Abstract
The bronchoscopy, though usually safe, is occasionally associated with complications, such as pneumonia. However, the use of prophylactic antibiotics is not recommended by the guidelines of the British Thoracic Society. Thus far there are few reports of the risk factors for post-bronchoscopy pneumonia; the purpose of this study was to evaluate these risk factors. We retrospectively collected data on patients in whom post-bronchoscopy pneumonia developed from the medical records of 2,265 patients who received 2666 diagnostic bronchoscopies at our institution between April 2006 and November 2011. Twice as many patients were enrolled in the control group as in the pneumonia group. The patients were matched for age and sex. In total, 37 patients (1.4%) had post-bronchoscopy pneumonia. Univariate analysis showed that a significantly larger proportion of patients in the pneumonia group had tracheobronchial stenosis (75.7% vs 18.9%, p < 0.01) and a final diagnosis of primary lung cancer (75.7% vs 43.2%, p < 0.01) than in the control group. The pneumonia group tended to have more patients with a history of smoking (83.8% vs 67.1%, p = 0.06) or bronchoalveolar lavage (BAL) (4.3% vs 14.9%, p = 0.14) than the control group. In multivariate analysis, we found that tracheobronchial stenosis remained an independent risk factor for post-bronchoscopy pneumonia (odds ratio: 7.8, 95%CI: 2.5–24.2). In conclusion, tracheobronchial stenosis was identified as an independent risk factor for post-bronchoscopy pneumonia by multivariate analysis in this age- and sex- matched case control study.
Similar content being viewed by others
Introduction
Bronchoscopy is one of the standard methods for diagnosing respiratory diseases including malignant tumors and diffuse lung diseases1. Bronchoscopy is usually a safe procedure but is sometimes associated with complications such as pneumonia2,3,4,5,6. The incidence of post-bronchoscopy pneumonia ranges from 0.02% to 6.3% and differs according to the reports2,3,5,6. Post-bronchoscopy pneumonia is not only a dangerous condition in itself but also delays treatment of the primary disease2. A small number of studies have examined the risk factors for post-bronchoscopy pneumonia. Aging, abnormal findings in the bronchial lumen, lung cancer, central location of the tumor, and current smoking have been reported as risk factors for post-bronchoscopy pneumonia, but the reports are inconsistent2,3,6. In the current study, we evaluated the risk factors for post-bronchoscopy pneumonia development.
Materials and methods
Our study was a retrospective, single-center case–control study and was performed in accordance with the Declaration of Helsinki and the guidelines and regulations of the ethics committee of Tokyo Metropolitan Tama Medical Center, which approved the study, including a waiver of informed consent for retrospective data collection and deidentified analysis. All patients 20 years old or older who underwent a diagnostic flexible bronchoscopy for abnormal pulmonary lesions in our bronchoscopy unit were eligible for enrollment. The sampling methods included bronchial washing, bronchoalveolar lavage (BAL), endobronchial brushing, needle aspiration, and forceps biopsy as well as transbronchial needle aspiration (TBNA) with or without endobronchial ultrasound (EBUS) assistance. During the study period, radial EBUS, biopsy via guide sheath, and cryobiopsy were not performed. Patients who received therapeutic bronchoscopy, such as laser resection, argon plasma coagulation, stenting, airway foreign body removal, bronchial occlusion, and balloon dilation, were excluded. Data from the medical records of patients who underwent a bronchoscopy at Tokyo Metropolitan Tama Medical Center, a tertiary teaching hospital in Tokyo, between April 2006 and November 2011, were retrospectively collected, and patients in whom post-bronchoscopy pneumonia developed were extracted for allocation to the pneumonia group.
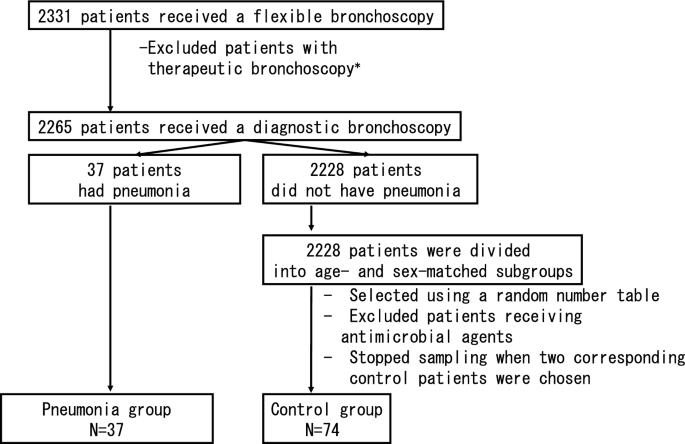
In the present study, post-bronchoscopy pneumonia was defined as pneumonia or a lung abscess diagnosed by the attending physician, the presence of new pulmonary lesions on a chest radiograph or the development or exacerbation of purulent sputum, and was treated with antibiotics within 30 days after the bronchoscopy. Twice as many patients were randomly selected for the control group as for the pneumonia group and were matched for age and sex, with the latter based on a random number table7,8. Patients who received antimicrobial agents were excluded (Fig. 1). Only the initial procedures were included if a patient underwent two or more bronchoscopies.
