Abstract
A lack of exercise leads to being overweight or obese affecting regional brain structure and functional connectivity associated with impaired cognitive function and dementia. In recent decades, several studies of healthy individuals suggest that adiposity may also produce negative independent effects on the brain. We aimed to investigate the relationship between body composition – total fat mass (TFM) and visceral adipose tissue (VAT) – with white matter (WM) integrity using a whole-brain approach in military pilots. Twenty-three military helicopter pilots (Mage = 36.79; SD = 8.00; MBMI = 25.48; SD = 2.49) took part in the study. Brain volumes were studied using diffusion tensor imaging technique by means of a 3T Magnetom Tim Trio. Measurements of body mass index (BMI), TFM and VAT were obtained using Dual-energy X-ray Absorptiometry (DXA). The results showed that, on one hand, higher TFM was associated with higher white matter fractional anisotropy (FA) and, on the other hand, higher VAT was associated with lower FA. Data showed that TFM and VAT are the critical factors underlying WM integrity in combat helicopter pilots. The authors suggest that fat presence enhance brain connectivity while there is no excess, specifically in VAT.
Similar content being viewed by others
Introduction
Military pilots are exposed to uncertain scenarios in extreme conditions where an incorrect decision may have catastrophic consequences, and thus, the assessment of brain function may help to evaluate the cognitive capabilities of pilots and predict their behaviour in challenging situations1. In recent decades, there has been a growing interest in analysing the relationships among body composition, physical fitness and brain function. Several brain imaging studies have shown an association between adiposity and decreased global brain volume2, as well as reduced volume of grey matter3 (GM) and white matter4 (WM). Related to this topic, the accumulated evidence has demonstrated that obesity raises the risk of cognitive decline and dementia. Indeed, it has been associated with structural brain changes in bilateral temporal lobes, anterior lobe of the cerebellum, frontal lobes, temporal lobes, anterior lobe of the cerebellum, occipital lobe, frontal lobe and precuneus3 and impaired functional connectivity5. Taking these results into account, we suggest that the putative link between functional brain alterations and body fat is worthy of study in this particular population.
A large number of studies have estimated adiposity with anthropometric measures, with body mass index (BMI) being the most commonly used method. However, the validity of BMI in the study of the relationship between body composition and brain structure and function is somewhat limited and may not fully assess the role of adipose tissue in conferring risk for structural brain alterations6. Nevertheless, as BMI is a proximate measure for the degree of adiposity present in the body, it is reasonable to consider the results of other studies with overweight and obese participants in which the BMI and WM relationship was observed5. However, the participants of this study are mostly normal-weight, thus different fat compartments were considered as variables of body composition instead of BMI: visceral adipose tissue (VAT) and total fat mass (TFM).
The assessment of WM microstructural changes of the human brain has been widely described from in vivo studies using diffusion tensor imaging7 (DTI). Many diffusion parameters can be calculated by DTI because of its capacity to evaluate the orientation and magnitude of water diffusion in the whole brain tissue8 allowing to observe the relationship between WM integrity and body composition. Concretely, the indicators of WM integrity observed in this research were fractional anisotropy (FA), considered as the directionality of water diffusivity degree, mean diffusivity (MD), an indicator of average molecular motion, and both radial diffusivity (RD) and axial diffusivity (AD), which are MD perpendicular and parallel to axonal fibres respectively.
In this study, we aimed to investigate the relationship of different body fat compartments – (TFM) and (VAT) separately – with WM integrity using a whole-brain approach. To the best of our knowledge, no previous studies have included people whose BMI is normal and their TFM and VAT are low, as may be expected in military pilots.
Results
Overall summary
The correlation analysis revealed that higher TFM is associated with higher FA and higher VAT with lower FA, while no significant results were found in MD, RD and AD. Means, standard deviations, minimum and maximum values and 95% confidence intervals for the mean for each variable of the study are displayed in Table 1.
