Abstract
Carfilzomib-lenalidomide-dexamethasone (KRd) therapy has yielded promising results in patients with newly diagnosed multiple myeloma (NDMM). Cereblon (CRBN) is the direct molecular target of lenalidomide and genetic polymorphisms in CRBN have been associated with lenalidomide efficacy. In this study, we assessed the correlation of five single nucleotide variants (SNVs) in the CRBN gene with clinical response and outcomes in patients with NDMM administered KRd therapy with lenalidomide maintenance, achieving favorable trial endpoints in a prospective Phase II study (NCT01402284). Of the observed SNVs, no associations with KRd therapy response were found in this patient cohort, although strong trends in hypoalbuminemia grade and hyperbilirubinemia grade emerged across the CRBN rs1672753 genotype (P = 0.0008) and the rs1714327 genotype (P = 0.0010), respectively. Our results do not provide conclusive support for the predictive utility of CRBN gene polymorphisms as potential biomarkers of clinical response to lenalidomide-based therapy in our patient population. However, these findings remain to be validated in prospective studies using larger patient populations.
Similar content being viewed by others
Introduction
Thalidomide and its derivatives, the immunomodulatory drugs (IMiDs) lenalidomide and pomalidomide, are used to treat several hematological malignancies, including multiple myeloma (MM)1,2. Although only 30% of patients respond to IMiDs used as single agents3, triplet combination therapies involving a proteasome inhibitor (carfilzomib), immunomodulatory agent (lenalidomide), and a corticosteroid (dexamethasone) are clinically effective, yielding complete or deep responses in patients with newly diagnosed multiple myeloma (NDMM)4,5 and relapsed or refractory MM6. Carfilzomib-lenalidomide-dexamethasone (KRd) therapy has resulted in improved progression-free survival (PFS) over administration of lenalidomide and dexamethasone alone2,5,6.
The anti-myeloma activity of IMiDs has been attributed to several mechanisms of action, including anti-angiogenic, pro-apoptotic, and anti-proliferative effects1,7. Until recently, however, the precise molecular mechanisms by which thalidomide and its analogs act remained elusive. A body of preclinical evidence now exists showing that cereblon (CRBN), a ubiquitously expressed E3 ligase protein, is the direct molecular target of IMiDs8,9 and its presence is indispensable for IMiD activity3. First identified in patients with non-syndromic mental retardation10, CRBN has since been studied in vitro in MM, myelodysplastic syndrome, and lymphoma cell lines9, in vivo using zebrafish, chick, and rodent animal models8,11,12,13,14, and in pre- and post-IMiD treatment tissue samples collected from patients with MM3. Upon binding to cereblon, IMiDs induce CRBN-dependent proteasomal degradation and inhibition of IKZF1/3, B cell-specific transcription factors required for both myeloma cell viability and activation of the immune system1,2,7.
Recent studies have established a correlation between CRBN expression levels and clinical response to IMiD treatment. High expression of CRBN in patients with NDMM continuing on daily thalidomide maintenance for 2 years was associated with longer PFS and treatment response (P = 0.005)15, and has also been shown to enhance the effects of lenalidomide therapy and potentially overcome resistance to treatment3,16,17,18. Conversely, reduced CRBN expression levels have been linked to the development of lenalidomide resistance in human myeloma cells3 as well as poor clinical outcomes in patients with either MM3 or lower risk myelodysplastic syndrome16. Diminished CRBN protein levels was specifically associated with the development of lenalidomide resistance over the course of treatment in 77% of lenalidomide-refractory MM patients, although baseline CRBN expression at diagnosis did not affect overall survival (OS)19. In another study of 53 refractory MM patients treated with pomalidomide, CRBN levels were predictive of decreased response rates and significant differences in both PFS (P < 0.001) and OS (P = 0.01)20.
