Abstract
Mortality of primary hypertension is high worldwide. Whether untraditional factors exist in modern life and affect the mortality is not well studied. The aim of the study was to evaluate the risk factors for fatality rate of hypertensive men in downtown area. A cross-sectional study was performed on hypertensive men, who were hospitalized into our hospital and lived in eligible urban areas. The characteristics of the patients and factors for the fatality were analyzed and of the risks or the contributors on the status were investigated. 14354 patients were identified. Mean age was 68.9 ± 12.4 year old (y) and dead ones was 75.9 ± 9.5 y. The overall hospitalized fatality was 5.9%, which was increased with age: fatality with 0.7%, 2.2%, 2.9%, 7.1%, 11.1% and 16.6% was for age group ≦ 49 y, 50–59 y, 60–69 y, 70–79 y, 80–89 y and ≧ 90 y respectively. The increased fatality was significantly positively correlated with the incidence of pneumonia, P < 0.05, r = 0.99. Pneumonia was prone to involve in men with older age and severer organ damage by hypertension. Similar to traditional risks such as coronary heart disease and stroke, pneumonia and lung cancer were also significantly associated with the fatality. Odds ratio (95% CI) for pneumonia and lung cancer were 6.18 (4.35–8.78) and 1.55 (1.14–2.11). The study provides evidence that pneumonia and lung cancer are highly associated with fatality of hypertensive men in downtown area, indicating that in order to reduce the fatality of hypertension, these lung diseases should be prevented and treated intensively in modern life.
Similar content being viewed by others
Introduction
Primary hypertension is one of the most common diseases worldwide; the prevalence reaches 60–80% in elderly1 and 26% in adult population2,3. It is also the most important risk for mortality, responsible for globally 13% of deaths4. Thus the both morbidity and mortality of hypertension are high incredibly in worldwide.
Traditional risk factors, such as coronary heart disease (CHD) and stroke, are implicated in the occurrence of death in patients with hypertension. However, the extent to which those risk factors correlated with mortality in such patients remain insufficiently assessed, highlighting a need for efforts toward finding untraditional risks in order to improve outcomes in this population.
With the social progress, economic development, population increase and human life spans lengthen ad so on, people’s lifestyle changes a lot. Modern life brings people fantastic world. However, the drawbacks exist, such as urban congestion and traffic pollution. One report5 showed that the proportions of men with hypertension in noisy and quiet areas were 23.6% and 17.5% respectively, The data of risk factors associated with mortality of hypertension in downtown community was deficient.
Pneumonia is among the most common illness6 affecting about 450 million people per year and occurring in every part of the world6. It is a main cause of death in all age groups resulting in 7% of the world’s total deaths per year7,8. Lung cancer is also common globally and accounts for the third highest prevalence in mortality9. Both pneumonia and lung cancer increase dramatically10.
Few data exist on whether pneumonia and lung cancer are associated with the mortality of individuals with hypertension. We have reported such issue among female hypertensive patients and found that pneumonia and lung cancer were associated with the fatality of certain age women with hypertension11. The object of this study was to assess the association between incidence of pneumonia/lung cancer and the fatality among male individuals with hypertension.
Material and Methods
Study design and data extraction
This was a cross-sectional study conducted at our hospital, the First Affiliated Hospital of Guangzhou Medical University, in Guangzhou of China. Male patients with primary hypertension were selected from those who were hospitalized into our hospital. The patients’ information forming variety data was derived from the database which officially recorded in information system in our hospital. It included patients’ age, gender, days of hospital stay, diagnoses, complications, comorbidities, therapeutic outcome, cause of death and place of residence, etc.
Ethical approval was obtained from ethics committee of our hospital, Medical Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University. The chairperson of the committee waived the need for patient consent for this study since the study had no effect on the patients and their personal information was not identified in the study. The ethics committee reviewed and proved the study in accordance with International Conference of Harmonization, Good Clinical Practice principles and relevant national laws and regulations.
Selection criteria
The qualified hypertensive patients were consecutively selected from those who were hospitalized due to hypertension or with hypertension. Treaded uncontrolled hypertensives were included. In order to avoid potential sources of bias, patients who had any one of below conditions were excluded: repeatedly hospitalized (only last time was retained), with secondary hypertension, and lived in ineligible geographic areas prior to admission. How the study size was arrived was explained in flow diagram Fig. 1. The eligible geographic areas, in which Yuexiu is our hospital located at, and their population densities12 were shown in Fig. 1.