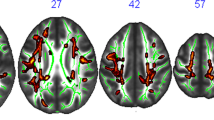
Total fat mass and fractional anisotropy analysis
Statistically significant correlations of TFM with white matter fractional anisotropy are reported in Table 2 and depicted in Fig. 1. We observed positive associations of TFM with a set of clusters in the left and right hemispheres, encompassing tracts such as the sagittal stratum, left anterior thalamic radiation, left forceps minor, left inferior fronto-occipital fasciculus, left uncinate fasciculus, left anterior thalamic radiation, right inferior longitudinal fasciculus, right inferior fronto-occipital fasciculus, right splenium of the corpus callosum, forceps major, right inferior longitudinal fasciculus, right inferior fronto-occipital fasciculus (temporal part), right superior longitudinal fasciculus and right anterior thalamic radiation.
Visceral adipose tissue and fractional anisotropy analysis
The correlations between VAT and white matter FA are displayed in Table 3 and Fig. 2. VAT is negatively related to FA in a set of clusters in both hemispheres, involving thalamic radiations, the longitudinal fasciculus, right inferior fronto-occipital fasciculus, sagittal striatum, left inferior fronto-occipital, longitudinal and superior fasciculus; anterior thalamic radiation, the right Genu of the corpus callosum; forceps minor; left posterior thalamic radiation (includes optic radiation); inferior fronto-occipital fasciculus; inferior longitudinal fasciculus; superior longitudinal fasciculus; forceps major, left corticospinal tract; and anterior thalamic radiation Fig. 3.
Discussion
The foremost goal of this study was to examine the possible associations of total fat mass (TFM) and visceral adipose tissue (VAT) with white matter (WM) integrity of subcortical structures on normal-weight individuals (military pilots), through fractional anisotropy (FA), mean diffusivity (MD), radial diffusivity (RD) and axial diffusivity(AD). Most of the previous research has mainly focused this relationship between the total brain volume, grey thickness or white matter, but less on WM integrity. Our results show that the percentages of VAT and TFM correlate negatively and positively with the FA respectively, but not with MD, RD and AD. A possible reason for these not significant results is that, in this population, different fat compartments are not associated with the molecular diffusion rate and myelin presence.
Our results showing that higher presence of VAT is associated with lower FA, are in line with those of other studies aimed at analysing the possible association between body fat mass with brain structure and function principally in obese and elderly people. There is evidence suggesting that adiposity and obesity are associated with altered functional connectivity across different brain regions9 and with normal-weight population has been reported that higher VAT is associated with lower functional brain connectivity5. Additionally, it seems that several multiple measures of brain microstructure impairs with adiposity10. For example, anthropometric and cortical thickness-based measures of visceral fat had a significant inverse association with total brain volume in middle-aged individuals11.
Concerning TFM, we observed that in contrary with VAT, is associated with higher FA. To the best of our knowledge, this result is not very present in the literature, perhaps because our participants were physically active and most of them had a BMI of normal-weight. Only one research had a similar result to ours: a cross-sectional study of more than three thousand participants conducted by Croll et al.12 revealed that higher fat mass is associated with higher FA. Some sample characteristics are quite similar to our study: BMI mean was 27.2 ± 3.9 and they were physically active, although the great differences are that it was composed of elderly people (age mean = 65.9 ± 11.1) and 57.3% were women. Nevertheless, these results support the idea that more studies in which different fat compartments are assessed along with participants with different BMI and not only obese or overweight people are needed.
In overall, these findings are somewhat unexpected, since the associations of TFM and VAT with brain connectivity demonstrate opposite directions. A possible explanation of this result could rely on the different metabolic and endocrine functions associated with different fat compartments. The distribution of body fat is crucial to understanding the adverse effects of obesity13. In this respect, brain alterations caused by neurodegenerative, vascular and metabolic disorders have been associated with obesity, particularly with VAT compartment14. However, the analysis of subcutaneous fat in participants with acute ischemic stroke did not show correlation with the volume of white matter lesions13.
Nevertheless, our findings showed that TFM is positively related to white matter FA in some specific tracts, which may be related to better cognitive function since WM microstructural integrity mediates communications in the brain15.
Taking into account the results of the studies described above, and according to our data, it is sound to consider that, in normal-weight population, a certain amount of fat cells may be needed to ensure white matter integrity, while an accumulation on the visceral compartment would hamper the brain connectivity.
