Abstract
Microsatellite Instability (MSI) is a hallmark of colorectal cancer (CRC) and occurs in 15–16% of CRC. Molecular biological information of CRC in South Africa (SA) is largely unrecorded. This study was undertaken to determine the frequency of MSI, with particular reference to Lynch syndrome (LS) with a view to improve surveillance and prevention strategies. This was a retrospective study on CRC samples diagnosed between 2011–2015 at Charlotte Maxeke Johannesburg Academic Hospital (CMJAH). Samples diagnosed between 2011–2012 were screened for MSI by PCR and mismatch repair (MMR) immunohistochemistry (IHC), and additional BRAFV600E mutational analysis performed. T-tests, Fischer’s exact and Chi square statistical tests were applied. Twelve percent of patients displayed MSI, with increased frequency in black (15%) versus other ethnic group (OEG) (8%) patients. MSI patients were significantly younger than microsatellite stable (MSS) patients, however when stratified by ethnicity, black patients were predominantly younger (median age: 47), with increased MSH2/6 loss, and no BRAF mutations. These findings suggest a large proportion of young black SA CRC patients develop via the LS pathway due to earlier age onset and predominant MSH2/6 protein loss. SA patients of other ethnicities appear to follow the more well established sporadic MSI pathway.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) develops through three major molecular pathways namely: Chromosomal Instability (CIN), Microsatellite Instability (MSI), and the epigenetic instability or CpG island methylator phenotype (CIMP) pathway1,2,3. CIN or microsatellite stable (MSS) tumours account for 65–75% of CRC and mainly develop through mutant adenomatous polyposis coli (APC) gene with subsequent KRAS mutational activation, TP53 inactivation and somatic copy number alterations (SCNAs)4,5. MSI CRC occurs in approximately 15–16% of CRC due to inactivation of the DNA Mismatch Repair (MMR) system (MLH1, MSH2, MSH6, PMS2), with the majority (12%) presenting as sporadic MSI CRC as a result of epigenetic mutation (methylation silencing) of the promoter sequence of MLH1, and BRAF V600E oncogenic mutations2,6,7,8,9,10. The remaining subset (2–3%) is caused by germline mutations in either one of 4 MMR genes or the EpCAM gene and is a feature of Lynch syndrome (LS)8,9,11,12,13,14. CIMP CRC (10–20%) demonstrate hypermethylation of several promoter CpG island loci throughout the genome, leading to tumour suppressor and tumour-related gene inactivation. The CIMP and the MSI pathway overlaps in sporadic MSI CRCs, as these tumours display high levels of CIMP and MSI and are characterized by a different type of precursor lesion in comparison to LS15,16. LS follows the classic adenoma-carcinoma sequence pathway as they present mainly with tubular adenomas (TAs) or tubulovillous adenomas (TVAs), whereas sporadic MSI CRCpremalignant lesions are sessile serrated adenomas (SSAs) developing through the serrated neoplasia pathway15,16,17. Clinicopathological features of sporadic MSI CRC include predominant occurrence in female patients, within the right colon and associated morphology includes signet ring cell and mucinous features with tumour infiltrating lymphocytes (TIL)15,18,19,20. LS patients are mainly associated with younger patients, with no gender preference and similar morphology as sporadic MSI tumours12.
Previous CRC studies conducted in SA showed a higher frequency of MSI CRC in young black patients through MMR deficiency than white patients21,22,23. These studies suggested a high frequency of LS, however additional validation studies and further molecular characterization of MSI CRC in black SA patients was recommended24.
MSI assessment has also shown important prognostic and predictive roles in CRC patient care, as MSI tumours are associated with a better prognosis than MSS tumours in early stage CRC, and treatment of MSI stage II tumours are not well responsive to 5-fluorouracil (5-FU) (standard treatment)25,26. MSI/BRAF wild-type tumours are also more suggestive of LS and is crucial for improving cancer surveillance and prevention screening for patient family members, due to their increased risk of developing cancer. Identifying LS patients and treating with aspirin (600 mg per day) have also shown to reduce the risk of CRC27.
