Abstract
Worsened lipid profiles were observed in chronic hepatitis C (CHC) patients during direct-acting antivirals (DAAs) treatment, among which combination drugs confounded the effect of individual ingredient on lipid. Tenofovir alafenamide (TAF) also worsened lipid profiles in HIV patients. Structural similarity between sofosbuvir (SOF) and TAF prompted us to investigate rapid increase in total cholesterol (TC) and low-density lipoprotein cholesterol (LDL-C) in CHC patients treated with SOF-based DAAs. A retrospective study was performed to analyze 487 CHC patients receiving DAAs with SVR12. Relative risks on elevating TC and LDL-C were analyzed by logistic regression to determine SOF-based over non-SOF-based regimens. TC or LDL-C levels at baseline, week-4 and SVR12 were compared by Wilcoxon matched-pairs signed rank test. Week 4 or SVR12 to baseline ratios of serum TC or LDL-C between regimens were compared by Mann–Whitney's test. 487 patients were treated with Harvoni (SOF-based, 206 patients), Epclusa (SOF-based, 124 patients), Maviret (non-SOF-based, 122 patients), or Zepatier (non-SOF-based, 35 patients). At week 4 during drug treatment, Harvoni, Epclusa, and Maviret induced statistically significant elevation of TC and LDL-C, but Zepatier did not. SOF-based regimens had 2.72-fold higher relative risk (RR) causing 10% elevation of TC (95% CI 1.84–4.02, p < 0.001) and 2.04-fold higher RR causing 10% elevation of LDL-C (95% CI 1.39–3.01, p < 0.001) than non-SOF-based DAAs. SOF-based DAAs were associated with significantly larger amplitude of increases in TC and LDL-C than non-SOF-based DAAs during the initial 4 weeks of treatment, but the increases were not sustained to SVR12.
Similar content being viewed by others
Introduction
Hepatitis C virus (HCV) is one of the major causes of liver-related morbidity and mortality1, estimating infection of approximately 180 million people worldwide2. The HCV life cycle is initiated by binding of virus particles to hepatocellular receptors, endocytosis, fusion of HCV glycoproteins with endosomal membranes, acidification of endosome, and release of the viral genome into cytosol for replication3. Internal ribosome entry site (IRES)-mediated translation of incoming viral RNA enables viral gene expression and processing, and replication occurs in the “membranous webs”4. Following replication, genomic RNAs in complex with NS5A protein (Nonstructural protein 5A) transit to lipid droplets, where core protein localizes and virion assembly occurs5. After acquiring apolipoproteins B and E (apoB and apoE), components of VLDL (very low-density lipoproteins) and LDL (low-density lipoprotein), HCV infectious particles egress in a manner that parallels the VLDL secretory pathway6,7. HCV-infected patients have a prevalence of hepatic steatosis twofold higher than in HBV (Hepatitis B virus)-infected patients8,9, demonstrating a clear correlation between HCV infection and non-alcoholic fatty liver disease. These patients are also more likely to present decreased serum levels of apoB-bearing lipoproteins because HCV seizes these lipoproteins10,11.
HCV nonstructural proteins 4B, 5A and 5B constitute a complex for RNA replication. The RNA translates into a polyprotein processed by viral NS3/4A and host proteases to generate structural proteins for viral assembly and nonstructural proteins involved in RNA replication12. Currently, direct-acting antivirals (DAAs), which have replaced interferon, are the standard treatment for HCV infection13,14. According to mechanisms of action and therapeutic targets, DAAs are classified into four categories: NS3/4A protease inhibitor, NS5A replication complex inhibitor, and NS5B nucleoside and non-nucleoside polymerase inhibitor15. In the class of NS5B nucleoside polymerase inhibitor, sofosbuvir (SOF) is the only drug and plays an important role in the combination of other DAAs for HCV treatment13,14.
Although DAAs provide well-tolerated, safe, and highly efficacious outcomes16, several studies reported worsened lipid profiles in chronic hepatitis C (CHC) patients during DAAs treatment17,18. SOF-based regimens appeared to have greater effect on low density lipoprotein-cholesterol (LDL-C) elevation. In the study by Meissner et al., the patients treated with SOF/ribavirin had significantly increased levels (LDL-C) from baseline to the end of treatment and to post-treatment week 4817. Younossi et al. also found significantly increased LDL-C from baseline to the end of treatment and to post-treatment week 4 in CHC patients treated with SOF/ledipasvir18.