Data profile (A) and criteria for patients’ residence (B). (A) 14354 in-hospital hypertensive men are at baseline analyses after excluding ones who do not meet the criteria of the study. (B) A map of geographic districts in city Guangzhou and a list of population, area, and population density in the districts. The patients enrolled in current study are from three districts in circles, from where Yuexiu is our hospital located at. The map is generated by Microsoft (R) Paint, version 5.1 (2600, xpsp_sp3_afe.130704–0421: Service Pack 3).
Method of blood pressure (BP) measurement, diagnostic criteria of high BP and stage of high BP
The method of arterial BP measurement was manual cuff compression method with mercury column (Yuyue desktop vertical mercury sphygmomanometer, Jiangsu Yuyue Medical Equipment & Supply Co., Ltd., China). Subjects were empty their bladders and not allowed to smoke, drink tea or coffee for 30 minutes before BP was measured. They sat in a chair with a back, rest for at least 10 minutes to relax body and then BP was measured with sitting position. Both side upper arms were choices for the first time measurement; the side with higher BP value was taken and the side arm was choice thereafter for BP measurement. In general it was right side. Four limbs were measured when pulse pressure was larger than 20 mmHg to exclude secondary high BP. During the mercury drop of measurement, a value with clear first throb was systolic BP and with beat suddenly weak was diastolic BP.
Diagnostic criteria of high BP were: ①Patients had elevated systolic BP (SBP) ≥ 140 mm Hg, or diastolic BP (DBP) ≥ 90 mm Hg, or both BP ≥ 140/90mmg without antihypertensive medication for three times but not in one day. ②They had normal BP or controlled BP below 140/90 mmHg but taking antihypertensive agent/agents. Treaded uncontrolled hypertensives were included and secondary hypertensives were not included in the study. The criteria of stage I, II and III of hypertension were: Stage I - hypertension only; Stage II - hypertension with organ/organs damage but it’s/their function/functions was/were normal. Stage III - hypertension with organ/organs damage/damages as well as it’s/their function/fuctions was/were abnormal.
Organ/organs damage with it’s/their function/functions normal indicated organ/organs harmed by long-term load stress on small arteries resulting in insufficient blood supply due to high BP; it’s/their function/functions was/were normal by compensatory, in which the clinical manifestation/manifestations could be left ventricular hypertrophy, proteinuria or/and cerebral ischemia. Organ/organs damage with it’s/their function abnormal indicated the function/functions of organ/organs was/were decompensated at late stage, III stage, of high BP, such as cardiac failure, renal failure or/and cerebral stroke.
Outcome observation
Primary outcome observed in the study was dead or alive. Secondary outcome observed was the risk factors, complications/comorbidities or diseases/disorders, which influenced the fatality. The associations of the factor/disease/disorder and the fatality of men with hypertension were analyzed. Diseases/disorders were categorized by ICD-10 codes (The International Statistical Classification of Diseases and Related Health Problems 10th Revision).
Classification and definitions of diseases or disorders
In order to study associations of the risk factors and the fatality, the possible factors, complications/comorbidities or diseases/disorders, were classified as positive or negative. Their definitions were: CHD included all types of coronary heart disease. Diabetes did not include impaired glucose tolerance, because they were not the same. Cerebral infarctions were all conformed by brain computerized tomography (CT) or magnetic resonance (MR) examination.
Pneumonia indicated all types of pneumonia, including different location (lobar, bronchial and interstitial), and different cause (viruses, bacteria and/or fungi) etc. Tumor was malignant tumor including lung cancer etc; Lung cancers were all confirmed with histology; they included all types of cancers from the lung, also referred to metastatic lung cancer. Pneumonia or lung cancer might happen prior to or duration of hospital stay.
Hospital death indicated patients who were dead derived from either hypertension or other causes of death with hypertension. The fatality was all-purpose death with hypertension,
Statistical analyses
Excel software was used to manage the data. SPSS software (Version 17; SPSS, Inc) was used to perform statistical analyses. Mean ± standard deviation was used to express continuous variables. Percentage or number was used to express categorical variables. Patients’ basic characteristics were described by Descriptive Statistics. Two continuous variables were compared by Mann-Whitney Test. Incidence of disease = (n/total population)X100%. Correlation analyses were performed with CORREL function to calculate Pearson’s correlation coefficient of r and with TTEST function to obtain statistical P value by Excel.