This study assesses the frequency and features associated with MSI CRC over a 5-year period in a cohort of newly diagnosed CRC patients at the Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) within SA. This data will provide insight into the CRC histopathological and molecular features associated with MSI CRC in black SA patients, with particular reference to MSI CRC frequency and the occurrence of suspected LS, a heretofore largely unassessed aspect of the disease.
Methodology
Patient demographics and tumour pathological characterisation
This was a retrospective study, comprising a 5-year cohort of 675 patients who had biopsy samples or colorectal resections fulfilling the histological criteria for adenocarcinoma of the colon or rectum from January 2011–December 2015, reported by the Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) branch of the National Health Laboratory Service (NHLS)/Anatomical Pathology Division, Faculty of Health Sciences, University of the Witwatersrand. A total of 439 CRC cases with an MSI status by MMR immunohistochemistry (IHC) or MSI PCR result were included in this study. All cases were stratified by age, gender, ethnicity, tumour site, histological subtype, grade, stage (TNM classification by AJCC staging), presence and grade of precursor lesion, presence of tumour infiltrating lymphocytes (TIL) and Crohn’s-like inflammatory reaction (CIR). Tumour site was considered left-sided if distal from the splenic flexure and right-sided if proximal to the splenic flexure. This information was obtained from histology reports. A semi-quantitive H&E assessment using the Klintrup-Mäkinen score was used to determine the presence of TILs28. Immunophenotypic profiling of TILs was not performed. Family histories were not available from the histological reports. This research was conducted under the institution’s blanket ethics clearance (M10744) which allows for research to be carried out on all archived pathology specimens without informed consent from study participants. Additional study-specific ethics clearance was also obtained by the Ethics Committee of the University of the Witwatersrand (clearance number M120994), and all tests were performed according to the relevant guidelines and regulations.
Molecular characterisation
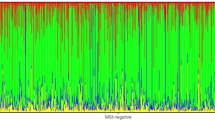
Molecular characterization of patient samples for frequency assessment was limited to the first 2 years (2011–2012) mainly due to the availability of funds (Figure 1). A total of 275 CRC cases were diagnosed during this period and a cohort of 267 archival CRC tumour specimens was retrieved, examined and subjected to molecular analysis. MSI PCR was conducted and samples with a MSI-High profile had additional BRAF V600E mutational analysis performed.
Cases without MMR IHC results as ascertained from the histology reports were screened for MMR protein loss by IHC.
DNA was extracted from 4 × 10µm sections of tumour tissue from formalin fixed paraffin embedded (FFPE) blocks using the QIAamp DNA FFPE tissue kit (Qiagen, Valencia, CA USA). The extracted DNA was subjected to a pentaplex PCR panel of 5 markers comprising mononucleotide repeats amplified by 5 sets of primers, i.e. (BAT-25, BAT-26, NR-21, NR-24, and NR-27) as described in Haghighi et al.29. Each antisense primer was labeled with 1 of the fluorescent markers FAM, HEX, or NED. The Applied Biosystems® True Allele® PCR master mix was used according to manufacturer’s instructions with slight modifications for successful amplification of the multiplex PCR. Fluorescent PCR products were subjected to capillary electrophoresis on the Applied Biosystems PRISM 3500 automated genetic analyzer, and allelic size was determined using Genemapper 4.0 software (Applied Biosystems). Samples with no allelic size variations in the 5 microsatellite markers were classified as microsatellite stable (MSS), allelic size variations found in 1 of the 5 microsatellites markers were classified as microsatellite instability-low (MSI-L) and variation in 2 or more microsatellite markers was classified as microsatellite instability-high (MSI-H)29. Previous studies have indicated black people show polymorphic variation frequencies within alleles NR21, BAT25 and BAT26 of approximately 10%30,31,32. For tumour samples that demonstrated instability in only 2 of these 3 markers, matched normal tissue was assessed to determine the instability status. In cases where no normal tissue could be assessed, samples were regarded as MSS.