It is far to be understood the physiological pathways associated with structural brain changes or connectivity and body fat accumulation. On one hand, there are positive effects associated with adiposity. Several studies have reported that leptin, which is correlated with visceral adiposity, is crucial in the coordination of the excitatory synaptic transmission aroused at hippocampal Schaffer-collateral (SC)-CA1 synapses16,17,18,19. Leptin receptors are present in various regions of the hippocampus, concretely at hippocampal synapses20,21. Moreover, in studies with leptin-insensitive rodents, an impairment in the hippocampal-dependent memory area was observed22,23. Thus, it is reasonable to consider that leptin potentially enhance cognitive functions24.
Additionally, insulin—which is also correlated with visceral adiposity25,26- influences memory processing27,28,29. Most of the insulin receptors are located in areas with an important role in declarative memory formation: the hippocampus and connected limbic brain structures30,31,32,33. In insulin-administered studies, both intravenous and intranasal administrations have reported an improvement in declarative memory29,34. Although it is not clear the mechanisms responsible for this improvement in memory function, Benedict et al.34 considered that if there is a gradual plastic neuronal change -because of the slow enhancement of memory after insulin inoculation- and that, additionally, improves synaptic plasticity35,36, then insulin supports and protects the hippocampal neural connectivity development and, consequently, improves declarative memory.
On the other hand, it is widely accepted that the increase in adipose tissue activity is related to chronic low-grade inflammation37 and increasing release of inflammatory cytokines such as leptin, which affects – at least in pathologic conditions38,39- the central nervous system due to the activation of microglial cells. Moreover, inflammation could exert deleterious effects on brain integrity through oxidative stress40. Another potential mechanism of the negative impact of inflammation on brain integrity is through impairing endothelial function employing a diminished production of nitric oxide41. This vasodilator is critical for regulating blood flow in the central nervous system since it helps to maintain resting vascular tone and regulates local flow adjustments in response to hypercapnia demands42.
In summary, it seems that adiposity provides both positive and negative effects on brain connectivity. In fact, obesity studies reported that visceral adiposity and BMI –which could be interpreted as the total fat present in the body in overweight and obese populations5- are negatively associated with brain connectivity9,10,11, while other studies with normal weight populations such as Croll et al.12 and ours observed that TFM is positively associated with brain connectivity. According to this information, the authors suggest that the presence of fat may enhance brain connectivity and, probably, overall brain health. However, the accumulation of fat, especially VAT, may hamper brain connectivity. Hence, the presence of fat cells could improve brain health as long as there is no excess, although the mechanisms are not well understood.
Beyond the lack of information on causal directionality, conclusions from the present work are affected by other limitations. The most important is the results reliability, which is limited due to the relatively small sample size in spite of including the entire team of active combat helicopter military pilots in the Spanish Army, although it may be enough to reveal certain patterns considering that the population is rather homogeneous. Future interventions and longitudinal studies should be carried out to assess the relative contribution of each causal fat compartment. Considering that the findings from this study are not fully consistent with the literature, it is necessary to perform further DTI studies aimed at exploring the relationship between TFM/VAT and WM integrity.
In conclusion, DTI results of the present study with combat helicopter military pilots revealed that higher FA is associated with lower VAT and, surprisingly, with higher TFM. The authors suggest that, when there is no excess, fat mass may enhance brain connectivity, while an accumulation of VAT could deteriorate it.
Material and Methods
Ethical approval
Recruitment and experimental procedures for this study complied with the Declaration of Helsinki and were approved by the Institutional Review Board (IRB) of the University of Granada, Spain (IRB approval: 850 and 12/CEIH2016). Written informed consent was obtained from each participant prior to the study.
Participants
Twenty-three military helicopter pilots (Mage = 36.79; SD = 8.00; MBMI = 25.48; SD = 2.49) from the Spanish Army Airmobile Force (FAMET), serving at the Almagro airbase, Ciudad Real (Spain), took part in the study. The sample size was limited by participants’ availability. All pilots were members of the Attack Helicopter Battalion BHELA I. Fifteen were qualified to fly the EC665 Tigre attack helicopter, constituting the entire active team of Spanish Tigre pilots, and eight out of the twenty-three flew the Messerschmitt-Bölkow-Blohm Bo 105 helicopter. All volunteers were on flight status, had a recent verification of good health and were free of medication. Academic training and military ranking were diversified, between the level of brigadier and lieutenant colonel.