Flowchart of patient selection. Patients without pneumonia were divided into groups by sex and age (by decade). Patients who received antimicrobial agents on the day before their bronchoscopy were excluded from the control group. *Therapeutic bronchoscopy is defined as laser resection, argon plasma coagulation, stenting, airway foreign body removal, bronchial occlusion or balloon dilation.
The factors evaluated were: history of smoking, immunocompromised state, findings of tracheobronchial stenosis, final diagnosis, and bronchoscopic sampling methods. Patients with a history of smoking one year or longer were defined as smokers. An immunocompromised patient was defined as an individual who received corticosteroids, immunosuppressants or chemotherapy or had diabetes, renal failure, liver failure, an hematologic malignancy or asplenia. Tracheobronchial stenosis was defined as the finding of stenosis in any area between the trachea and the subsegmental bronchi by bronchoscopy that was diagnosed by a certified bronchoscopist. The final diagnosis was defined as a diagnosis based on an analysis of the lesions for which bronchoscopy was indicated.
The bronchoscopies were performed under local anesthesia using lidocaine, intramuscular injections of hydroxyzine pamoate or intravenous injections of pethidine without intubation. The bronchoscopes used were 1T200, 1T240, 1T260, F260 (Olympus, Japan). The procedure was performed by two or more experienced respiratory physicians, including one or more bronchoscopists certified by the Japan Society for Respiratory Endoscopy.
The patients’ age was analyzed using Student's t-test while the physician’s experience was analyzed using Mann–Whitney’s U-test. The other univariate analyses were performed using the chi-square test. Multivariate analysis was performed using logistic regression analysis for factors with p < 0.2 on univariate analysis. P < 0.05 indicated statistical significance. SPSS® (version 19) was used for the statistical analysis.
Results
In 68 months, 2331 patients received 2773 bronchoscopies. Sixty-six patients who received therapeutic bronchoscopies, such as laser resection, argon plasma coagulation, stenting, airway foreign body removal, bronchial occlusion or balloon dilation, were excluded. The median (+ /− SD) age was 65 (+ /− 14) years, and 1393 (61.5%) patients were male. In total, 37 patients (1.4%) had pneumonia. No lung abscess was found. The median duration to pneumonia development after a bronchoscopy was three days (range: 0–20 days). Seventy-four patients who received a bronchoscopy and did not have pneumonia were randomly chosen to be the age- and sex-matched controls (Table 1). Although TBNA with or without EBUS was not excluded, none of the patients in the present study underwent this procedure.
Univariate analysis showed that the pneumonia group had a significantly larger proportion of patients with tracheobronchial stenosis (75.7% vs 18.9%, p < 0.01) and a final diagnosis of primary lung cancer (75.7% vs 43.2%, p < 0.01) than the control group. The pneumonia group tended to have more patients with a smoking history (83.8% vs 67.1%, p = 0.06) than the control group. With respect to the sampling measures, the pneumonia group had slightly more patients who received BAL than the control group (4.3% vs 14.9%, p = 0.14). There was no significant difference in the physicians’ experience between the two groups (p = 0.26) (Table 2). Of the 28 patients who had tracheobronchial stenosis in the pneumonia group, most (24/28, 86%) had lung cancer. Other diagnoses included esophageal cancer (2/28), nontuberculous mycobacterial infection (1/28), and bronchial asthma (1/28). In contrast, of the 14 patients who had tracheobronchial stenosis in the control group, most (8/14, 57%) also had lung cancer. Other diagnoses included diffuse large B cell lymphoma (1/14), metastatic breast cancer (1/14), obstructive pneumonia (1/14), bronchial asthma, and tuberculosis (1/14). Two patients did not receive a diagnosis.
Multivariate analysis performed to identify factors with p < 0.20 found that tracheobronchial stenosis was an independent factor in post-bronchoscopy pneumonia (OR: 15.1, 95%CI: 4.8–48.1) (Table 3).
Discussion
Although previous studies identified variables, such as aging, abnormal findings in the bronchial lumen, lung cancer, central location of the tumor, and current smoking as risk factors2,3,5,6 (Table 4), this age- and sex-matched controlled study demonstrated that tracheobronchial stenosis was the only independent risk factor for post-bronchoscopy pneumonia.