MMR IHC was performed on MSI-H samples that were not previously assessed, utilizing the Dako EnVision™ FLEX detection system Kit and Autostainer Link 48 equipment (Dako, Glostrup, Denmark) according to manufacturer’s instructions. The primary monoclonal antibodies used were FLEX monoclonal mouse antibodies against MLH1 (clone ES05, ref ISO79, ready-to-use), MSH2 (clone FE11, ref IRO85, ready-to-use), MSH6 (clone EP49, ref IRO86, ready-to-use) and PMS2 (clone EP51, IRO87, ready-to-use) (Dako, Glostrup, Denmark). These were applied to 4-μm deparaffinized formalin fixed paraffin-embedded (FFPE) tissue sections. Blockage of endogenous peroxide activity was carried out with the EnVision™ FLEX Peroxidase-Blocking Reagent (Dako, Glostrup, Denmark) and Antigen retrieval performed at 97 °C for 20 minutes (pH 9.0). Antigen-antibody reaction was visualized with the DAB (Diaminobenzidine) solution, and subsequently counter-stained with hematoxylin. Each sample was screened by an expert pathologist for the absence or presence of expression of each of the 4 MMR proteins. Negative protein expression was defined as complete absence of nuclear staining within tumor cells. Expression of MMR proteins in normal epithelium, lymphocytes and stromal cells was used as positive internal controls for each case. The four deficient (d) MMR patterns assessed were 1: dMLH1/PMS2; 2: dMSH2/MSH6; 3: dMSH6 and 4: dPMS2.
All MSI-H samples were assessed for BRAF V600E mutations using the real-time Therascreen RGQ BRAF V600E mutation kit (Qiagen, Whitehead Scientific WHS), according to the manufacturer’s instructions. The kit uses ARMS® and Scorpions® technology, and includes a control assay to evaluate the adequacy of quality and quantity of DNA in a sample, before assessing the presence or absence of mutated DNA. Results were only deemed valid if the control run passed.
Data obtained from the molecular characterization study (2011–2012) led to a more comprehensive study which included cases with an MSI status from histological reports for the total 5-year study period (2011–2015).
Statistical analysis
All clinical data was collected in an excel sheet and statistical analysis was performed using Stata Intercooled 7.0 (Stata, College Station, TX, USA) and Graphpad Prism version 7 (GraphPad Software, La Jolla, CA, USA). MSS and MSI-L cases were grouped together into one group (MSS), to establish unique associations with the counterpart MSI-H group. Patients were also analysed on the basis of ethnicity: black (African) versus other ethnic groups i.e., white (Caucasian), coloured (Mixed Ancestry), Indian (Asian); age and gender. The ability to draw statistically significant results on all ethnic groups was not possible due to small case numbers of certain groups. For this reason, White, Indian and Coloured patients were grouped into one “Other Ethnic Group” (OEG) to allow comparison with their black counterpart. Histopathological features were assessed as stated in the methodology section, and associations were evaluated using Fischer’s exact and Chi-square tests. A result with a P value less than 0.05 was considered statistically significant.
Results
Patient demographics
A total 439 of 672 CRC patients diagnosed between January 2011-December 2015 had MSI CRC status assessment. Of these cases, 247 (56%) were male and 192 (44%) female, with an overall median age of 58 years. Black patients contributed to 60% (262/439) of cases. (Column1 of Table 1).
Pathological characteristics
Further descriptive analysis was done with respect to histological characteristics, with left sided tumours accounting for the majority of cases (63%; 273/430) (Column1 of Table 1). The most common subtype was invasive adenocarcinoma (384/430; 89%), followed by invasive mucinous adenocarcinoma (30/430; 7%). AJCC tumour stage II and III accounted for the majority of cases (259/287; 90%) (Table 1). Further stratification by MSI and MSS subtype is illustrated in the 2nd and 3rd column in Table 1.
MSI CRC molecular characterization (2011–2012)
MSI PCR performed on 267 cases (2011–2012) illustrated the majority were MSS (191/267; 71%), followed by MSI-L (45/267; 17%) and MSI-H (31/267; 12%). MMR IHC results demonstrated dMLH1 in most MSI CRC cases (13/31; 42%), followed by dMSH2/6 (10/31; 32%), dPMS2 (2/31; 6%) and dMSH6 (1/31; 3%). BRAF mutational analysis was performed on all MSI-H cases with only 10% (3/31) harbouring a mutation, and all 3 (3/13; 23%) occurred in dMLH1 tumours (See Fig. 1).