HCV virion is tightly associated with hepatocyte-derived lipoproteins to form a lipid-laden particle, called lipo-viro-particle. It was thought that HCV hijacks lipoproteins that are released to the blood after clearance of the virus by DAAs. Given that the concept is true, all DAA regimens would have equivalent effects on lipid profiles of the blood. In this report, we performed retrospective analysis from the laboratory data of DAA-treated CHC patients based on structural similarity between TAF (tenofovir alafenamide) and SOF (Fig. 1A) and the observation that patients given TAF for HIV (human immunodeficiency virus) infection had elevated cholesterol level19,20,21. Both TAF and SOF are prodrugs with phosphoramidate and phosphoxybenzene side chains that were enzymatically cleaved in the cell to produce bioactive nucleotide analogues by releasing phenolate ion and propan-2-yl 2-aminopropanoate22,23 Therefore, we hypothesized that SOF might be the major contributor to total cholesterol (TC) and LDL-C elevations during DAAs treatment for patients infected by HCV. The mechanism may be related to the phosphoramidate side chain that is cleaved from sofosbuvir to produce an active nucleotide analogue, GS-461203 (2′-deoxy-2′-α-fluoro-β-C-methyluridine-5′-triphosphate)24 (Fig. 1B). To prove our hypothesis, we included HCV patients treated with SOF- or non-SOF-based DAAs and compared lipid profiles between the two groups during and after treatment. We found that SOF-based regimens contributed more to elevated TC and LDL-C during treatment, however, the elevations returned to baseline at SVR12 (sustained virologic response 12 weeks post-treatment).
Structures of tenofovir alafenamide (TAF), sofosbuvir (SOF), and tenofovir disoproxil fumarate (A). TAF and SOF have similar phosphoramidate side chain (green and orange in the figure) that is cleaved from sofosbuvir to produce an active nucleotide analogue, GS-461203 (2′-deoxy-2′-α-fluoro-β-C-methyluridine-5′-triphosphate) (B).
Methods
Study population
The study retrospectively enrolled HCV-infected patients who received DAAs treatment for 8 or 12 weeks at Taipei Veterans General Hospital from September 2018 to August 2020. All patients were aged above 18, male or female and had chronic HCV infection, defined as detectable anti-HCV antibody and HCV RNA level in the serum for more than 6 months. Patients were excluded from the study if they had decompensated cirrhosis. The study was approved by the Institutional Review Board of Taipei Veterans General Hospital and was conducted in accordance with the principles of Declaration of Helsinki and the International Conference on Harmonization for Good Clinical Practice. All patients read and signed informed consent before drug prescription and study-related procedure.
Study design
All patients tested positive for anti-HCV antibody in the blood underwent a series of blood tests as shown in Table 1 including HCV genotype and HCV viral loads. Those with positive HCV RNA in the blood were treated with DAAs. All patients’ daily medications were subjected to drug-drug interaction screening for DAAs. Lipid-lowering medications were discontinued during DAAs treatment and 12 weeks post-treatment. Baseline demographic data were collected before treatment. Hemogram, serum biochemical profiles (albumin, total bilirubin, direct bilirubin, aspartate aminotransferase [AST], alanine aminotransferase [ALT], creatinine, international normalized ratio [INR], estimated glomerular filtration rate [eGFR]), anti-HCV, hepatitis B virus surface antigen (Abbott Architect HBsAg qualitative assay, Abbott Laboratories), HCV RNA and HCV genotype (Abbott RealTime HCV Genotype II, Abbott Laboratories, Abbott) were obtained from all patients. Hemogram and serum biochemistry were collected at baseline, week 4 and SVR12. Non-cirrhotic patients were treated with DAAs as suggested in package insert, with or without with weight-based ribavirin (RBV, Robatrol, 200 mg capsule, Genovate Biotechnology Co., Ltd. Taiwan; 1200 mg daily if the body weight ≥ 75 kg; 1000 mg daily if the body weight < 75 kg) for 8 or 12 weeks. The DAA regimens included SOF/LED (sofosbuvir 400 mg/ledipasvir 90 mg, Harvoni, 206 patients), SOF/VEL (sofosbuvir 400 mg/velpatasvir 100 mg, Epclusa, 124 patients), GLE/PIB (glecaprevir 100 mg/pibrentasvir 40 mg, Maviret, 122 patients), and ELB/GRA (elbasvir 50 mg/grazoprevir 100 mg, Zepatier, 35 patients). Eight patients took RBV for 12 weeks with SOF/VEL, and 7 patients took RBV for 12 weeks with SOF/LED (Table 1).
Virologic assessment
On-treatment effectiveness was assessed by detecting serum HCV RNA levels at weeks 4 and 12 (there was no week 8 data). The effectiveness at the end of treatment was SVR12, defined as serum HCV RNA level < LLOQ (lower limit of quantification) 12 weeks after completed treatment.
Statistical analyses.