Whether these associations may be driven by genetic variations in the CRBN gene remains unknown, as there are currently no clear biomarkers that predict response to lenalidomide therapy. Attempts to quantify cereblon’s utility as a clinical biomarker for IMiDs is ongoing20,21,22,23. One study found an increased prevalence of mutations in both CRBN and the CRBN pathway impacting CRBN-IMiD interactions in patients with multidrug refractory disease, and subsequently observed conferred lenalidomide resistance in vitro following the functional introduction of these mutations in MM cells24. A recent analysis of acquired pomalidomide-resistance in MM cell lines similarly revealed a range of CRBN mutations and CRBN protein loss associated with treatment resistance25. Given the documented association between CRBN expression and IMiD treatment response in patients with MM, some studies have also begun to explore single nucleotide variants (SNVs) in the CRBN gene as potentially useful biomarkers for the clinical assessment of antimyeloma efficacy, or patient selection for predicted responders before initiating therapy. In a cohort of 144 MM patients compared to 237 matched healthy individuals, two SNVs (rs711613C > T and rs1045433C > T) within the non-coding regions of the CRBN gene (intron 1 and 3′-untranslated region, respectively), thought to control CRBN expression, correlated with major differences in MM susceptibility, progression, and response to treatment26. Carriers of the rs711613 major allele demonstrated better response to thalidomide treatment (P = 0.023), while the rs1045433 minor allele was found to be more common, but not statistically significant, in patients with complete or partial response after thalidomide treatment (P = 0.092).
The role of CRBN genetic variations as biomarkers that may predict clinical response to IMiD-based therapy remains controversial due to inconsistent findings. Two studies examining a SNV located at -29 nucleotides of the 5′-untranslated region (5′UTR) (rs1672753 C > T) yielded contradictory results on the predominance of each allele in myelodysplastic patients, as compared to healthy controls16,27. More recently, this SNV was found to have a significant impact on survival outcomes in patients with MM, conferring extended PFS (P = 0.005) and OS (P = 0.023) in patients with the variant genotypes compared to those with two major alleles, independent of thalidomide therapy28. Another study consisting of 68 thalidomide-treated patients with MM conversely identified the major allele to be associated with significantly shorter PFS (P = 0.0321), without significantly impacting OS29. In another cohort of 169 patients with refractory or relapsed MM treated with lenalidomide regimens, minor allele carriers of two other naturally occurring SNVs (rs1714327C > G and rs1705814C > T) were associated with worse clinical response and shorter PFS (OR = 2.49, P = 0.0054)30. Therefore, whether CRBN genetic variations can be prognostic markers of myeloma cell biology or predictive biomarkers of clinical response to IMiD-based therapy remain to be determined.
We previously reported results from a prospective Phase II study that included patients with NDMM treated with 8 cycles of KRd therapy, followed by two years of lenalidomide maintenance (KRd-R)5. In this patient cohort, this therapy regimen was found to be highly tolerable and demonstrated high rates of MRD negativity, translating into 12-month longer PFS (P < 0.001). The five-year followup to this study demonstrated long term survival benefits, with KRd-R treatment leading to a rapid, deep, and durable overall response rate and sustained MRD-negative complete responses (CRs)31. Given cereblon’s central role as a direct molecular target of thalidomide and its analogs, we sought to determine whether CRBN genetic variants may predict for the impressive clinical response observed for this patient population on KRd-R therapy. In the current study, the same patient cohort was genotyped for five CRBN polymorphisms (rs1714327 C > G, rs1672753 C > T, rs1045433 C > T, rs1705814 C > T, rs711613 C > T). To our knowledge, this study comprises the largest array of CRBN SNVs studied for associations with favorable clinical outcomes following KRd-R therapy among a single patient cohort. We assessed for correlations between these CRBN SNVs and clinical progression, response to treatment, and toxicity.
Results and Discussion
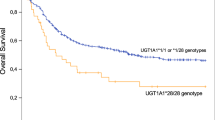
We aimed to assess the prognostic significance of previously described SNVs in the CRBN gene, which may affect the expression, activity, or alternative splicing of its protein, in a single cohort of patients with NDMM demonstrating impressive survival benefits following lenalidomide therapy. We chose a patient population demonstrating promising clinical outcomes, with an overall response rate of 100%5, and previously reported differences in mutational patterns between patients with early and later stage disease32. Five SNVs in CRBN (rs1714327 C > G, n = 42; rs1672753 C > T, n = 40; rs1045433 C > T, n = 43; rs1705814 C > T, n = 44; rs711613 C > T, n = 43) were detected, although low frequencies of homozygous genotypes and the number of determined SNVs limited the power of statistical analyses. The distribution of the CRBN genotypes was not significantly correlated with patient demographics, disease markers or baseline laboratory findings (data not shown). Of the observed SNVs, none of the variants appeared to be associated with KRd-R therapy response and/or minimum residual disease status in this patient cohort (Table 1). All patients carrying homozygous wild-type alleles of two SNVs (rs1672753 CC, rs1705814 CC) were MRD-negative (3/3, 7/7), compared to 77% (27/35) and 71% (25/35) of patients carrying variant alleles. Additionally, none of the observed genotypes appeared to be related to progression-free survival (Table 2). Assessing for genotype versus toxicities, all toxicities with sufficient data were tested for associations with CRBN SNVs (Supplementary Table 1). Strong trends in hypoalbuminemia grade and hyperbilirubinemia grade emerged across the CRBN rs1672753 genotype (P = 0.0008) and the rs1714327 genotype (P = 0.0010), respectively (Table 3). Analysis using Somers’ D statistic indicates that the associations are strong with the rs1672753 variant genotypes having higher hypoalbuminemia grade (D = 0.53) and with the rs1714327 wild-type genotype having higher hyperbilirubinemia grade (D = −0.45) (Supplementary Table 2). The significance of these associations and their relevance as potential biomarkers remain to be determined.
