRAF genes (7.7%).
RNF43 mutations identified in CRC and their clinico-pathological associations
In our study, 15 RNF43 mutations were identified in 13 CRC cases (5.9%), ten cases detected by WES and three cases detected by Sanger sequencing, including frameshift mutation in six cases, stop gain mutation in four cases, missense mutation in four cases and splicing mutation in one case. Two cases harbored two RNF43 mutations respectively (Table 2).
RNF43 mutation was found to be significantly associated with right-sided tumors (p = 0.0170) and dMMR (p = 0.0008). 53.9% (7/13) of the RNF43 mutant cases were right sided tumors and 76.9% (10/13) were dMMR. We also found an association between RNF43 mutation and APC wildtype (p = 0.0079) as well as TP53 wildtype (p = 0.0341) CRC, with 76.9% (10/13) of RNF43 mutant CRCs being APC wildtype and TP53 wildtype (Table 3). However, no association was between RNF43 mutation and nuclear β-catenin expression (Fig. 3). Interestingly, on multivariate logistic regression analysis, we found that dMMR (Odds ratio = 5.43; 95% confidence interval = 1.12–26.32; p = 0.0356) and APC wildtype (Odds ratio = 4.77; 95% confidence interval = 1.51–19.77; p = 0.0312) were independent predictors of RNF43 mutation (Table 4).
Discussion
A screening for mutations in 220 primary CRCs identified RNF43 coding for ring domain E3 ubiquitin-protein ligase is mutated in Middle Eastern CRC. Our analysis revealed that 5.9% of the Middle Eastern CRC patients had RNF43 mutations. This is similar to what has been reported in the largest existing RNF43 study of Seeber et al. (6.1%)32. Similar frequency of RNF43 mutant cases has also been observed in TCGA cohort where RNF43 mutations were seen in about 5.7% (12/212) of CRC patients33. Different studies have reported higher incidence of RNF43 mutations in CRC14,18. This differences could be attributed to the sample size differences, technical artifacts and ethnic backgrounds of CRC patient analyzed.
Consistent with previous reports14,15,34,35, multivariate analysis revealed that dMMR tumors and wild type APC were independently associated with RNF43 in this population. Importantly, RNF43 ranked fourth in mutational frequency to APC (58.2%; 128/220), TP53 (50.9%; 112/220), KRAS (46.4%; 102/220) and at comparable frequency with BRAF (3.6%; 8/220) suggesting an important role of this gene in Middle Eastern CRC.
Similar to previous studies, RNF43 mutations were found strongly enriched with MSI-linked hypermutated CRC tumors14,36,37. Despite the shared dMMR phenotype between RNF43 mutations and Lynch syndrome, we could not identify any RNF43 mutations in the Lynch syndrome dMMR cancers. RNF43 mutations were seen mainly in sporadic MSI cancers. This difference in RNF43 mutations between hereditary and sporadic dMMR CRC (which also have been documented previously)19 could be due to the presence of other mutations in Wnt pathway genes in hereditary MSI CRC tumors.
Furthermore, we observed inverse association between RNF43 mutations and APC as well as TP53 mutations. This suggests the presence of relationship between type of Wnt pathway mutations and the biological context of CRC tumors.
RNF43 mutations were not associated with tumor grade, stage or specific histology. In addition, no significant correlation was found between RNF43 and BRAF mutations, contrary to previous reports18,36. This discrepancy could be attributed to the known low rate of BRAF mutations in CRC from this ethnicity and rare prevalence of serrated adenoma as precursor of Middle Eastern CRC38. Previous reports have linked RNF43 mutations with serrated pathway of CRC development that originates from serrated polyp enriched for activating BRAF mutations and mismatch repair (MMR) gene mutations15,36,39. In addition, RNF43 mutations were shown previously to be a late event that drive the progression of sessile serrated adenoma36,40. Therefore, it was hypothesized that RNF43 mutations exerts lower impact on Wnt pathway activation. To test this hypothesis, (as a way to examine Wnt pathway activation) we examined nuclear β-catenin accumulation via IHC in the entire cohort, and tested the association with RNF43 mutations. We found no correlation between RNF43 mutations and nuclear β-catenin level which is supportive of the notion that RNF43 does not display prominent role in Wnt pathway activation. These results must be interpreted carefully in light of some limitations of this study with regards to sample size and lack of copy number variation data. Further larger studies including entire chromosomal instability data are needed to confirm the association between RNF43 and nuclear β-catenin accumulation. The co-occurrence of RNF43 and BRAF mutations was not seen in our study contrary to previous report which showed significant association between RNF43 mutations and BRAF mutations in CRC due to their involvement in MSI and CIMP pathways in colorectal carcinogenesis18. This result could be attributed to the low BRAF mutations identified in CRC patients from Middle Eastern population as previously reported38.