The mechanism of post-bronchoscopy pneumonia in patients with tracheobronchial stenosis can be adequately explained based on that of obstructive pneumonia: first, intramural or extramural stenosis of the normal bronchi occurs due to primary lung cancer, metastatic lung tumor, benign tumor, hematoma, edema, foreign body, pleural effusion or fibrosis. Second, progression to endogenous lipoid pneumonia occurs due to the accumulation of foamy macrophages and mucus and cell invasion caused by disorders of the mucociliary transport system distal to the stenosis. Finally, development of obstructive pneumonia occurs via colonization of bacteria flowing into the lesion9,10. Bronchoscopy can aggravate this condition by carrying the oropharyngeal flora attached to the bronchoscope into the lesion, thereby leading to obstructive pneumonia.
Although several previous studies suggested that lung cancer was associated with post-bronchoscopy pneumonia based on univariate analysis2,3 (Table 4), lung cancer itself was not identified as an independent risk factor on multivariate analysis in our study. Pneumonia developed in four patients in the pneumonia group with bronchial stenosis who did not have lung cancer while pneumonia did not develop in any of the patients in the control group with lung cancer. Indeed, some reports showed that a predisposition for pneumonia was caused by tracheobronchial stenosis due to diseases other than lung cancer. Pneumonia developed in 4.2% of the patients with endobronchial valves for advanced emphysema, and most of the cases were resolved by antibiotic treatment and valve removal11. Obstructive pneumonia also developed due to occlusion by endobronchial Watanabe spigots for refractory pneumothorax and resolved through antibiotic treatment and spigot removal12. A recent study suggested that the central tumor location was one of the risk factors for post-bronchoscopy pneumonia. However, the study did not analyze the bronchoscopic findings and only included patients with lung cancer, which was difficult to diagnose during the bronchoscopy2. Another study suggested that patients with lung cancer with necrosis and/or cavity or large tumor diameter tend to develop a lung abscess13. In the article, the authors suggested that radial EBUS using the guide-sheath (EBUS-GS) technique might contribute to the incidence of lung abscess in patients with lung cancer. However, patients with non-neoplastic lung diseases who do not receive EBUS-GS also acquired pneumonia after bronchoscopy. While the previous study only included patients with lung cancer, the present study included patients with any pulmonary lesions. Notably, there were no patients with a lung abscess in our study. This clear distinction might be due to differences in the patients’ background, sampling methods or the developmental mechanisms of post-bronchoscopy respiratory infection. Thus, our study suggested that it was not lung cancer itself, but the bronchial stenosis caused by any of a number of diseases (including lung cancer), that directly induced post-bronchoscopy pneumonia.
Multivariate analysis did not demonstrate that smoking history was a risk factor for post-bronchoscopy pneumonia despite the promising results of the univariate analysis. Smoking, which is well-known as a risk factor for numerous lung diseases, such as lung cancer, chronic bronchitis, and chronic obstructive pulmonary diseases, can also disturb mucociliary transportation, increase sputum production, and depress the cough reflex14,15. Indeed, a retrospective study of 237 patients with lung cancer who underwent a bronchoscopy reported that current smoking was a risk factor2. However, a previous prospective study of 100 patients who underwent a bronchoscopy suggested that smoking history was not associated with post-bronchoscopy pulmonary complications including pneumonia6, and a study that compared obstructive pneumonia and bacterial, community-acquired pneumonia suggested that smoking was not a risk factor for obstructive pneumonia9. While smoking might directly or indirectly exacerbate post-bronchoscopy pneumonia, its exact role is still unknown.
There are no widely accepted criteria for diagnosing post-bronchoscopy pneumonia, and the definition and observation period for this condition vary2,3,5,6. We defined pneumonia occurring within 30 days after the procedure as a bronchoscopy-related infection in accordance with the surgical-site infection guidelines issued by the Centers for Disease Control and Prevention, which state that an organ infection occurring within 30 days after an operation is likely to be related to the operation if no implant has been left in place16. Our study did not require radiographic confirmation because chest X-rays may fail to detect pneumonia17.
Our study concluded that tracheobronchial stenosis is the only independent risk factor for post-bronchoscopy pneumonia. Tracheobronchial stenosis can be judged promptly during bronchoscopy, and there is no need to wait for the diagnosis. Also, whether tracheobronchial stenosis is caused by lung cancer or not is irrelevant. Our study enrolled the largest number of patients to date for the purpose of determining the risk factors for post-bronchoscopy pneumonia. However, it has some limitations. First, since the study was retrospective and a definitive diagnosis of post-bronchoscopy pneumonia is difficult to establish, the condition might have been underdiagnosed. However, since our criteria for pneumonia included antibiotic administration, few cases of pneumonia were likely to have been overlooked. Second, immune status and bronchoscopic sampling methods varied. A carefully stratified evaluation is needed to address these issues. Third, the role of age and sex was not able to be examined because our study was designed as an age- and sex-matched control study. Finally, since patients who received EBUS-GS, endobronchial cryobiopsy or therapeutic bronchoscopy were not included, the issue of whether tracheobronchial stenosis contributed to post-bronchoscopy pneumonia development in these patients was unable to be addressed.