All analyses were performed using STATA (12th ed., developed by StataCorp LLC, College Station, TX, USA). The pre-treatment patient characteristics were shown in median (range) and percentages as appropriate and compared by Mann–Whitney's test and χ2 with Fisher’s exact test. The effectiveness of treatment during and after drug administration was shown in number and percentages. Relative risks on elevating TC and LDL-C were analyzed by logistic regression to determine SOF-based regimens over non-SOF-based regimens. TC or LDL-C levels at baseline, week 4 and SVR12 were compared by Wilcoxon matched-pairs signed rank test. Week 4 or SVR12 to baseline ratios of serum TC or LDL-C between regimens were compared by Mann–Whitney's test. All statistics were two-tailed, and the results were considered statistically significant when a p value was < 0.05.
Consent to participate
The study was approved by the Institutional Review Board of Taipei Veterans General Hospital and was conducted in accordance with the principles of Declaration of Helsinki and the International Conference on Harmonization for Good Clinical Practice. All patients read and signed informed consent before drug prescription and study-related procedure.
Consent to publish
All authors agree that the copyright is transferred to the journal in case of acceptance of the manuscript.
Results
Patient characteristics
Four hundred and eighty-seven CHC patients achieving SVR12 were included in the study (Table 1). The median age was 63 years, and 247 patients were male (50.7%). The two major genotypes (GT) are GT 1b (255 patients, 52.4%) and GT 2 (160 patients, 32.9%). Four hundred and fifty-one patients were treatment-naïve (92.6%), and 35 had HBV co-infection (7.2%). No patient received antiviral therapy for HBV, and neither developed HBV reactivation nor hepatitis flares during DAA therapy. Forty-one patients had HIV co-infection, who took anti-HIV drugs. The median log10 HCV RNA level was 6.18. One hundred and ninety-six patients had a baseline viral load < 800,000 IU/mL (40.3%). One hundred and one patients had a Fib-4 fibrosis stage of F3 (20.7%), and 54 patients, F4 (11.1%) (Table 1). The patient percentages of F0, F1, F2, and F3 were similar between SOF and non-SOF groups. F4 fibrosis is 13.3% in SOF group and 6.4% in non-SOF group.
Effectiveness
Four hundred and ninety-five patients were treated with different DAA regimens. Four hundred and eighty-seven patients achieved SVR12. The SVR12 rates for SOF/VEL, SOF/LED, GLE/PIB, and ELB/GRA were 100% (124/124), 99.5% (206/207), 94.6% (122/129), and 100% (35/35), respectively (Table 2).
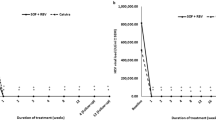
Changes in TC and LDL-C at week 4
Three hundred and thirty patients achieving SVR12 were treated with SOF-based regimens (124 SOF/VEL and 206 SOF/LED), and 157 patients were treated with non-SOF-based (122 GLE/PIB and 35 ELB/GRA) with or without ribavirin (8 patients in SOF/VEL and 7 patients in SOF/LED) for 8 or 12 weeks as shown in Table 1 (DAA regimens). Ribavirin groups were treated for 12 weeks. At week 4, elevated TC (Fig. 2A) and LDL-C (Fig. 2B) were noted in patients treated with SOF/VEL (p < 0.001), SOF/LED (p < 0.001) and GLE/PIB (p < 0.001), but not in patients treated with ELB/GRA (TC, p = 0.176; LDL-C, p = 0.078). The elevations were sustained at SVR12 with SOF/VEL, SOF/LED and GLE/PIB (p < 0.001). However, the ELB/GRA group showed higher TC and LDL-C at SVR12 than baseline (TC, p = 0.023; LDL-C, p = 0.037).
Boxplots showing total cholesterol (TC) (A) and LDL-C (B) levels at baseline, week-4 and SVR12 during different DAAs treatment. Patient number: SOF/VEL (n = 124), SOF/LED (n = 206), GLE/PIB (n = 122) and ELB/GRA (n = 35). TC and LDL-C levels at baseline, week-4 and SVR12 were compared by Wilcoxon matched-pairs signed rank test.
Amplitudes of changes in TC and LDL-C between SOF- and non-SOF-based regimens
Amplitudes of changes in serum TC and LDL-C from baseline to week 4 (or SVR12) were expressed as Log10 [(Week 4 or SVR12)/Baseline] and shown at Y axis of Fig. 3. SOF-based regimens caused significantly larger amplitude of change in TC (Fig. 3A, p < 0.001) and LDL-C (Fig. 3B, p < 0.001) at week 4 compared to non-SOF-based regimens. These changes were not sustained at SVR12 (TC, p = 0.884; LDL-C, p = 0.475). The stratified analyses compared different two regimens and showed that there was no significant difference in log10 (Week4/Baseline) change of both TC (Fig. 3C, p = 0.361) and LDL-C (Fig. 3D, p = 0.248) between the two SOF-based regimens, SOF/VEL and SOF/LED. The statistically significant changes in TC and LDL-C were noted at these two-regimen comparisons: SOF/VEL vs GLE/PIB (TC, p = 0.001; LDL-C, p = 0.010), SOF/LED vs GLE/PIB (TC, p < 0.001; LDL-C, p < 0.001), and SOF/LED vs ELB/GRA (TC, p < 0.001; LDL-C, p = 0.011). The p value of TC at SOF/VEL vs ELB/GRA was 0.017, and that of LDL-C was 0.070. These data suggested that SOF was associated with the major inductor of higher week-4 lipid change.