The associations of categorical variables and fatality were studied by Pearson Chi-square Test when count less than 5 with <20% cells expected; while they were studied by Continuity Correction when count less than 5 with ≧ 20% cells expected. Univariate Analyses were preformed first, from which only the significant variables (P < 0.05) were chosen and placed into Multivariate Analysis Model. Then Multivariate Logistic Backward Regression Model was applied to assess the associations between fatality and the factors, resulting in odds ratio (OR) and its 95% confidence interval (CI) calculated as the degree of fatality risk. P value of < 0.05 was considered statistically significant.
Results
Characteristics of selected patients
A total of 27306 in-hospital men with primary hypertension were selected, Of which, 11220 (40.0%) was excluded with repeated admission; then 133 (0.8%) was excluded with secondary hypertension. The left patients were 15953. Of which, 1599 (10.0%) were excluded again with living at ineligible geographic area prior to admission. Finally, the sample size of 14354 was reached, Fig. 1. Mean age of the patients was 68.9 ± 12.4 year old (ys). The age distribution was gathered in 55–89 ys, in which, the percentage of each group, based on every 5 years, was >10%, Fig. 2.
Age distribution of men with hypertension and dead ones (A) and relationship between the age and complications/comorbidities (B,C). (A) The figure supports hypertension is an aged related disease. (B) Numbers of Comp (complications/comorbidities) increase with age. P < 0.000, r = 0.99. (C) Patients with Comp are significantly older than those without except for hemorrhagic stroke marked NS (not significant). *P < 0.05. CHD = coronary heat disease; -S = stroke.
Characteristics of dead ones in selected patients
Among the patients in the study population above, overall fatality was 5.9%. Mean age of the death was 75.9 ± 9.5 ys. The age distribution was gathered at 70–89 ys, in which, the percentage of every group was >10%, Fig. 2A. The hospital stay and percentage of isolate hypertension (Patients who met the criteria for primary hypertension without any complication and comorbiditiy) from dead patients were shown in Table 1.
Leading complications and comorbidities
Patients accompanied with one or more complications/complications were as many as 87.6%, so patients with isolated hypertension were 12.4%. While, dead ones with isolated hypertension were only 0.6%, Table 1.
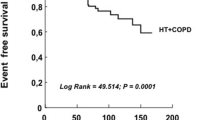
Frequencies and types of complications/comorbidities were shown in Fig. 2 and Table 2. Except for traditional complications/comorbidities such as CHD and ischemic stroke, to our surprise, pneumonia and lung cancer were also among the leading complications/comorbidities list. For pneumonia, positive correlation was found between incidence of it and the fatality (Fig. 3).
Positive correlation between incidence of pneumonia and the fatality of hypertension. (A), The fatality of men with hypertension increases with age. (B) Significant positive coefficient correlation (SP-CC) is found between incidence of pneumonia and the fatality. (C) SP-CC is also found in pneumonia between the patients and dead ones. (D) SP-CC is not found in lung cancer between the patients and dead ones.
Factors influencing incidence of pneumonia and lung cancer
In order to recognize what factors might affect incidence of pneumonia and lung cancer, we analyzed severity of the hypertension and age, and found positive correlation between incidence of pneumonia and stage of hypertension (Fig. 4), also between incidence of pneumonia and age (Fig. 4).
Pneumonia is susceptible in patients with higher stage of hypertension and older age. (A) Distribution of each stage of hypertension in the patients. (B) Distribution of pneumonia in each stage of hypertension. (C) The higher stage of hypertension the more pneumonia. (D) The higher stage of hypertension the more pneumonia and the older age.
However, above correlations were not found for lung cancer. Percentage of stage I, II and III hypertension with lung cancer was 3.0%, 3.2% and 3.1%, P > 0.05. The mean age of men with lung cancer was 72.6 ± 8.9 (35–92) ys.
Associations between traditional risks and the fatality
Thirty possible confounders which might affect the fatality were tested, Table 3. Firstly by univariate analysis, the positive factors, with P < 0.05, were applied into multivariate analyses. Secondly, by multivariate analyses, older age, hemorrhagic disorders, acute diseases, chronic diseases and tumor, as broad categories, were found significantly associated with the fatality. In addition, CHD, diabetes, cerebral infarction and acute cerebral hemorrhage were also associated with the fatality. all P < 0.05. It’s reasonable that they were widely accepted as traditional risks for fatality of hypertension.