Conclusion
The present case–control study matching patient age and sex was the first to demonstrate by multivariate analysis that stenosis of the trachea or bronchi is an independent risk factor for the development of post-bronchoscopy pneumonia. This finding will help to identify patients at risk of post-bronchoscopy pneumonia development without the need to wait for a pathological diagnosis.
References
British Thoracic Society BTS Flexible Bronchoscopy Guideline Group. BTS Guideline for diagnostic flexible bronchoscopy in adults. Thorax 68, i10-11 (2013).
Takiguchi, H. et al. Post-bronchoscopy pneumonia in patients suffering from lung cancer: development and validation of a risk prediction score. Respir. Investig. 55, 212–218 (2017).
Kanazawa, H. Efficacy of azithromycin administration in prevention of respiratory tract infection after bronchoscopic biopsy: a randomized, controlled trial. Respirology 12, 70–75 (2007).
Park, J. S. et al. Impact of antibiotic prophylaxis on post-bronchoscopy fever: a randomized controlled study. Int. J. Tuberc. Lung Dis. 15, 528–535 (2011).
Kanemoto, K. et al. Prospective study of fever and pneumonia after flexible fiberoptic bronchoscopy in older people. J. Am. Geriatr. Soc. 54, 827–830 (2006).
Pereira, W. et al. Fever and pneumonia after flexible fiberoptic bronchoscopy. Am. Rev. Respir. Dis. 112, 59–64 (1975).
Lewallen, S. & Coutright, P. Epidemiology in practice: case-control studies. Community Eye Health 11, 57–58 (1998).
D’Souza, G. et al. Case-control study of human papillomavirus and oropharyngeal cancer. N. Engl. J. Med. 356, 1944–1956 (2007).
Abers, M. S. et al. Postobstructive pneumonia: an underdescribed syndrome. Clin. Infect. Dis. 62, 957–961 (2016).
Burke, M. & Fraser, R. Obstructive pneumonitis: a pathologic and pathogenetic reappraisal. Radiology 166, 699–704 (1988).
Sciurba, F. C. et al. A randomized study of endobronchial valves for advanced emphysema. N. Engl. J. Med. 363, 1233–1244 (2010).
Morikawa, S. et al. A simple method of bronchial occlusion with silicone spigots (Endobronchial Watanabe Spigot; EWS®) using a curette. Ther. Adv. Respir. Dis. 10, 518–524 (2016).
Shimoda, M., Yamana, K., Yano, R., et al. Analysis of risk factors for the development of a post-bronchoscopy respiratory infection in lung cancer patients. J. Infecti. Chemotherapy (2020).
Nakagawa, M., Tanaka, H., Tsukuma, H. & Kishi, Y. Relationship between the duration of the preoperative smoke-free period and the incidence of postoperative pulmonary complications after pulmonary surgery. Chest 120, 705–710 (2001).
McGowan, N. Surgery and smoking. Semin. Perioper. Nurs. 8, 146–154 (1999).
Mangram, A. J. et al. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am. J. Infect. Control. 27(97–132), 1999 (1999).
Upchurch, C. P. et al. Community-acquired pneumonia visualized on CT scans but not chest radiographs: pathogens, severity, and clinical outcomes. Chest 153, 601–610 (2018).
Acknowledgements
We thank the Department of Clinical Research at the study institution, which has a qualified statistician on staff, for their excellent support and statistical advice throughout this study. We are also indebted to James R. Valera for his assistance with editing the manuscript.
Author information
Authors and Affiliations
Contributions
Y.S., M.Y., T.I. and K.M. designed the study. Y.S., M.Y. and T.I. have contributed to data collection. K.M. conceived the presented idea and contributed to analysis and interpretation of data. Y.S. and K.M. wrote the main manuscript text and prepared tables. Y.S., M.Y., T.I., K.M., M. K.S., A.W., and M.T. have critically reviewed the manuscript. M.Y, T.I, M. K.S., A.W., and M.T. commented on the manuscript. All the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sato, Y., Murata, K., Yamamoto, M. et al. Risk factors for post-bronchoscopy pneumonia: a case–control study. Sci Rep 10, 19983 (2020). https://doi.org/10.1038/s41598-020-76998-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-76998-z
This article is cited by
-
Pulmonary actinomycosis mimicking lung cancer on 18F-fluorodeoxyglucose positron emission tomography: a case report
Journal of Medical Case Reports (2022)
-
Association between oxygen saturation level during bronchoscopy and post-bronchoscopy adverse events: a retrospective cohort study
Respiratory Research (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.