Boxplots showing TC and LDL-C ratios of week 4/baseline and SVR12/baseline in SOF-based and non-SOF-based DAA (TC in A; LDL-C in B) and in different DAA regimens (TC in C; LDL-C in D). The Y-axis scale is the value of log10[(Week 4 or SVR12)/Baseline]. The differences were compared by Mann–Whitney's test.
Incidence comparisons of increased TC or LDL-C in SOF- and non-SOF-based regimens
To make TC and LDL-C elevations easy to understand, we classified week-4 TC and LDL-C changes to increases > 10% ([Week4/Baseline] > 1.1) and > 25% ([Week4/Baseline] > 1.25) by patient numbers (Table 3). The SOF-based regimens showed higher incidences of increases in TC and LDL-C > 10% (TC, p < 0.001; LDL-C, p < 0.001) or > 25% (TC, p = 0.003; LDL-C, p = 0.001) (Table 3). Relative risk (RR) of TC elevation > 10% for SOF-based regimens was 2.72-fold higher than non-SOF-based regimens (95% CI 1.84–4.02, p < 0.001), and that of LDL-C was 2.04 (95% CI 1.39–3.01, p < 0.001) (Table 4). RR of TC elevation > 25% for SOF-based regimens was 2.11-fold higher than non-SOF-based regimens (95% CI 1.28–3.47, p = 0.003), and that of LDL-C was 2.04 (95% CI 1.36–3.06, p = 0.001) (Table 4).
There were no significant differences in week-4 TC and LDL-C elevations between two SOF regimens (SOF/VEL and SOF/LED) and between two non-SOF regimens (GLE/PIB and ELB/GRA) in either increase > 10% or > 25%. However, in TC > 10%, all SOF vs non-SOF (SOF/VEL vs GLE/PIB, SOF/VEL vs ELB/GRA, SOF/LED vs GLE/PIB, and SOF/LED vs ELB/GRA) showed significant differences in TC elevation. In LDL-C > 10%, SOF/LED caused significant higher risk in LDL-C elevation than GLE/PIB and ELB/GRA. In TC or LDL-C > 25%, SOF-based regimen still showed significant higher risk in some SOF vs non-SOF paired comparisons (SOF/VEL vs GLE/PIB and SOF/LED vs GLE/PIB). In TC or LDL-C > 25%, there are no difference in comparisons SOF/VEL vs ELB/GRA, and SOF/LED vs ELB/GRA. These statistics gave further evidence for SOF in worsened week-4 lipid profiles. The SOF-based lipid-elevation effects were not seen at SVR12 (Supplementary Table 1).
Multivariable logistic regression for possible confounders
The variables in Table 1, which affect SOF- and non-SOF-based statistics (p < 0.05) were subjected to multivariable logistic regression which evaluates confounders of HIV infection, WBC, platelet, DB, AST, creatinine, eGFR, hemodialysis and F4 status, and also classified into week 4/baseline > 1.10 and > 1.25 for TC and LDL-C as shown in supplementary Table 2 (sTable 2). SOF vs non-SOF still gave significant differences in TC and LDL-C at week 4/baseline either > 1.10 or > 1.25. Baseline WBC was negatively associated with TC elevation > 10% at week 4 (adjusted RR = 0.99, p = 0.033). Baseline AST was positively associated with LDL-C elevation > 25% at week 4 (adjusted RR = 1.01, p = 0.021). Hemodialysis was negatively associated with TC and LDL-C elevations either > 10% or > 25% (all with adjusted RR and p < 0.05). The influence of WBC, AST, and hemodialysis on TC and LDL-C during DAAs treatment is uncertain and requires further study to clarify relationship between them.