Associations between untraditional risks, pneumonia/lung cancer, and the fatality
Except for above risks, pneumonia and lung cancer were also found significantly associated with the fatality, both P < 0.05. Furthermore, pneumonia presented odds ratio number the highest, OR = 6.18, 95% CI = 4.35–8.78, indicating it was the most serious factor associated with the fatality. Lung cancer presented OR also >1, = 1.55, indicating the factor was a risk factor, 95% CI = 1.14–2.11, Table 3 and Fig. 5.
It is important to know how many patients were hospitalized with pneumonia/lung cancer and died with it and how these related to the study population. The answers were: 8.0%/3.9% patients were hospitalized with pneumonia/lung cancer, 24.8%/9.6%% patients were died with it (pneumonia/lung cancer). Of the current study population, 16.7%/6.1% patients were hospitalized with pneumonia/lung cancer; 50.4%/17.4% patients were died with it (pneumonia/lung cancer). The former was less than the latter: hospitalized total patients with pneumonia/lung vs. hospitalized hypertensive patients with pneumonia/lung = 8.0% vs. 16.7% /3.9% vs. 6.1%, P = 0.06/0.48; for dead ones = 24.8% vs. 50.4%/ 9.6% vs. %17.4%, P = 0.0002/0.11. Of the four P values, hospitalized hypertensive dead patients with pneumonia were significantly more than hospitalized total patients with pneumonia, P < 0.05 = 0.0002; supporting pneumonia is significantly affect the fatality of hypertension.
Discussion
The mortality of hypertension is very high4 and associated with some factors. The most studied and recognized factors are cardio-cerebral-vascular and metabolism related risk factors, such as CHD and stroke, arterial ischemic stroke, diabetes13, serum uric acid14 and coronary artery calcium15,16. Untraditional risk factors are assessed insufficiently although some of them are also reported including chronic obstructive pulmonary disease (COPD)17, physical activity18, geographic concentrations of medical doctors18, sex and ethnicity19. Whether pneumonia and lung cancer affect the mortality of hypertensive patients is uncertain. We have reported20 they were significantly affect the mortality of certain age women with hypertension.
In the study, we found the most severe risk factor associated with the fatality of men with hypertension was pneumonia. In literature we could not found this information directly, but below evidences indirectly supported our conclusion: Pneumonia is very common ① in all parts of the world7,8; ② in causes of death accounting for 7% of the total death globally yearly, and 10–25% of the hospital deaths who were particularly most in older people and in patients with comorbidities21,22; ③ in hospitalized patients with cardiovascular diseases and with a increased trend to poor outcomes23,24.
Thus, pneumonia is a disease very common and results in high fatality. Coincidentally, hypertension shares these characteristics as well. Therefore, patients should have worse outcomes when they suffer from both hypertension and pneumonia. We also found positive correlations between incidence of pneumonia and age, and between incidence of pneumonia and stage of hypertension. These could explain why and what types of patients (with older age and severe condition of organ damage by hypertension) were prone to involve in pneumonia.
Except for pneumonia, we found another significant risk affect the fatality - lung cancer. Similar to hypertension, lung cancer is also a disease of the elderly; most of the patients with lung cancer (>65%) are old (>65 years old)25. Our results were consistent with this that 75.4% of patients with lung cancer were ≧65. In addition, lung cancer is the most common among cancers for men in Asia26 and the world (1.1 million, 16.5% of all)27. Such high incidence of lung cancer makes it important to reduce its harmfulness.
Hypertension is reported related to increased risk modestly for cancer incidence and mortality28. Medication for lung cancer could make blood pressure higher or cause the outcomes worse, such as Bevacizumab29 and Regorafenib. They may result hypertension, blisters on hand or/and foot skin, and diarrhea. These side effects might be manageable by reducing dosage or stopping the medicines30. Therefore, doctors should beware of the side effects of the medication, prevent and treat them in time.