Flow diagram illustrating the molecular methodology and frequency results of CRC cases diagnosed between 2011–2012. MSI CRC was found in 12% of CRC cases, with predominant MLH1 loss, however only 23% of deficient MLH1 cases harboured BRAFV600E mutations. These findings suggest a large proportion of SA MSI CRC patients could develop through a hereditary pathway.
MSI versus MSS CRC subtyping (2011–2015)
Male patients comprised 56% of the entire CRC cohort. Correlation between subtype and age was found (P = 0.0033) as median age was significantly lower in MSI CRC compared to the MSS subtype (51 vs 59 years respectively) (Table 1). A higher frequency of MSI tumours was seen in blacks ([22/148; 15%] versus OEG patients [9/119; 8%]), for the period 2011–2012. A significant relationship was seen between CRC subtype and tumour site (P < 0.0001), as MSS was associated with left sided tumours (261/370; 70%) and MSI with the right sided tumours [(47/60; 78%). A link between CRC molecular subtype and tumour subtype was also found (P < 0.0001), as mucinous adenocarcinoma occurred at a more frequent rate in MSI CRC; (13/60; 22%) than MSS CRC (17/370; 5%). Tumour infiltrating lymphocytes (TIL) response and subtype was found to have a correlation (P = 0.0045) as this occurred more often in the MSI group (26/47; 55%) than the MSS (77/236; 33%). Polyp subtypes tubular adenoma (TA) and tubulovillous adenoma (TVA) were associated with molecular subtypes (P = 0.0216) as TAs occurred more frequently in MSS CRC (49/84; 58%) and TVAs in MSI CRC (11/17; 65%).
Within the MSI CRC subgroup, additional association evaluations between ethnicity, gender, tumour site, defective MMR proteins and BRAFV600E mutation status were performed (Table 2). A correlation with age was shown (P = 0.0006) as black patients were significantly younger compared to OEG patients (median age: 47 versus 62, respectively). Tumour site and ethnicity showed an association for 2011–2012 data (P = 0.0105), as the majority of tumours were right sided within OEG patients (8/9; 89%), whereas black patients had left (8/22; 36%) and right-sided tumours (13/22; 59%) (Supplementary Data Table 2). Data for 2011–2015 however showed no such association (P = 0.1817). An association between ethnic groups and dMMR protein expression was found (P = 0.0098), where dMLH1/PMS2 expression was more commonly seen in OEG patients (15/22; 68%), and dMSH2/6 in black patients (19/39; 49%). BRAF V600E mutation status and ethnicity were related in the 2011–2012 data (P = 0.0187) (Supplementary Data Table 2), as all black patients were wild-type for BRAF gene status, however within the OEG, BRAF mutations were only found in dMLH1 tumours (3/5; 60%). For the 2011–2015 BRAFV600E data analysis, 2011–2012 results were dominantly represented with an additional 3 cases from 2013–2015 reports with BRAFV600E status. An increased association between BRAFV600E and OEG patients was shown (P = 0.0045) for this period.
Table 3 illustrates a multivariate analysis including variables considered clinically significant for MSI status. Total number of observations were 277. Age, tumour site, mucinous adenocarcinomas and TILS associated after controlling for confounding factors. Patients >50 years were 67% less likely to have MSI and right sided tumours were 8X more likely to have MSI. Invasive adenocarcinomas were 73% less likely to show MSI than mucinous adenocarcinomas. Absence of a TIL response was 60% most likely not to have MSI in comparison to those with TILs. TVAs were not included due to the small sample size, reducing the power and value of the analysis.
Discussion
MSI CRC was detected in 12% of CRC patients diagnosed during the period 2011–2012, however when stratified by ethnic groups, a higher frequency was found in black versus OEG patients although only of borderline significance (15% versus 8% respectively; P = 0.0831). Black patients with MSI tumours occurred in younger patients with left- (36%) and right-sided (59%) tumours, associated with dMSH2/6 (45%), and dMLH1/PMS2 (36%) tumours with a lack of BRAF mutations, indicating a possible LS cause10,33,34,35. MSI CRC in Western population groups are shown to dominantly occur in female patients with right-sided tumours, a serrated morphology and BRAFV600E mutations, MLH1 protein loss due to promoter methylation and a high CIMP molecular phenotype2,20.