Variables and instruments
Analysis of cerebral connectivity
Regarding the analysis of cerebral connectivity, T1-weighted and DTI volumes were acquired using 32-channel Siemens 3 T Magneton TRIO system located at the Mind, Brain and Behaviour Research Centre (CIMCYC) at the University of Granada. The T1 MPRAGE parameters were: TR = 1900 ms; and TE = 2.52 ms; FA = 9°). A total of 176 slices of a thickness of 1 mm of the whole brain were obtained (voxel size = 1 × 1 × 1 mm3, FOV = 256 mm, 256 × 256 data acquisition matrix).
Diffusion images were acquired on the same scanner using a 2D EPI diffusion sequence, with the following parameters: TE = 90 ms and TR = 3300 ms. A DTI diffusion plan was used, and a total of 30 sampling directions, repeated 3 times. In addition, 3 b0 volumes were obtained. The value of b was 1000 s/mm2. The in-plane resolution was 1,797 mm. The thickness of the slice was 5.2 mm. The DTI volumes were analysed with the FDT program43, a part of the library FMRIB, v5.544. The images were corrected by a brain mask created from the b0 images, and the FA maps were obtained by applying dtifit to the masked volumes. The analysis was carried out using the tract-based spatial statistical package (TBSS). The FA maps were recorded by the standard FA template FSL in MNI (Montreal Neurological Institute) space using FNIRT. The mean volume FA was used to skeletonize the individual normalised FA maps. This skeletonization is assumed to be the centre of all sections following a given path. The individual maps of the FA were projected to these skeletons and voxel-wise analysed using Threshold-free Cluster Enhancement (TFCE, a part of the FMNI library).
Body composition
Dual-energy X-ray Absorptiometry (DXA) fan-beam technology (Hologic QDR 4500 A, Hologic) was used for the measurement of BMI, TFM and VAT. A standardized procedure for patient positioning and utilization of the QDR software was used. The DXA 4500 A scans were analysed with the software version 8.21.
Statistical analysis
Data summaries were computed for the whole sample. Shapiro-Wilk’s tests indicated normality for the variables of interest. For each correlation analysis (TFM and VAT), a total of 2,500 random extractions were given to obtain an empirical distribution of the correlation coefficient. A TFCE corrected for a multiple comparisons p-value of 0.05 was used.
Data availability
The corresponding author had full access to all the data in the study and all authors shared final responsibility for the decision to submit for publication. The database is available without restriction in the Open Science Framework (OSF) website, https://osf.io/kq8ph/.
References
Borghini, G., Astolfi, L., Vecchiato, G., Mattia, D. & Babiloni, F. Measuring neurophysiological signals in aircraft pilots and car drivers for the assessment of mental workload, fatigue and drowsiness. Neuroscience & Biobehavioral Reviews 44, 58–75 (2014).
Ward, M. A., Carlsson, C. M., Trivedi, M. A., Sager, M. A. & Johnson, S. C. The effect of body mass index on global brain volume in middle-aged adults: a cross sectional study. BMC neurology 5, 23 (2005).
Taki, Y. et al. Relationship between body mass index and gray matter volume in 1,428 healthy individuals. Obesity 16, 119–124 (2008).
Gustafson, D. R., Steen, B. & Skoog, I. Body mass index and white matter lesions in elderly women. An 18-year longitudinal study. International Psychogeriatrics 16, 327–336 (2004).
Raschpichler, M. et al. Abdominal fat distribution and its relationship to brain changes: the differential effects of age on cerebellar structure and function: a cross-sectional, exploratory study. BMJ open 3, e001915 (2013).
Bettcher, B. M. et al. Body mass and white matter integrity: the influence of vascular and inflammatory markers. PloS one 8, e77741 (2013).
Pierpaoli, C., Jezzard, P., Basser, P. J., Barnett, A. & Di Chiro, G. Diffusion tensor MR imaging of the human brain. Radiology 201, 637–648 (1996).
Piervincenzi, C. et al. White Matter microstructural changes following Quadrato motor training: a longitudinal study. Frontiers in human neuroscience 11, 590 (2017).