Chronic diseases-stratified analysis in SOF- and non-SOF groups
To determine whether chronic diseases affected TC and LDL-C during DAA treatment and at SVR12, we stratified SOF and non-SOF groups into disease subgroups including cardiovascular disease, hypercholesterolemia, diabetes mellitus, and chronic kidney disease (sTable 3). Patients with cardiovascular disease and chronic renal disease had higher percentage of patients taking non-SOF-based regimens (sTable 3, p values). The disease-stratified analysis showed that patients with hypercholesterolemia and diabetes mellitus did not have significant elevation of TC and LDL-C (> 10%) at week 4 (sTable 4) and SVR12 (sTable 5). Patients with cardiovascular disease showed elevated TC (p = 0.004) and LDL-C (p = 0.035) at week 4 (sTable 4) and elevated LDL-C (p = 0.027) at SVR12 (sTable 5). Patients with chronic kidney disease showed elevated LDL-C at week 4 (p = 0.040, sTable 4). These data suggest that patients with normal baseline TC and LDL-C contributed more to elevations of TC and LDL-C at week 4 than those with baseline hypercholesterolemia. It is known that diabetes mellitus patients are prone to have elevated blood cholesterol. Then we divided both SOF- and non-SOF groups into normal baseline cholesterol and baseline hypercholesterolemia subgroups. As shown in sTable 6, patients with normal baseline TC and LDL-C showed significant increases in TC (p < 0.001) and LDL-C (p = 0.001) at week 4, but the elevations were not sustained to SVR12 (sTable 7), consistent with data shown in Fig. 3A,B. SOF did not cause significant change in TC and LDL-C at week 4 (sTable 6) and SVR12 (sTable 7) in hypercholesterolemia subgroups.
Discussion
DAAs have been shown to worsen lipid profiles during CHC treatment. To the best of our knowledge, this study is the first retrospective analysis to evaluate the effect of SOF-based DAAs on changes in lipid profiles. Our results showed that compared with non-SOF DAAs, SOF-based DAAs were associated with significant increases in TC and LDL-C during the initial 4 weeks of treatment. However, the SOF-potentiated effects were not sustained at the end of treatment. A further comparison of SOF/VEL or SOF/LED with GLE/PIB and ELB/GRA revealed a similar trend. It is interesting to note that ELB/GRA did not cause TC and LDL-C elevation at week 4. Very limited literature documented association of ELB/GRA with lipid worsening during CHC treatment. Sun et al. reported 24 cases, 13 treated with ELB/GRA and 11 with SOF/LED, showing significant elevation of cholesterol at week 425, which might be the effect of SOF/LED rather than ELB/GRA because our data showed that ELB/GRA did not cause significant increase in total cholesterol at week 4. However, at SVR12, TC and LDL-C increased in ELB/GRA group compared with its baseline (TC, p = 0.023; LDL-C, p = 0.037, Fig. 2).
Combination DAAs have been the treatment standard for CHC. Our data provide strong evidence that SOF-based DAAs resulted in higher elevation of TC and LDL-C than non-SOF-based regimens at week 4 after drug administration (Table 3, Figs. 2 and 3). Since the two kinds of regimens achieved similar SVR12, viral clearance appeared not to be the sole mechanism to account for different TC and LDL-C changes between the two. We compared three compounds, sofosbuvir, tenofovir alafenamide (TAF), and tenofovir disoproxil fumarate (TDF) (Fig. 1) and found that SOF and TAF have similar phosphoramidate side chains (Fig. 1A, colored structures in SOF and TAF) and both cause elevated blood cholesterol in the current (SOF) and previous studies (TAF)19,20,21. However, TDF without the side chains did not affect cholesterol level. Milinkovic et al. reported changes in lipid profile in HIV patients treated with TDF or TAF. After switching from TDF to TAF, mean total cholesterol increased from 186 ± 37 mg/dL at baseline to 206 ± 43 mg/dL and 204 ± 43 mg/dL at weeks 12 and 24 (p < 0.001), and the increase in total cholesterol was mainly due to an increase in LDL-C20. Similar lipid changes were reported by other HIV investigators21,26.
For CHC patients, SOF-based DAAs significantly elevated TC and LDL-C levels during the initial 4 weeks of treatment, but the higher amplitudes of changes in TC and LDL-C tended to disappear at the end of treatment. It could be deduced from the chemical structures of SOF and TAF that the cleaved products phenolate ion and propan-2-yl 2-aminopropanoate from the phosphoramidate side chain may promote β-lipoprotein synthesis and secretion initially and then induce more enzymes to destroy them with time, so TC and LDL-C levels jump transiently and then decline. SOF-based DAA regimens have been shown to have cardiotoxicity27,28, so careful monitoring of initial four weeks of lipid profiles is important, especially for patients with ischemic heart disease or diabetes mellitus.