In the SA cohort, MSI CRC was associated with younger age, right sided tumours, mucinous adenocarcinomas, TIL response, and TVA precursor lesions. This correlates well with findings in the literature36,37. Histopathological features were further stratified by ethnic groups (black versus OEG) to assess if any associations occurred with regard to gender, age, tumour site, MMR protein expression profile and BRAF mutation status. Within the 2011–2012 cohort, patients within the OEG were predominantly older (median age: 62), female (67%), possessed right sided tumours (89%), with deficient MLH1 (56%) expression, of which 60% harboured BRAF mutations. The 2011–2015 cohort however demonstrated an equal ratio of male to female patients, which could signify an under-diagnosis of female patients with MSI within the OEG. All other variables illustrated increased statistical associations within the 5-year cohort study. Collectively these features suggest the majority of OEG patients follow the more well established sporadic MSI CRC pathway19,20. Within the black patient group, all 2011–2012 data analysed with statistical significant associations revealed increased significance within the 5 year cohort, with the exception of tumour site where 2011–2012 data illustrated significance with an increased incidence of left-sided MSI tumours. This could possibly be due to pathologists generally screening more right than left-sided tumours for MSI CRC.
MSI CRC also showed a high percentage of proficient (p) MMR expression (16%) for the universal 2-year screen, despite high concordance rates (95–96%) for MSI PCR versus IHC reported38. This could possibly be indicative of aberrant non-functional proteins expressed or an alternative MMR protein involved in the development of MSI in this group of patients. This would suggest the 5 mononucleotide panel for MSI testing is the more sensitive tool for detecting instability in the South African setting. Perhaps this could be explored further for alternative causes of dMMR in these patients. For example, MSH3 loss of expression has recently been shown to be associated with MSI in African American patients39,40.
Multiple logistic regression analysis was also conducted to control for the effect of confounding factors, young age (≤50 years), right-sided tumours, mucinous adenocarcinomas and TILS were associated with MSI CRC in SA patients.
Limitations of the study included patient selection bias as patients from the 2013–2015 cohort were only selected if an MSI status was available. In addition, only a few patient samples with available data in certain subgroup analysis, such as TNM stage of disease, TILs, polyp subtype could be analysed, and this is mainly due to biopsy samples also included in the cohort. Only a subset of MSI samples (34/61; 56%) for the period 2011–2015 were included for BRAFV600E analysis, these largely from cases between period 2011–2012. This also represents a limitation of the study. The majority of patients diagnosed at CMJAH are of the black population group, therefore selection bias could play a role in the selection effect due to smaller sample numbers in the comparator OEG patient group. Previous MSI studies in SA however, have largely shown MLH1 mutations as the cause of hereditary and sporadic CRC in OEG patients (specifically the coloured and white population groups in the Western and Northern Cape regions of SA)23,41,42. A study carried out by Cronje et al. in 2009 at CMJAH in Johannesburg demonstrated a large number of young black patients had increased loss of MMR protein expression, particularly MSH2, in comparison to their white counterpart, also suggesting a heritable cause21. Findings from this study confirm dMLH1 and dMSH2 associations within young OEG and black SA patients respectively.
South Africa is comprised of 9 provinces, with an estimated mid-year population of 58.78 million. The Northern Cape comprises 2.2% of the population, Western Cape 11.5%, and Gauteng 25.8%43,44. The Western and Northern Cape comprises mainly of the coloured population within SA, and LS have largely been identified in these 2 provinces (See Fig. 2)23,41,45. Genetic services are offered to newly diagnosed LS patients and family members in these regions mainly through academic centres based in the Western Cape, and to smaller surrounding towns and rural areas through outreach programmes23,41,45,46.
Map of South Africa illustrating the distribution of population groups by the different provinces, (adapted from the Wikipedia map of South Africa 2011)54.