Causal relationships of hypertension to pneumonia, and between pneumonia and lung cancer may exist. These include: (1) hypertension increases cardiovascular risks such as stroke, which is related with pneumonia: approximately one third of patients with hypertension occurs pneumonia after acute stroke31. (2) hypertension induces vascular endothelial dysfunction with oxidative stress and reactive oxygen species, which are key signaling molecules playing an significant role in the development of inflammation including pneumonia32. (3) hypertension causes kidney failure and heart failure etc. leading to low immunity and respiratory tract infection. Besides, patients with lung cancer increase chances of developing pneumonia; while, patients with history of lung diseases present increased risk of having lung cancer33. All in all, inner-link among hypertension, pneumonia and lung cancer may exist. This may explain why pneumonia and lung cancer are risks significantly affect the fatality of hypertension.
In addition, the reason for high incidence of pneumonia and lung cancer with hypertension in the study should be related with the adverse environment condition of the patients, who were all from the top three most crowd districts in city Guangzhou. These districts have high population density; this city is arranged at the third place for large city in China, and is an important trading port and national transportation center, causing heavy air pollution. Hence, air pollution and carcinogenic material increased etc, should contribute to the more incidence of pneumonia and lung cancer. For history of smoking habits as risk factors, we should consider but didn’t include due to a large number of patients analyzed in the study. The database we used didn’t include this parameter and it’s difficult to collect this data in a short period of time from tens of thousands of people. We may study this in the future.
How to reduce the mortality and fatality of hypertension? Some organizations for the deal with hypertension emphasized to lower blood pressure, but overlook the complications/comorbidities of hypertension. Our observation indicated that for hypertensive management, taking care of complications and comorbidities is extremely important to decrease mortality/fatality, not only traditional risks such as coronary heart disease and stroke, but also lung diseases like pneumonia and lung cancer.
Conclusions
In conclusion, we studied hospitalized fatality of hypertension and effecting factors among a large number of patients in urban China. Our findings provided evidence on fatality and factors associated with fatality; especially the untraditional factors. This study suggests that in order to reduce the mortality/fatality, men with hypertension need intensively management for prevention, diagnosis and treatment of pneumonia and lung cancer.
References
Del, G. A., Pompa, G. & Aucella, F. Hypertension in the elderly. J. Nephrol. 23(Suppl 15), S61–S71 (2010).
Kearney, P. M. et al. Global burden of hypertension: analysis of worldwide data. Lancet 365, 217–223 (2005).
Hajjar, I., Kotchen, J. M. & Kotchen, T. A. Hypertension: trends in prevalence, incidence, and control. Annu. Rev. Public Health 27, 465–490 (2006).
Moon, J. Y. et al. A trend analysis of the prevalence, awareness, treatment, and control of hypertension by age group. J. Prev. Med. Public Health 46, 353–359 (2013).
Belojevic, G. A., Jakovljevic, B. D., Stojanov, V. J., Slepcevic, V. Z. & Paunovic, K. Z. Nighttime road-traffic noise and arterial hypertension in an urban population. Hypertens. Res. 31, 775–781 (2008).
Biscevic-Tokic, J., Tokic, N. & Musanovic, A. Pneumonia as the most common lower respiratory tract infection. Med. Arch. 67, 442–445 (2013).
Ruuskanen, O., Lahti, E., Jennings, L. C. & Murdoch, D. R. Viral pneumonia. Lancet 377, 1264–1275 (2011).
Kabra, S. K., Lodha, R. & Pandey, R. M. Antibiotics for community-acquired pneumonia in children. Cochrane. Database. Syst. Rev. CD004874 (2010).
McGuire, S. World Cancer Report 2014. Geneva, Switzerland: World Health Organization, International Agency for Research on Cancer, WHO Press, 2015. Adv. Nutr. 7, 418–419 (2016).
Simoni, M. et al. Adverse effects of outdoor pollution in the elderly. J. Thorac. Dis. 7, 34–45 (2015).
Shen, Y. et al. Impact of pneumonia and lung cancer on mortality of women with hypertension. Sci Rep. 6, 20 (2016).
National Bureau of Statistics of China. Communiqué of the National Bureau of Statistics Of the People’s Republic of China on Major Figures of the 2010 Population Census, No. 1. Beijing Review. 54, 1 (2011).
Reis, A. F. et al. Hypertension and diabetes-related morbidity and mortality trends in a municipality in the countryside of Sao Paulo. Rev. Lat. Am. Enfermagem. 23, 1157–1164 (2015).
Bombelli, M. et al. Prognostic value of serum uric acid: new-onset in and out-of-office hypertension and long-term mortality. J. Hypertens. 32, 1237–1244 (2014).