The discovery of cereblon as the direct target of thalidomide and its derivatives has significantly heightened interest in its potential use as a biomarker of clinical response and outcome3,15,33,34. Cereblon is a necessary component of the cullin ring E3 ubiquitin ligase complex required for lenalidomide efficacy15,34 and specific CRBN variants are thought to be potential genetic markers of clinical response or outcome following KRd therapy in patients with MM26. To date, the role of CRBN as a biomarker for treatment response and/or resistance has not been strongly established, and these findings on the association of CRBN SNVs with patient outcomes remain controversial21,24,35,36. For example, a recent analysis of CRBN gene expression levels in patients enrolled in STRATUS, a Phase IIIb study evaluating the safety and efficacy of pomalidomide treatment, found no notable difference in overall response rate in high versus low CRBN expressers37, despite previously documented associations between CRBN expression and IMiD treatment response in patients with MM18,20,38.
Due to insufficient data on CRBN gene variants and their impact on clinical response to therapy, larger scale studies are needed to determine the prognostic significance of CRBN SNVs. The reported incidence of direct polymorphisms in CRBN and in publicly available MM sequencing data is low, except in single case reports or in vitro cell line studies24,36,39. A similar genotyping study on the effects of a CRBN coding region SNV (rs121918368 C > T) only detected the wild-type allele in the genotyped patient cohort34, while another study failed to identify any CRBN or CRBN pathway variants in all samples analyzed from a cohort of 21 patients with MM35. Likewise, our study was limited by a small sample size in patient subgroups and few progressions, thus the results should be viewed cautiously. Discrepancies reported in previous studies indicate a need for larger patient cohorts to confirm our findings, which warrant future replication studies with expanded study groups to examine the potential predictive utility of CRBN SNVs as biomarkers16,21,27,36.
Future genotyping studies would further benefit from a thorough functional analysis of the investigated CRBN genetic variants to elucidate the biological mechanisms underlying any potential associations with response to lenalidomide therapy. Three of the substitutions chosen (rs711613 C > T, rs1045433 C > T, and rs1672753 C > T) are located in non-coding regions of CRBN (intron 1, 3′UTR, and 5′UTR, respectively), which may be associated with lenalidomide efficacy26. However, the exact functional consequences of the SNVs investigated in this study are currently unknown. Potential mechanisms underlying the effects of cereblon include modulation of its gene and protein expression or alternative splicing, particularly via removal of exon 10 containing the IMiD-binding domain15,16,21.
A molecular analysis of cereblon-related resistance to IMiD therapy in a longitudinal study of 1000 patients with NDMM from multiple clinical sites revealed a subset of IMiD-treated patients exhibiting significant reductions in CRBN expression and copy number loss at relapse compared to baseline levels, whereas patients with copy number gains at baseline appeared to benefit from IMiD therapy40. Given the central role of cereblon as a substrate receptor within the E3 ubiquitin ligase complex, which contains other proteins required to carry out the ubiquitination functions regulating MM cell survival, the substrate specificity and/or ability of cereblon to recognize or bind to its partners may additionally be determined by CRBN genetic variants10. Other studies have proposed alternative mechanisms including epigenetic, transcriptional, and/or post-transcriptional modulation of CRBN gene expression that may drive clinical response to lenalidomide therapy20,36,41. In addition, mutational screening of NDMM patients receiving lenalidomide in the Phase II GEM10MAS65 trial implicated several downstream genes in the CRBN pathway (such as IKZF1, IKZF2, IRF4, and MYC) as other potential biomarkers of lenalidomide resistance42. Molecular studies have also implicated alternative binding targets43,44 and mechanisms of action8,14,45, which may be cell-type specific, and (by extension) disease-specific, which may explain the variability in reported correlations between CRBN expression and patient response to IMiDs. Although CRBN is known to be the direct target of lenalidomide and its presence is essential to IMiD activity, whether IMiDs may target other molecules downstream of CRBN and/or different signaling pathways resulting in treatment resistance has not been well established3.