Interestingly, RNF43 mutations were found to be significantly enriched in right sided CRCs, which has also previously been reported in other studies16,17,32,41, and suggests that RNF43 mutations are associated with distinct primary tumor locations within the colon, further supporting regional differences for Wnt pathway alterations.
Despite the interesting findings of this study, we acknowledge that this analysis has some limitations. First, this retrospective analysis was performed at a single institution. Second, the number of patients with RNF43 mutations are limited. Third, this study was conducted on patients from specific ethnicity. Therefore, future study from larger cohort, multi-institution and different ethnicity is needed.
In conclusion, we have found that dysregulated Wnt signaling and mutations in the tumor suppressor RNF43 are involved in Middle Eastern CRC and is representative of a CRC subset with distinct characteristics.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Siegel, R. L., Miller, K. D., Fuchs, H. E. & Jemal, A. Cancer statistics, 2021. CA Cancer J. Clin. 71, 7–33. https://doi.org/10.3322/caac.21654 (2021).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249. https://doi.org/10.3322/caac.21660 (2021).
Keum, N. & Giovannucci, E. Global burden of colorectal cancer: Emerging trends, risk factors and prevention strategies. Nat. Rev. Gastroenterol. Hepatol. 16, 713–732. https://doi.org/10.1038/s41575-019-0189-8 (2019).
Howlader, N. et al. SEER Cancer Statistics Review, 1975–2017 (National Cancer Institute, 2020).
Almatroudi, A. The incidence rate of colorectal cancer in Saudi Arabia: An observational descriptive epidemiological analysis. Int. J. Gen. Med. 13, 977–990. https://doi.org/10.2147/IJGM.S277272 (2020).
Awad, H., Abu-Shanab, A., Hammad, N., Atallah, A. & Abdulattif, M. Demographic features of patients with colorectal carcinoma based on 14 years of experience at Jordan University Hospital. Ann. Saudi Med. 38, 427–432 (2018).
Alrawaji, et al. Saudi Cancer Registry (Saudi Health Council, 2018).
Schatoff, E. M., Leach, B. I. & Dow, L. E. Wnt signaling and colorectal cancer. Curr. Colorectal Cancer Rep. 13, 101–110. https://doi.org/10.1007/s11888-017-0354-9 (2017).
Zhan, T., Rindtorff, N. & Boutros, M. Wnt signaling in cancer. Oncogene 36, 1461–1473. https://doi.org/10.1038/onc.2016.304 (2017).
Bugter, J. M., Fenderico, N. & Maurice, M. M. Mutations and mechanisms of WNT pathway tumour suppressors in cancer. Nat. Rev. Cancer 21, 5–21. https://doi.org/10.1038/s41568-020-00307-z (2021).
Koo, B.-K. et al. Tumour suppressor RNF43 is a stem-cell E3 ligase that induces endocytosis of Wnt receptors. Nature 488, 665–669 (2012).
Serra, S. & Chetty, R. Rnf43. J. Clin. Pathol. 71, 1–6. https://doi.org/10.1136/jclinpath-2017-204763 (2018).
Jo, Y. S. et al. Frequent frameshift mutations in 2 mononucleotide repeats of RNF43 gene and its regional heterogeneity in gastric and colorectal cancers. Hum. Pathol. 46, 1640–1646. https://doi.org/10.1016/j.humpath.2015.07.004 (2015).
Giannakis, M. et al. RNF43 is frequently mutated in colorectal and endometrial cancers. Nat. Genet. 46, 1264–1266 (2014).
Bond, C. E. et al. RNF43 and ZNRF3 are commonly altered in serrated pathway colorectal tumorigenesis. Oncotarget 7, 70589–70600. https://doi.org/10.18632/oncotarget.12130 (2016).
Lai, C. et al. RNF43 frameshift mutations contribute to tumourigenesis in right-sided colon cancer. Pathol.-Res. Pract. 215, 152453 (2019).
Salem, M. E. et al. Molecular analyses of left- and right-sided tumors in adolescents and young adults with colorectal cancer. Oncologist 25, 404–413. https://doi.org/10.1634/theoncologist.2019-0552 (2020).
Matsumoto, A. et al. RNF43 mutation is associated with aggressive tumor biology along with BRAF V600E mutation in right-sided colorectal cancer. Oncol. Rep. 43, 1853–1862 (2020).
Fennell, L. J. et al. RNF43 is mutated less frequently in Lynch syndrome compared with sporadic microsatellite unstable colorectal cancers. Fam. Cancer 17, 63–69 (2018).
Siraj, A. K. et al. Germline POLE and POLD1 proofreading domain mutations in endometrial carcinoma from Middle Eastern region. Cancer Cell Int. 19, 1–9 (2019).