Graham, G. et al. Impact of coronary artery calcification on all-cause mortality in individuals with and without hypertension. Atherosclerosis 225, 432–437 (2012).
Mahmoodi, B. K. et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without hypertension: a meta-analysis. Lancet 380, 1649–1661 (2012).
Xu, W., Shubina, M., Goldberg, S. I. & Turchin, A. Body mass index and all-cause mortality in patients with hypertension. Obesity. (Silver. Spring) 23, 1712–1720 (2015).
Hart, J. Association of hypertension mortality rates with geographic concentrations of chiropractors and medical doctors in the u.s., 2008. Dose. Response 11, 543–549 (2013).
Quan, H. et al. Incidence, cardiovascular complications and mortality of hypertension by sex and ethnicity. Heart 99, 715–721 (2013).
O’Donnell, M. J. et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 376, 112–123 (2010).
Viasus, D. et al. Community-acquired Legionella pneumophila pneumonia: a single-center experience with 214 hospitalized sporadic cases over 15 years. Medicine (Baltimore) 92, 51–60 (2013).
Ochoa-Gondar, O. et al. The burden of community-acquired pneumonia in the elderly: the Spanish EVAN-65 study. BMC. Public Health 8, 222 (2008).
Poling, J., Kelly, L., Chan, C., Fisman, D. & Ulanova, M. Hospital admission for community-acquired pneumonia in a First Nations population. Can. J. Rural. Med. 19, 135–141 (2014).
Cangemi, R. et al. Relation of Cardiac Complications in the Early Phase of Community-Acquired Pneumonia to Long-Term Mortality and Cardiovascular Events. Am. J. Cardiol. 116, 647–651 (2015).
la Cruz, C. S., Tanoue, L. T. & Matthay, R. A. Lung cancer: epidemiology, etiology, and prevention. Clin. Chest Med. 32, 605–644 (2011).
Pakzad, R., Mohammadian-Hafshejani, A., Ghoncheh, M., Pakzad, I. & Salehiniya, H. The incidence and mortality of lung cancer and their relationship to development in Asia. Transl. Lung Cancer Res. 4, 763–774 (2015).
Rafiemanesh, H. et al. Epidemiology, incidence and mortality of lung cancer and their relationship with the development index in the world. J. Thorac. Dis. 8, 1094–1102 (2016).
Harding, J. L. et al. Hypertension, antihypertensive treatment and cancer incidence and mortality: a pooled collaborative analysis of 12 Australian and New Zealand cohorts. J. Hypertens. 34, 149–155 (2016).
Chen, J., Lu, Y. & Zheng, Y. Incidence and risk of hypertension with bevacizumab in non-small-cell lung cancer patients: a meta-analysis of randomized controlled trials. Drug Des Devel. Ther. 9, 4751–4760 (2015).
Alexander, W. 2012 american society of clinical oncology and american society of hypertension: 27th annual scientific meeting and exposition. P. T. 37, 471–477 (2012).
Hilker, R. et al. Nosocomial pneumonia after acute stroke: implications for neurological intensive care medicine. Stroke 34, 975–981 (2003).
Cowley, A. W. Jr. et al. Reactive oxygen species as important determinants of medullary flow, sodium excretion, and hypertension. Am. J. Physiol Renal Physiol 308, F179–F197 (2015).
Navarro-Torne, A. et al. Chronic respiratory diseases and lung cancer research: a perspective from the European Union. Eur. Respir. J. 46, 1270–1280 (2015).
Acknowledgements
This work was supported by Guangdong Natural Science Foundation in China (2015A030313467, S2013010015962), Guangdong Science and Technology Plan Project in China (2014A020212364, 2013B021800282) and Guangzhou Science and Technology Plan Project in China (201510010181).
Author information
Authors and Affiliations
Contributions
S.Y.C. and L.J. designed the study. C.Y.L., H.Z. collected and organized the data. S.Y.C., C.Y.L. and L.X.C. analyzed the data. H.J.Y. and T.Z.J. guided statistical study. S.Y.C. and C.Y.L wrote the manuscript. All authors reviewed and agreed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shen, Y., Chen, Y., Huang, Z. et al. Associations between untraditional risk factors, pneumonia/lung cancer, and hospital fatality among hypertensive men in Guangzhou downtown. Sci Rep 10, 1425 (2020). https://doi.org/10.1038/s41598-020-58207-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-58207-z
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.