We previously reported results from a clinical study with positive trial endpoints using the same cohort of lenalidomide-treated NDMM patients5. Our group identified putative VEGF and VEGFR2 SNVs that may be possible markers of clinical response following KRd combination therapy46. Moreover, we recently identified a significant mutational burden in our patient population of NDMM of recurrent genetic mutations implicated in MM32. The current exploratory genotyping study was the first, to the best of our knowledge, to evaluate the association of multiple CRBN genetic variations with clinical response and outcome within a patient population demonstrating impressive survival benefits, including an 100% overall response rate. While we did not find any significant correlations of these five CRBN variants with either treatment response or progression-free survival in our limited patient population, whether CRBN polymorphisms have a role as predictive biomarkers of response and/or outcome needs to be verified in other MM patients on KRd therapy. Future genetic and functional studies of these causal variants are warranted to confirm the findings observed from this patient population. An improved understanding of the molecular consequences of CRBN polymorphisms may aid the development of personalized treatment regimens for MM and address whether these SNVs may serve as promising biomarkers for lenalidomide-based therapy.
Methods
Patients
Patients (n = 45) with newly diagnosed multiple myeloma (NDMM) were enrolled in a prospective Phase II study (NCT01402284) and received eight 28-day cycles of KRd followed by lenalidomide maintenance for 2 years after completing 8 cycles of the combination therapy. Details regarding patient characteristics, response criteria, minimum residual diseases (MRD) monitoring methods, dosing regimens, and pharmacokinetics data have been previously reported47. The studies were approved by the Institutional Review Board at the National Cancer Institute, and all participants provided written informed consent. All research methods were performed in accordance with relevant guidelines and regulations.
Genotyping
A QiaBlood DNA extraction kit was used to extract DNA from samples of whole blood, as per the manufacturer’s instructions (Qiagen, Valencia, CA). Primer pairs were designed or used as previously published27 to amplify and determine CRBN polymorphisms using a nested PCR protocol. Big Dye Terminator Cycle Sequencing Ready Reaction kit V1.1 was used to perform direct nucleotide sequencing PCR on an ABI Prism 310 Genetic Analyzer (Applied BioSystems, Foster City, CA). Quality of the amplified PCR products was verified by agarose gel electrophoresis for each sample tested. The primer sequences for each SNV are listed in Supplementary Table 3. The genotype analysis was performed independently by two persons and repeat sequence analysis was performed to confirm all individuals expressing the variant genotypes.
Statistical considerations
Trends in continuous distributions and dichotomous factors across three genotypes were assessed using the Jonckheere-Terpstra and Cochran-Armitage tests, respectively, while the Wilcoxon rank sum test and Fisher’s exact test were used for comparisons of two genotypes or groups. Associations between continuous and ordered categorical variables were quantified using the Spearman rank correlation coefficient (r) and Somers’ D statistic, while the Chi squared test was used to ascertain Hardy-Weinberg equilibrium and consistency with previously published genotype frequencies. Progression-free survival was measured from the on-study date to the date of progression or last follow-up. Genotypes and categorical variables were compared using the log-rank test, and hazard ratios were estimated using proportional hazards regression. Exact tests were used as appropriate to calculate P values and 95% confidence intervals (CIs). Large sample CIs of test statistics may be inconsistent with exact P values in cases where exact CI methods are not available in the software employed (SAS/STAT 12.1). The P values reported are not corrected for multiple comparisons.
References
Fuchs, O. Immunomodulatory drugs and their therapeutic effect in hematological malignancies through cereblon. Hematology & Medical Oncology 2, 1–8, https://doi.org/10.15761/HMO.1000129 (2017).
Holstein, S. A. & McCarthy, P. L. Immunomodulatory Drugs in Multiple Myeloma: Mechanisms of Action and Clinical Experience. Drugs 77, 505–520, https://doi.org/10.1007/s40265-017-0689-1 (2017).