Our results showed trends of increases in TC and LDL-C at week 4 and SVR12. Some reports showed the increases in TC or LDL-C disappeared after treatment29,30. Other studies suggested the elevated LDL-C continued to post-treatment 1 year31,32,33,34. The main reason for the inconsistency was that most of these studies were single-arm studies with different drugs and doses and without placebo controls. Additionally, both Younossi et al. and Pedersen et al. observed that genotype 3 patients had significantly increased LDL-C during DAAs treatment, but genotype 1 or genotype 2 patients did not35,36. As the majority of the included patients in the present study were genotype 1 (59.6%) and genotype 2 (32.9%) patients (Table 1), changes in LDL-C would be less, consequently reducing the difference between treatment groups. Furthermore, genetic factors have been reported in association with changes in LDL-C. In the study by Emmanuel et al., the IFNL4-ΔG carriers had significant increases in LDL-C during DAAs treatment and at post-treatment 1 year, but the patients with IFNL4-TT/TT did not37. In the study by Morihana et al., the difference in LDL-C between sofobusvir/ledipasvir and daclatasvir/asunaprevir disappeared after the end of treatment. However, the IL28B TG/GG patients continued to have increased LDL-C from the end of treatment to post-treatment 2 years, whereas the IL28B TT patients did not29. Because the current analysis did not consider these genetic factors, our results might be potentially confounded by these predictors.
Although it was common to observe increases in TC and LDL-C during DAAs treatment, a few studies analyzing risk factors for increased LDL-C during DAAs treatment revealed discordant findings. In the study by Morihana et al., multivariate regression analysis showed that changes in LDL-C were negatively correlated with baseline LDL-C and HDL29. Hashimoto et al. reported that the decline of HCV core antigen from day 0 to day 1 was independently associated with amplitudes of changes in LDL-C but not with baseline LDL-C during DAA treatment38. The discordance highlighted the need of prospective large-scale long-term studies to elucidate the effect of DAAs on lipid profiles.
There were several limitations in this study. Firstly, lipid profiles are incomplete without HDL and triglyceride. Secondly, case numbers are uneven among DAA regimens. The third is that the included patients in this study were mainly those who achieved SVR12. In addition, we did not have lipid data of post-treatment long-term follow-up. Therefore, it deserves more comparative studies, which evaluate complete lipid profiles at different time points among DAAs regimens. In conclusion, chemical structure of DAAs may be one of the mechanisms causing hyperlipidemia during anti-HCV treatment in addition to abrupt lipoprotein release from hepatocyte to the blood during HCV clearance. SOF contributes more to dyslipidemia than other DAAs probably on account of its phosphoramidate side chain, which deserves attention in patients taking drugs containing the side chain long term such as TAF to treat HIV and HBV. Dyslipidemia may increase cardio- and cerebro-vascular events in these patients.
Data availability
The datasets generated during and analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Global Burden of Hepatitis, C. W. G. Global burden of disease (GBD) for hepatitis C. J. Clin. Pharmacol. 44, 20–29. https://doi.org/10.1177/0091270003258669 (2004).
Petruzziello, A., Marigliano, S., Loquercio, G., Cozzolino, A. & Cacciapuoti, C. Global epidemiology of hepatitis C virus infection: An up-date of the distribution and circulation of hepatitis C virus genotypes. World J. Gastroenterol. 22, 7824–7840. https://doi.org/10.3748/wjg.v22.i34.7824 (2016).
Burlone, M. E. & Budkowska, A. Hepatitis C virus cell entry: Role of lipoproteins and cellular receptors. J. Gen. Virol. 90, 1055–1070. https://doi.org/10.1099/vir.0.008300-0 (2009).
Moradpour, D., Penin, F. & Rice, C. M. Replication of hepatitis C virus. Nat. Rev. Microbiol. 5, 453–463. https://doi.org/10.1038/nrmicro1645 (2007).
Miyanari, Y. et al. The lipid droplet is an important organelle for hepatitis C virus production. Nat. Cell Biol. 9, 1089–1097. https://doi.org/10.1038/ncb1631 (2007).
Gastaminza, P. et al. Cellular determinants of hepatitis C virus assembly, maturation, degradation, and secretion. J. Virol. 82, 2120–2129. https://doi.org/10.1128/JVI.02053-07 (2008).
Huang, H. et al. Hepatitis C virus production by human hepatocytes dependent on assembly and secretion of very low-density lipoproteins. Proc. Natl. Acad. Sci. USA 104, 5848–5853. https://doi.org/10.1073/pnas.0700760104 (2007).
Sharma, P. et al. Hepatic steatosis in hepatitis C virus genotype 3 infection: Does it correlate with body mass index, fibrosis, and HCV risk factors?. Dig. Dis. Sci. 49, 25–29. https://doi.org/10.1023/b:ddas.0000011597.92851.56 (2004).
Thomopoulos, K. C. et al. Prevalence of liver steatosis in patients with chronic hepatitis B: A study of associated factors and of relationship with fibrosis. Eur. J. Gastroenterol. Hepatol. 18, 233–237. https://doi.org/10.1097/00042737-200603000-00002 (2006).