The Gauteng province, although the smallest, is the most densely populated and urbanized with nearly 700 people per square kilometre43,44. This is largely due to the discovery of gold in Johannesburg during the 1800’s, with a large influx of migrants from Africa and Europe46. The black population is the predominant group (77.4%) followed by white (15.6%) in this region43,44. LS genetic screening in Gauteng and remaining 6 provinces have been poor to non-existent, even though preliminary findings have suggested a possible hereditary cause, particularly in black patients from the 1990’s21,47,48,49.
The healthcare financial system in SA is based on private and public funding, with the majority (57%) of the population utilizing public healthcare services, however 80% of healthcare expenditure in SA occurs in the private sector46,50. Genetic services such as testing and counselling are mostly offered in academic centres, and subsidies for these services are limited primarily due to the high medical costs associated with the HIV/AIDS epidemic46. Pathologists within the National Health Laboratory Services include a possible hereditary cause in histopathological reports of these patients with suspected LS, but genetic services are limited to counselling, particularly within the public sector of the Gauteng province. Colonoscopic surveillance of family members at risk for LS is difficult and expensive in a resource-poor country, however previous LS studies carried out within the Western Cape region of SA have shown the identification of the causative-mutation simplifies and reduces costs of surveillance considerably22,45,51.
If LS is the more prevalent MSI subtype in black SA patients, identifying the causative mutation together with regular colonoscopy screening is recommended for all affected individuals and families by the 2nd decade of life, to be repeated every 1–2 years52. LS patients treated with aspirin have a considerably reduced risk and reduced mortality rates associated with CRC27,53.
Conclusion
This study revealed MSI in black SA CRC patients is associated with earlier age onset, higher frequency of MSH2/6 loss and a lack of BRAFV600E mutations, suggesting Lynch or “Lynch-Like Syndrome” (LLS) as the main hereditary driver. Implementation of universal MSI screening is recommended as a routine diagnostic test within the SA setting to increase the detection rate of LS or LLS. This data warrants further molecular investigations in defining the underlying germline or somatic mutations. Appropriate early detection, surveillance and prevention strategies will reduce the risk and improve overall management of the disease in suspected LS patients and affected family members, particularly in the black population group in SA.
Compliance with ethical standards
This was a retrospective study on already available biological material and ethics clearance was obtained from the Human Ethics Research Committee, Faculty of Health Sciences: Ethics clearance reference number: M120994.
Data availability
The dataset generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
TCGA. Comprehensive molecular characterization of human colon and rectal cancer. Nature 487, 330–337 (2012).
Muller, M., Ibrahim, A. & Arends, M. Molecular pathological classification of colorectal cancer. Virchows Arch. 469, 125–134 (2016).
Mojarad, E. N., Kuppen, P. J. K., Aghdaei, H. A. & Zali, M. R. The CpG island methylator phenotype (CIMP) in colorectal cancer. Gastroenterol. Hepatol. from Bed to Bench 6, 120–128 (2013).
Muller, A. & Ibrahim, M. A. New molecular classification of colorectal cancer. Cancer Chemother. Rev. 11, 66–72 (2016).
Tariq, K., Ghias, K., Tariq, K. & Ghias, K. Colorectal cancer carcinogenesis: a review of mechanisms. Cancer Biol. Med. 13, 120–35 (2016).
Wang, L. et al. BRAF mutations in colon cancer are not likely attributable to defective DNA mismatch repair. Cancer Res. 63, 5209–5212 (2003).
Toyota, M. et al. CpG island methylator phenotype in colorectal cancer. Proc. Natl. Acad. Sci. USA 96, 8681–8686 (1999).
Kawakami, H., Zaanan, A. & Sinicrope, A. MSI testing and its role in the management of colorectal cancer. Curr. Treat. Options Oncol. 16, 1–12 (2015).
Adar, T. et al. A tailored approach to BRAF and MLH1 methylation testing in a universal screening program for Lynch syndrome. Mod. Pathol. 30, 440–447 (2017).
Weisenberger, D. et al. CpG Island Methylator Phenotype in Human Colorectal Cancer Is Tightly Associated with BRAF Mutation and Underlies Sporadic Mismatch Repair Deficiency. Nat. Genet. 38, 787–793 (2006).
Lynch, P. M., Lynch, H. T. & Harris, R. E. Hereditary proximal colonic cancer. Dis. Colon Rectum 20, 661–668 (1977).