Li, H. & Durbin, R. Fast and accurate long-read alignment with Burrows-Wheeler transform. Bioinformatics 26, 589–595 (2010).
McKenna, A. et al. The genome analysis toolkit: A MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303. https://doi.org/10.1101/gr.107524.110 (2010).
Cibulskis, K. et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat. Biotechnol. 31, 213–219. https://doi.org/10.1038/nbt.2514 (2013).
Wang, K., Li, M. & Hakonarson, H. ANNOVAR: Functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 38, e164. https://doi.org/10.1093/nar/gkq603 (2010).
Bu, R. et al. Identification of novel BRCA founder mutations in Middle Eastern breast cancer patients using capture and Sanger sequencing analysis. Int. J. Cancer 139, 1091–1097 (2016).
Dekker, E. et al. Update on the world Health organization criteria for diagnosis of serrated polyposis syndrome. Endoscopy 158, 1520–1523 (2020).
Lipton, L. et al. Refining the Amsterdam Criteria and Bethesda Guidelines: Testing algorithms for the prediction of mismatch repair mutation status in the familial cancer clinic. J. Clin. Oncol. 22, 4934–4943 (2004).
Siraj, A. K. et al. PD-L1 expression is associated with deficient mismatch repair and poor prognosis in middle eastern colorectal cancers. J. Pers. Med. 11, 73 (2021).
Siraj, A. K. et al. Overexpression of PARP is an independent prognostic marker for poor survival in Middle Eastern breast cancer and its inhibition can be enhanced with embelin co-treatment. Oncotarget 9, 37319 (2018).
Siraj, A. K. et al. Prevalence of Lynch syndrome in a Middle Eastern population with colorectal cancer. Cancer 121, 1762–1771. https://doi.org/10.1002/cncr.29288 (2015).
Morikawa, T. et al. Association of CTNNB1 (β-catenin) alterations, body mass index, and physical activity with survival in patients with colorectal cancer. JAMA 305, 1685–1694 (2011).
Seeber, A. et al. Comprehensive analysis of R-spondin fusions and RNF43 mutations implicate novel therapeutic options in colorectal cancer. Clin. Cancer Res. 9, 1863–1870 (2022).
Network, C. G. A. Comprehensive molecular characterization of human colon and rectal cancer. Nature 487, 330 (2012).
Fujita, M. et al. Genomic landscape of colitis-associated cancer indicates the impact of chronic inflammation and its stratification by mutations in the Wnt signaling. Oncotarget 9, 969–981. https://doi.org/10.18632/oncotarget.22867 (2018).
Wang, C., Ouyang, C., Sandhu, J. S. & Kahn, M. Wild-Type APC is Associated with Poor Survival in Metastatic (American Society of Clinical Oncology, 2020).
Yan, H. H. N. et al. RNF43 germline and somatic mutation in serrated neoplasia pathway and its association with BRAF mutation. Gut 66, 1645–1656. https://doi.org/10.1136/gutjnl-2016-311849 (2017).
Dienstmann, R. et al. Consensus molecular subtypes and the evolution of precision medicine in colorectal cancer. Nat. Rev. Cancer 17, 79–92 (2017).
Siraj, A. K. et al. A very low incidence of BRAF mutations in Middle Eastern colorectal carcinoma. Mol. Cancer 13, 1–9 (2014).
Sekine, S. et al. Frequent PTPRK–RSPO3 fusions and RNF43 mutations in colorectal traditional serrated adenoma. J. Pathol. 239, 133–138 (2016).
McCarthy, A. J., Serra, S. & Chetty, R. Traditional serrated adenoma: An overview of pathology and emphasis on molecular pathogenesis. BMJ Open Gastroenterol. 6, e000317. https://doi.org/10.1136/bmjgast-2019-000317 (2019).
Yaeger, R. et al. Clinical sequencing defines the genomic landscape of metastatic colorectal cancer. Cancer Cell 33, 125-136e123. https://doi.org/10.1016/j.ccell.2017.12.004 (2018).
Author information
Authors and Affiliations
Contributions
The study was conceived and designed by K.S.A. Material preparation and data collection were performed by K.I., W.A.H., H.A.D., S.A., Z.Q., and P.A. Data analysis was performed by R.B., T.M., S.K.P., and K.I. Resources were provided by F.A.D. Supervision was performed by K.S.A. The first draft of the manuscript was written by K.S.A., and A.K.S. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Siraj, A.K., Bu, R., Masoodi, T. et al. Exome sequencing revealed comparable frequencies of RNF43 and BRAF mutations in Middle Eastern colorectal cancer. Sci Rep 12, 13098 (2022). https://doi.org/10.1038/s41598-022-17449-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17449-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.