García‐García, I. et al. Alterations of the salience network in obesity: a resting‐state fMRI study. Human brain mapping 34, 2786–2797 (2013).
Gianaros, P. J., Marsland, A. L., Sheu, L. K., Erickson, K. I. & Verstynen, T. D. Inflammatory pathways link socioeconomic inequalities to white matter architecture. Cerebral cortex 23, 2058–2071 (2012).
Debette, S. et al. Visceral fat is associated with lower brain volume in healthy middle‐aged adults. Annals of neurology 68, 136–144 (2010).
Croll, P. H. et al. Body composition is not related to structural or vascular brain changes. Frontiers in neurology 10, 559 (2019).
Widya, R. L. et al. Visceral adipose tissue is associated with microstructural brain tissue damage. Obesity 23, 1092–1096 (2015).
Jagust, W., Harvey, D., Mungas, D. & Haan, M. Central obesity and the aging brain. Archives of neurology 62, 1545–1548 (2005).
van Tilborg, E. et al. Origin and dynamics of oligodendrocytes in the developing brain: Implications for perinatal white matter injury. Glia 66, 221–238 (2018).
Shanley, L. J., Irving, A. J. & Harvey, J. Leptin enhances NMDA receptor function and modulates hippocampal synaptic plasticity. Journal of Neuroscience 21, RC186–RC186 (2001).
Oomura, Y. et al. Leptin facilitates learning and memory performance and enhances hippocampal CA1 long-term potentiation and CaMK II phosphorylation in rats. Peptides 27, 2738–2749 (2006).
Moult, P. R. et al. Leptin regulates AMPA receptor trafficking via PTEN inhibition. Journal of Neuroscience 30, 4088–4101 (2010).
Moult, P. R. & Harvey, J. NMDA receptor subunit composition determines the polarity of leptin-induced synaptic plasticity. Neuropharmacology 61, 924–936 (2011).
Håkansson, M.-L., Brown, H., Ghilardi, N., Skoda, R. C. & Meister, B. Leptin receptor immunoreactivity in chemically defined target neurons of the hypothalamus. Journal of Neuroscience 18, 559–572 (1998).
Shanley, L. J., O’Malley, D., Irving, A., Ashford, M. & Harvey, J. Leptin inhibits epileptiform-like activity in rat hippocampal neurones via PI 3-kinase‐driven activation of BK channels. The Journal of physiology 545, 933–944 (2002).
Li, X.-L. et al. Impairment of long-term potentiation and spatial memory in leptin receptor-deficient rodents. Neuroscience 113, 607–615 (2002).
Winocur, G. et al. Memory impairment in obese Zucker rats: an investigation of cognitive function in an animal model of insulin resistance and obesity. Behavioral neuroscience 119, 1389 (2005).
Harvey, J. & McGregor, G. Regulation of hippocampal synaptic function by the metabolic hormone, leptin: Implications for health and neurodegenerative disease. Frontiers in cellular neuroscience 12, 340 (2018).
Woods, S. C., Seeley, R. J., Porte, D. & Schwartz, M. W. Signals that regulate food intake and energy homeostasis. Science 280, 1378–1383 (1998).
Benoit, S. C., Clegg, D. J., Seeley, R. J. & Woods, S. C. Insulin and leptin as adiposity signals. Recent progress in hormone research 59, 267–286 (2004).
Marfaing, P. et al. Effects of hyperinsulinemia on local cerebral insulin binding and glucose utilization in normoglycemic awake rats. Neuroscience letters 115, 279–285 (1990).
Park, C. R., Seeley, R. J., Craft, S. & Woods, S. C. Intracerebroventricular insulin enhances memory in a passive-avoidance task. Physiology & behavior 68, 509–514 (2000).
Kern, W. et al. Improving influence of insulin on cognitive functions in humans. Neuroendocrinology 74, 270–280 (2001).
Unger, J. W., Livingston, J. N. & Moss, A. M. Insulin receptors in the central nervous system: localization, signalling mechanisms and functional aspects. Progress in neurobiology 36, 343–362 (1991).
Lannert, H. & Hoyer, S. Intracerebroventricular administration of streptozotocin causes long-term diminutions in learning and memory abilities and in cerebral energy metabolism in adult rats. Behavioral neuroscience 112, 1199 (1998).