Hofer, H. et al. Hepatocellular fat accumulation and low serum cholesterol in patients infected with HCV-3a. Am. J. Gastroenterol. 97, 2880–2885. https://doi.org/10.1111/j.1572-0241.2002.07056.x (2002).
Marzouk, D. et al. Metabolic and cardiovascular risk profiles and hepatitis C virus infection in rural Egypt. Gut 56, 1105–1110. https://doi.org/10.1136/gut.2006.091983 (2007).
Tellinghuisen, T. L., Evans, M. J., von Hahn, T., You, S. & Rice, C. M. Studying hepatitis C virus: Making the best of a bad virus. J. Virol. 81, 8853–8867. https://doi.org/10.1128/JVI.00753-07 (2007).
Panel, A.-I. H. G. Hepatitis C guidance 2018 update: AASLD-IDSA recommendations for testing, managing, and treating hepatitis C virus infection. Clin. Infect. Dis. 67, 1477–1492. https://doi.org/10.1093/cid/ciy585 (2018).
Ghany, M. G., Morgan, T. R., Panel, A.-I. H. C. G. Hepatitis C guidance 2019 update: American association for the study of liver diseases-infectious diseases Society of America recommendations for testing, managing, and treating hepatitis C virus infection. Hepatology 71, 686–721. https://doi.org/10.1002/hep.31060 (2020).
Poordad, F. & Dieterich, D. Treating hepatitis C: Current standard of care and emerging direct-acting antiviral agents. J. Viral Hepat. 19, 449–464. https://doi.org/10.1111/j.1365-2893.2012.01617.x (2012).
Falade-Nwulia, O. et al. Oral direct-acting agent therapy for hepatitis C virus infection: A systematic review. Ann. Intern. Med. 166, 637–648. https://doi.org/10.7326/M16-2575 (2017).
Meissner, E. G. et al. Effect of sofosbuvir and ribavirin treatment on peripheral and hepatic lipid metabolism in chronic hepatitis C virus, genotype 1-infected patients. Hepatology 61, 790–801. https://doi.org/10.1002/hep.27424 (2015).
Younossi, Z. M. et al. Ledipasvir/sofosbuvir treatment of hepatitis C virus is associated with reduction in serum apolipoprotein levels. J. Viral Hepat. 22, 977–982. https://doi.org/10.1111/jvh.12448 (2015).
Milinkovic, A., Berger, F., Arenas-Pinto, A. & Mauss, S. Reversible effect on lipids by switching from tenofovir disoproxil fumarate to tenofovir alafenamide and back. AIDS 33, 2387–2391. https://doi.org/10.1097/QAD.0000000000002350 (2019).
Milinkovic, A., Berger, F., Arenas-Pinto, A. & Mauss, S. Lipid changes due to tenofovir alafenamide are reversible by switching back to tenofovir disoproxil fumarate. AIDS https://doi.org/10.1097/QAD.0000000000002350 (2019).
Cid-Silva, P. et al. Treatment with tenofovir alafenamide fumarate worsens the lipid profile of HIV-infected patients versus treatment with tenofovir disoproxil fumarate, each coformulated with elvitegravir, cobicistat, and emtricitabine. Basic Clin. Pharmacol. Toxicol. 124, 479–490. https://doi.org/10.1111/bcpt.13161 (2019).
Ray, A. S., Fordyce, M. W. & Hitchcock, M. J. Tenofovir alafenamide: A novel prodrug of tenofovir for the treatment of Human Immunodeficiency Virus. Antiviral Res. 125, 63–70. https://doi.org/10.1016/j.antiviral.2015.11.009 (2016).
Dousson, C. B. Current and future use of nucleo(s)tide prodrugs in the treatment of hepatitis C virus infection. Antivir. Chem. Chemother. 26, 2040206618756430. https://doi.org/10.1177/2040206618756430 (2018).
Kirby, B. J., Symonds, W. T., Kearney, B. P. & Mathias, A. A. Pharmacokinetic, pharmacodynamic, and drug-interaction profile of the hepatitis C virus NS5B polymerase inhibitor sofosbuvir. Clin. Pharmacokinet. 54, 677–690. https://doi.org/10.1007/s40262-015-0261-7 (2015).
Sun, H. Y. et al. Favouring modulation of circulating lipoproteins and lipid loading capacity by direct antiviral agents grazoprevir/elbasvir or ledipasvir/sofosbuvir treatment against chronic HCV infection. Gut 67, 1342–1350. https://doi.org/10.1136/gutjnl-2017-313832 (2018).
Taramasso, L. et al. Lipid profile changings after switching from rilpivirine/tenofovir disoproxil fumarate/emtricitabine to rilpivirine/tenofovir alafenamide/emtricitabine: Different effects in patients with or without baseline hypercholesterolemia. PLoS ONE 14, e0223181. https://doi.org/10.1371/journal.pone.0223181 (2019).