Zhu, Y. X. et al. Cereblon expression is required for the antimyeloma activity of lenalidomide and pomalidomide. Blood 118, 4771–4779, https://doi.org/10.1182/blood-2011-05-356063 (2011).
Jakubowiak, A. J. et al. A phase 1/2 study of carfilzomib in combination with lenalidomide and low-dose dexamethasone as a frontline treatment for multiple myeloma. Blood 120, 1801–1809, https://doi.org/10.1182/blood-2012-04-422683 (2012).
Korde, N. et al. Treatment With Carfilzomib-Lenalidomide-Dexamethasone With Lenalidomide Extension in Patients With Smoldering or Newly Diagnosed Multiple Myeloma. JAMA. Oncol 1, 746–754, https://doi.org/10.1001/jamaoncol.2015.2010 (2015).
Stewart, A. K. et al. Carfilzomib, lenalidomide, and dexamethasone for relapsed multiple myeloma. N Engl J Med 372, 142–152, https://doi.org/10.1056/NEJMoa1411321 (2015).
Quach, H. et al. Mechanism of action of immunomodulatory drugs (IMiDS) in multiple myeloma. Leukemia 24, 22–32, https://doi.org/10.1038/leu.2009.236 (2010).
Ito, T. et al. Identification of a primary target of thalidomide teratogenicity. Science 327, 1345–1350, https://doi.org/10.1126/science.1177319 (2010).
Lopez-Girona, A. et al. Cereblon is a direct protein target for immunomodulatory and antiproliferative activities of lenalidomide and pomalidomide. Leukemia 26, 2326–2335, https://doi.org/10.1038/leu.2012.119 (2012).
Chang, X. B. & Stewart, A. K. What is the functional role of the thalidomide binding protein cereblon? Int J Biochem Mol Biol 2, 287–294 (2011).
Fink, E. C. et al. Crbn (I391V) is sufficient to confer in vivo sensitivity to thalidomide and its derivatives in mice. Blood 132, 1535–1544, https://doi.org/10.1182/blood-2018-05-852798 (2018).
Gemechu, Y. et al. Humanized cereblon mice revealed two distinct therapeutic pathways of immunomodulatory drugs. Proc Natl Acad Sci USA 115, 11802–11807, https://doi.org/10.1073/pnas.1814446115 (2018).
Akuffo, A. A. et al. Ligand-mediated protein degradation reveals functional conservation among sequence variants of the CUL4-type E3 ligase substrate receptor cereblon. J Biol Chem 293, 6187–6200, https://doi.org/10.1074/jbc.M117.816868 (2018).
Kazuki, Y. et al. Thalidomide-induced limb abnormalities in a humanized CYP3A mouse model. Sci Rep 6, 21419, https://doi.org/10.1038/srep21419 (2016).
Broyl, A. et al. High cereblon expression is associated with better survival in patients with newly diagnosed multiple myeloma treated with thalidomide maintenance. Blood 121, 624–627, https://doi.org/10.1182/blood-2012-06-438101 (2013).
Jonasova, A. et al. High level of full-length cereblon mRNA in lower risk myelodysplastic syndrome with isolated 5q deletion is implicated in the efficacy of lenalidomide. Eur J Haematol 95, 27–34, https://doi.org/10.1111/ejh.12457 (2015).
Jian, Y. et al. Arsenic trioxide potentiates sensitivity of multiple myeloma cells to lenalidomide by upregulating cereblon expression levels. Oncol Lett 14, 3243–3248, https://doi.org/10.3892/ol.2017.6502 (2017).
Heintel, D. et al. High expression of cereblon (CRBN) is associated with improved clinical response in patients with multiple myeloma treated with lenalidomide and dexamethasone. Br J Haematol 161, 695–700, https://doi.org/10.1111/bjh.12338 (2013).
Franssen, L. E. et al. Cereblon loss and up-regulation of c-Myc are associated with lenalidomide resistance in multiple myeloma patients. Haematologica 103, e368–e371, https://doi.org/10.3324/haematol.2017.186601 (2018).
Schuster, S. R. et al. The clinical significance of cereblon expression in multiple myeloma. Leuk Res 38, 23–28, https://doi.org/10.1016/j.leukres.2013.08.015 (2014).
Gandhi, A. K. et al. Measuring cereblon as a biomarker of response or resistance to lenalidomide and pomalidomide requires use of standardized reagents and understanding of gene complexity. Br J Haematol 164, 233–244, https://doi.org/10.1111/bjh.12622 (2014).