Squire, L. R. Memory and the hippocampus: a synthesis from findings with rats, monkeys, and humans. Psychological review 99, 195 (1992).
Eichenbaum, H. The hippocampus and declarative memory: cognitive mechanisms and neural codes. Behavioural brain research 127, 199–207 (2001).
Benedict, C. et al. Intranasal insulin improves memory in humans. Psychoneuroendocrinology 29, 1326–1334 (2004).
Wozniak, M., Rydzewski, B., Baker, S. P. & Raizada, M. K. The cellular and physiological actions of insulin in the central nervous system. Neurochemistry international 22, 1–10 (1993).
Fields, R. D. & Stevens-Graham, B. New insights into neuron-glia communication. Science 298, 556–562 (2002).
Pou, K., Massaro, J. & Hoffmann, U. The Framingham Heart Study. Visceral and subcutaneous adipose tissue volumes are cross-sectionally related to markers of inflammation and oxidative stress. Circulation 116, 1234–1241 (2007).
Münzberg, H. & Morrison, C. D. Structure, production and signaling of leptin. Metabolism 64, 13–23 (2015).
Gao, Y. et al. Hormones and diet, but not body weight, control hypothalamic microglial activity. Glia 62, 17–25 (2014).
Kaur, S. S. et al. Inflammation as a mediator of the relationship between cortical thickness and metabolic syndrome. Brain imaging and behavior 9, 737–743 (2015).
Di Francescomarino, S., Sciartilli, A., Di Valerio, V., Di Baldassarre, A. & Gallina, S. The effect of physical exercise on endothelial function. Sports Medicine 39, 797–812 (2009).
Lavi, S., Egbarya, R., Lavi, R. & Jacob, G. Role of nitric oxide in the regulation of cerebral blood flow in humans: chemoregulation versus mechanoregulation. Circulation 107, 1901–1905 (2003).
Behrens, T. E. et al. Characterization and propagation of uncertainty in diffusion-weighted MR imaging. Magnetic Resonance in Medicine: An Official Journal of the International Society for Magnetic Resonance in Medicine 50, 1077–1088 (2003).
Jenkinson, M., Beckmann, C. F., Behrens, T. E., Woolrich, M. W. & Smith, S. M. Fsl. Neuroimage 62, 782–790 (2012).
Acknowledgements
Research by D.C., I.M., J.V. and F.A. is funded by the Spanish Ministry of Economy and Competitiveness (Agencia Estatal de Investigación) grant DEP2017-89879-R . Also, funding was provided by CEMIX (Centro Mixto UGR-MADOC, Spain) grant PIN 11. The authors are indebted to Juan F. Navas for his help in crafting the article. The authors deeply thank the collaboration of the pilots of BHELA-1, their commanders, specially Lieutenant-Colonel Santiago Juan Fenández Ortiz-Repiso and commander Alberto José Cherino Muñoz, and the personnel of MADOC (Army of Spain), especially Lieutenant-Colonel Lorenzo Rebollo Gómez.
Author information
Authors and Affiliations
Contributions
D.C., F.A. and A.C. conceptualised the research study and its hypotheses. Data collection was performed by C.T., I.M. and J.V.A.C. performed the analysis. The manuscript was written and edited by D.C., I.M., F.A., C.T., J.V., R.J. and A.C.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cárdenas, D., Madinabeitia, I., Vera, J. et al. Better brain connectivity is associated with higher total fat mass and lower visceral adipose tissue in military pilots. Sci Rep 10, 610 (2020). https://doi.org/10.1038/s41598-019-57345-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-57345-3
This article is cited by
-
Changes in physical fitness and body composition of pilot cadets before and after a process of directed flight preparation
BMC Sports Science, Medicine and Rehabilitation (2022)
-
Dynapenic abdominal obesity is associated with mild cognitive impairment in patients with cardiometabolic disease: a cross-sectional study
BMC Geriatrics (2022)
-
Association of life course adiposity with risk of incident dementia: a prospective cohort study of 322,336 participants
Molecular Psychiatry (2022)
-
The Potential Crosstalk Between the Brain and Visceral Adipose Tissue in Alzheimer’s Development
Neurochemical Research (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.