Mazzitelli, M. et al. Evaluation of cardiac function by global longitudinal strain before and after treatment with sofosbuvir-based regimens in HCV infected patients. BMC Infect. Dis. 18, 518. https://doi.org/10.1186/s12879-018-3426-9 (2018).
Caldeira, D. et al. Cardiac harms of sofosbuvir: Systematic review and meta-analysis. Drug Saf. 41, 77–86. https://doi.org/10.1007/s40264-017-0586-2 (2018).
Morihara, D. et al. IL28B gene polymorphism is correlated with changes in low-density lipoprotein cholesterol levels after clearance of hepatitis C virus using direct-acting antiviral treatment. J. Gastroenterol. Hepatol. 34, 2019–2027. https://doi.org/10.1111/jgh.14741 (2019).
Townsend, K. et al. Interferon-free treatment of hepatitis C virus in HIV/hepatitis C virus-coinfected subjects results in increased serum low-density lipoprotein concentration. AIDS Res. Hum. Retroviruses 32, 456–462. https://doi.org/10.1089/AID.2015.0170 (2016).
Beig, J., Orr, D., Harrison, B. & Gane, E. Hepatitis C virus eradication with new interferon-free treatment improves metabolic profile in hepatitis C virus-related liver transplant recipients. Liver Transpl. 24, 1031–1039. https://doi.org/10.1002/lt.25060 (2018).
Carvalho, J. R., Velosa, J. & Serejo, F. Lipids, glucose and iron metabolic alterations in chronic hepatitis C after viral eradication—Comparison of the new direct-acting antiviral agents with the old regimens. Scand. J. Gastroenterol. 53, 857–863. https://doi.org/10.1080/00365521.2018.1473486 (2018).
Ichikawa, T. et al. Carotid intima-media thickness and small dense low-density lipoprotein cholesterol increase after one year of treatment with direct-acting antivirals in patients with hepatitis C virus infection. Intern. Med. 58, 1209–1215. https://doi.org/10.2169/internalmedicine.1514-18 (2019).
Lacerda, G. S. et al. Exploring lipid and apolipoprotein levels in chronic hepatitis C patients according to their response to antiviral treatment. Clin. Biochem. 60, 17–23. https://doi.org/10.1016/j.clinbiochem.2018.07.007 (2018).
Pedersen, M. R., Patel, A., Backstedt, D., Choi, M. & Seetharam, A. B. Genotype specific peripheral lipid profile changes with hepatitis C therapy. World J. Gastroenterol. 22, 10226–10231. https://doi.org/10.3748/wjg.v22.i46.10226 (2016).
Younossi, Z. M. et al. Dysregulation of distal cholesterol biosynthesis in association with relapse and advanced disease in CHC genotype 2 and 3 treated with sofosbuvir and ribavirin. J. Hepatol. 64, 29–36. https://doi.org/10.1016/j.jhep.2015.08.027 (2016).
Emmanuel, B. et al. Metabolic changes in chronic hepatitis C patients who carry IFNL4-DeltaG and achieve sustained virologic response with direct-acting antiviral therapy. J. Infect. Dis. 221, 102–109. https://doi.org/10.1093/infdis/jiz435 (2020).
Hashimoto, S. et al. Rapid increase in serum low-density lipoprotein cholesterol concentration during hepatitis C interferon-free treatment. PLoS ONE 11, e0163644. https://doi.org/10.1371/journal.pone.0163644 (2016).
Acknowledgements
This study was supported by grants from the Ministry of Science and Technology, Taiwan (MOST 109-2314-B-075-031 to Keng-Hsin Lan; MOST-107-2314-B-075-049 -MY2 to Wei-Ping Lee), and Taipei Veterans General Hospital (V108C-121 to Keng-Hsin Lan; V109C-197 to Wei-Ping Lee), Taipei, Taiwan.
Funding
This study was supported by grants from the Ministry of Science and Technology, Taiwan (MOST 109-2314-B-075-031 to Keng-Hsin Lan; MOST-107-2314-B-075-049-MY2 to Wei-Ping Lee), and Taipei Veterans General Hospital (V108C-121 to Keng-Hsin Lan; V109C-197 to Wei-Ping Lee), Taipei, Taiwan.
Author information
Authors and Affiliations
Contributions
All authors have contributed substantially to preparation of this manuscript including conception and design, execution, analysis, and interpretation of data, and drafting the article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, YK., Wang, YW., Lu, CL. et al. Sofosbuvir-based direct-acting antivirals and changes in cholesterol and low density lipoprotein-cholesterol. Sci Rep 12, 9942 (2022). https://doi.org/10.1038/s41598-022-13657-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-13657-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.