Ren, Y. et al. A Dual Color Immunohistochemistry Assay for Measurement of Cereblon in Multiple Myeloma Patient Samples. Appl Immunohistochem Mol Morphol 24, 695–702, https://doi.org/10.1097/PAI.0000000000000246 (2016).
Chang, X. et al. Mouse Monoclonal Antibodies Generated from Full Length Human Cereblon: Detection of Cereblon Protein in Patients with Multiple Myeloma. Int J Mol Sci 18, https://doi.org/10.3390/ijms18091999 (2017).
Kortum, K. M. et al. Targeted sequencing of refractory myeloma reveals a high incidence of mutations in CRBN and Ras pathway genes. Blood 128, 1226–1233, https://doi.org/10.1182/blood-2016-02-698092 (2016).
Sarah Gooding, C. C. B. et al. 2648 Single Cell Analysis of Acquired Pomalidomide-Resistance in Multiple and Gene Expression Heterogeneity. ASH Annual Meeting (2018).
Butrym, A. et al. Cereblon and IRF4 Variants Affect Risk and Response to Treatment in Multiple Myeloma. Arch Immunol Ther Exp (Warsz) 64, 151–156, https://doi.org/10.1007/s00005-016-0442-6 (2016).
Sardnal, V. et al. A G polymorphism in the CRBN gene acts as a biomarker of response to treatment with lenalidomide in low/int-1 risk MDS without del(5q). Leukemia 27, 1610–1613, https://doi.org/10.1038/leu.2013.59 (2013).
Han, M. et al. A pharmacogenetic analysis of the Canadian Cancer Trials Group MY.10 clinical trial of maintenance therapy for multiple myeloma. Blood 128, 732–735, https://doi.org/10.1182/blood-2016-06-716902 (2016).
Szudy-Szczyrek, A. et al. Polymorphisms in the promoter region of the CRBN gene as a predictive factor for the first-line CTD therapy in multiple myeloma patients. Oncotarget 9, 24054–24068, https://doi.org/10.18632/oncotarget.25307 (2018).
Iskierka-Jazdzewska, E. et al. Cereblon (CRBN) Gene Polymorphisms Predict Clinical Response and Progression-Free Survival in Multiple Myeloma Patients Treated with Lenalidomide: A Pharmacogenetic Study of Immense Consortium. Blood 124, 3628 (2014).
Kazandjian, D. et al. Remission and Progression-Free Survival in Patients With Newly Diagnosed Multiple Myeloma Treated With Carfilzomib, Lenalidomide, and Dexamethasone: Five-Year Follow-up of a Phase 2 Clinical Trial. JAMA Oncol 4, 1781–1783, https://doi.org/10.1001/jamaoncol.2018.5457 (2018).
Mailankody, S. et al. Baseline mutational patterns and sustained MRD negativity in patients with high-risk smoldering myeloma. Blood Adv 1, 1911–1918, https://doi.org/10.1182/bloodadvances.2017005934 (2017).
Stewart, A. K. Novel therapies for relapsed myeloma. Hematology Am Soc Hematol Educ Program, 578–586, https://doi.org/10.1182/asheducation-2009.1.578 (2009).
Butrym, A. et al. Polymorphisms within beta-catenin encoding gene affect multiple myeloma development and treatment. Leuk Res 39, 1462–1466, https://doi.org/10.1016/j.leukres.2015.10.007 (2015).
Dimopoulos, K. et al. Expression of CRBN, IKZF1, and IKZF3 does not predict lenalidomide sensitivity and mutations in the cereblon pathway are infrequent in multiple myeloma. Leuk Lymphoma, 1–9, https://doi.org/10.1080/10428194.2018.1466290 (2018).
Thakurta, A. et al. Absence of mutations in cereblon (CRBN) and DNA damage-binding protein 1 (DDB1) genes and significance for IMiD therapy. Leukemia 28, 1129–1131, https://doi.org/10.1038/leu.2013.315 (2014).
Qian, X. et al. Cereblon gene expression and correlation with clinical outcomes in patients with relapsed/refractory multiple myeloma treated with pomalidomide: an analysis of STRATUS. Leuk Lymphoma, 1–9, https://doi.org/10.1080/10428194.2018.1485915 (2018).