Lynch, H. et al. Review of the Lynch syndrome: history, molecular genetics, screening, differential diagnosis, and medicolegal ramifications. Clin. Genet 76, 1–18 (2009).
Boland, C. & Goel, A. Microsatellite Instability in Colorectal Cancer. J. Gastroenterol. 138, 2073–2087 (2010).
Liccardo, R., De Rosa, M., Izzo, P. & Duraturo, F. Novel implications in molecular diagnosis of lynch syndrome. Gastroenterol. Res. Pract. 2017, 1–12 (2017).
Okamoto, K. et al. Clinicopathological characteristics of serrated polyps as precursors to colorectal cancer: Current status and management. J. Gastroenterol. Hepatol. 32, 358–367 (2017).
Jass, R. HNPCC and sporadic MSI-H colorectal cancer: a review of the morphological similarities and differences. 3, 93–100 (2004).
Walsh, M. D. et al. Immunohistochemical testing of conventional adenomas for loss of expression of mismatch repair proteins in Lynch syndrome mutation carriers: A case series from the Australasian site of the colon cancer family registry. Mod. Pathol. 25, 722–730 (2012).
Boland, C. R. et al. A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res. 58, 5248–5257 (1998).
Sinicrope, F. A. & Yang, Z. J. Prognostic and predictive impact of DNA mismatch repair in the management of colorectal cancer. Futur. Oncol. 7, 467–474 (2011).
Inamura, K. Colorectal cancers: An update on their molecular pathology. Cancers (Basel). 10, 1–18 (2018).
Cronjé, L., Paterson, A. C. & Becker, P. J. Colorectal cancer in South Africa: A heritable cause suspected in many young black patients. South African Med. J. 99, 103–106 (2009).
Stupart, D. A., Goldberg, P. A., Algar, U. & Ramesar, R. Surveillance colonoscopy improves survival in a cohort of subjects with a single mismatch repair gene mutation. Color. Dis. 11, 126–130 (2009).
Vergouwe, F. et al. Mismatch repair deficiency in colorectal cancer patients in a low-incidence area. South African J. Surg. 51, 16–21 (2013).
Katsidzira, L. et al. The shifting epidemiology of colorectal cancer in sub-Saharan Africa. Lancet. Gastroenterol. Hepatol. 2, 377–383 (2017).
Boland, P. M., Yurgelun, M. B. & Boland, C. R. Recent progress in Lynch syndrome and other familial colorectal cancer syndromes. CA. Cancer J. Clin. 68, 217–231 (2018).
Sargent, D. J. et al. Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer. J. Clin. Oncol. 28, 3219–3226 (2010).
Burn, J. et al. Long-term effect of aspirin on cancer risk in carriers of hereditary colorectal cancer: An analysis from the CAPP2 randomised controlled trial. Lancet 378, 2081–2087 (2011).
Hendry, S. et al. Assessing Tumor-Infiltrating Lymphocytes in Solid Tumors: A Practical Review for Pathologists and Proposal for a Standardized Method from the International Immuno-Oncology Biomarkers Working Group: Part 2: TILs in Melanoma, Gastrointestinal Tract Carcinom. Adv. Anat. Pathol. 24, 311–335 (2017).
Haghighi, M. M. et al. Frequent MSI mononucleotide markers for diagnosis of hereditary nonpolyposis colorectal cancer. Asian Pac. J. Cancer Prev. 11, 1033–1035 (2010).
Pyatt, R. et al. Implications for Microsatellite Instability Testing. Cancer Res. 155, 349–353 (1999).
Suraweera, N. et al. Evaluation of tumor microsatellite instability using five quasimonomorphic mononucleotide repeats and pentaplex PCR. Gastroenterology 123, 1804–1811 (2002).
Buhard, O. et al. Multipopulation Analysis of Polymorphisms in Five Mononucleotide Repeats Used to Determine the Microsatellite Instability Status of Human Tumors. J. Clin. Oncol. 24, 241–251 (2005).
Umar, A. et al. Revised Bethesda Guidelines for Hereditary Nonpolyposis Colorectal Cancer (Lynch Syndrome) and Microsatellite Instability. 96, 261–268 (2004).