Xiaozhong Qian, M. A. D. et al. Correlative Analyses of Cereblon (CRBN), cMYC, IRF4, BLIMP1, and XBP1 with Clinical Outcomes in Stratus (MM-010), a Phase 3b Study of Pomalidomide (POM) + Low-Dose Dexamethasone (LoDEX) in Patients (pts) with Relapsed/Refractory Multiple Myeloma (RRMM). American Society of Hematology (2017).
Egan, J. B. et al. Extramedullary myeloma whole genome sequencing reveals novel mutations in Cereblon, proteasome subunit G2 and the glucocorticoid receptor in multi drug resistant disease. Br J Haematol 161, 748–751, https://doi.org/10.1111/bjh.12291 (2013).
Sheri Skerget, B. B. et al. A Molecular Analysis of Cereblon-Related Immunomodulatory Drug Resistance in Commpass Multiple Myeloma Patients. American Society of Hematology (2017).
Lode, L. et al. Cereblon expression in multiple myeloma: not ready for prime time. Br J Haematol 163, 282–284, https://doi.org/10.1111/bjh.12478 (2013).
Ruiz-Heredia, Y. et al. Mutational screening of newly diagnosed multiple myeloma patients by deep targeted sequencing. Haematologica. https://doi.org/10.3324/haematol.2018.188839 (2018).
Yamazaki, H. et al. Assessment of Protein Binding of 5-Hydroxythalidomide Bioactivated in Humanized Mice with Human P450 3A-Chromosome or Hepatocytes by Two-Dimensional Electrophoresis/Accelerator Mass Spectrometry. Chem Res Toxicol 29, 1279–1281, https://doi.org/10.1021/acs.chemrestox.6b00210 (2016).
Millrine, D., Tei, M., Gemechu, Y. & Kishimoto, T. Rabex-5 is a lenalidomide target molecule that negatively regulates TLR-induced type 1 IFN production. Proc Natl Acad Sci USA 113, 10625–10630, https://doi.org/10.1073/pnas.1611751113 (2016).
Matyskiela, M. E. et al. SALL4 mediates teratogenicity as a thalidomide-dependent cereblon substrate. Nat Chem Biol 14, 981–987, https://doi.org/10.1038/s41589-018-0129-x (2018).
Sissung, T. M. et al. Carfilzomib and lenalidomide response related to VEGF and VEGFR2 germline polymorphisms. Cancer Chemother Pharmacol 80, 217–221, https://doi.org/10.1007/s00280-017-3323-8 (2017).
Korde, N. et al. Treatment With Carfilzomib-Lenalidomide-Dexamethasone With Lenalidomide Extension in Patients With Smoldering or Newly Diagnosed Multiple Myeloma. JAMA Oncol, https://doi.org/10.1001/jamaoncol.2015.2010 (2015).
Acknowledgements
The authors would like to thank Dr. Douglas Price for his helpful comments and suggestions. This work was supported by the Intramural Research Program of the Center for Cancer Research, National Cancer Institute, National Institutes of Health. Drs. Landgren, Korde, and Mailankody thank Memorial Sloan Kettering Cancer Center NCI Core Grant (P30 CA 008748) for funding support. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organization imply endorsement by the U.S. Government.
Author information
Authors and Affiliations
Contributions
C.H.C. and W.D.F. designed the research. P.A.H., S.L.B. and S.G. performed research. P.A.H., D.J.V. and C.H.C. analyzed data. D.K., N.K., S.M. and O.L. provided clinical trial data. P.A.H., S.L.B. and C.H.C. wrote the paper. All authors revised and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
O.L. receives grant support from NIH, FDA, MMRF, IMF, LLS, Perelman Family Foundation, Rising Tides Foundation, Amgen, Celgene, Janssen, Takeda, Glenmark, Seattle Genetics, and Karyopharm. He is a member of the following Honoraria/Advisory Boards: Adaptive, Amgen, Binding Site, BMS, Celgene, Cellectis, Glenmark, Janssen, Juno, and Pfizer. He also serves as Chairman for “Medscape Myeloma” (2014-ongoing) and is a member of the Independent Data Monitoring Committee (IDMC) for Takeda, Merck, Janssen, and Theradex. All other authors declare no potential conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, P.A., Beedie, S.L., Chau, C.H. et al. Cereblon gene variants and clinical outcome in multiple myeloma patients treated with lenalidomide. Sci Rep 9, 14884 (2019). https://doi.org/10.1038/s41598-019-51446-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-51446-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.