Lynch, H. & de la Chapelle, A. Hereditary Colorectal Cancer. 348, 919–932 (2003).
Lagerstedt Robinson, K. et al. Lynch syndrome (hereditary nonpolyposis colorectal cancer) diagnostics. J. Natl. Cancer Inst. 99, 291–299 (2007).
Alexander, J. et al. Histopathological identification of colon cancer with microsatellite instability. Am. J. Pathol. 158, 527–535 (2001).
Kim, H., Jen, J., Vogelstein, B. & Hamilton, S. R. Clinical and pathological characteristics of sporadic colorectal carcinomas with DNA replication errors in microsatellite sequences. Am J Pathol 145, 148–156 (1994).
Cicek, M. S. et al. Quality assessment and correlation of microsatellite instability and immunohistochemical markers among population- And clinic-based colorectal tumors: Results from the colon cancer family registry. J. Mol. Diagnostics 13, 271–281 (2011).
Ashktorab, H. et al. Driver genes exome sequencing reveals distinct variants in African Americans with colorectal neoplasia. Oncotarget 10, 2607–2624 (2019).
Venderbosch, S. et al. EMAST is associated with a poor prognosis in microsatellite instable metastatic colorectal cancer. PLoS One 10, 1–13 (2015).
Wentik, M. Q., Rakers, M., Stupart, D. A., Ramesar, R. & Goldberg, P. A. Incidence and histological features of colorectal cancer in the Northern Cape province, South Africa. South African J. Surg. 48, 109–113 (2010).
Hitchins, M. et al. Identification of new cases of early-onset colorectal cancer with an MLH1 epimutation in an ethnically diverse South African cohort. Clin. Genet. 80, 428–434 (2011).
Census. Statistics South Africa. Census Stat. South Africa 78 (2011), P0301.4 (2011).
Statistics South Africa. Mid-year population estimates. Mid-year Popul. Estim. 2019 (Report). 29 July 2019 Retrieved 29 July 2019 (2019).
Bruwer, Z., Futter, M. & Ramesar, R. A mobile colonoscopic unit for lynch syndrome: Trends in surveillance uptake and patient experiences of screening in a developing country. J. Genet. Couns. 22, 125–137 (2013).
Kromberg, J. G., Sizer, E. B. & Christianson, A. L. Genetic services and testing in South Africa. J. Community Genet. 4, 413–423 (2013).
Degiannis, E., Sliwa, K., Levy, R., Hale, M. J. & Saadia, R. Clinicopathological trends in colorectal carcinoma in a Black South African population. Trop. Gastroenterol. 16, 55–61 (1995).
Skalsky, J. A. Colorectal cancer in young black patients. Trop. Doct. 19, 185 (1989).
Bebington, B. An evaluation of epidemiological differences in colorectal cancer patients over and under the age of 50 presenting to academic centers in Johannesburg. S Afr J Surg 55, 54 (2017).
Econex. Estimating the Financial Cost of the NHI Plan. Heal. (San Fr. 9, 24–30 (2010).
Goldberg, P. A. et al. In a Resource-Poor Country, Mutation Identification has the Potential to Reduce the Cost of Family Management for Hereditary Nonpolyposis Colorectal Cancer. Dis. Colon Rectum 41, 1250–1255 (1998).
Lynch, H. T., Lynch, J. F. & Attard, T. A. Diagnosis and management of hereditary colorectal cancer syndromes: Lynch syndrome as a model. Cmaj 181, 273–280 (2009).
Chan, A. T. et al. Aspirin in the chemoprevention of colorectal neoplasia: An overview. Cancer Prev. Res. 5, 164–178 (2012).
Wikipedia Map of South Africa by dominant population groups. Available at: https://en.wikipedia.org/wiki/Demographics_of_South_Africa#/media/File:South_Africa_2011_dominant_population_group_map.svg, (Accessed: 30th July 2019) (2011).
Acknowledgements
Griffin Trust Fund (GTCP016). National Health Laboratory Services Trust Fund (94347). Wits University FRC Fund (001.251.8462101.5121105.000000.0000000000.4550). Dr. Innocent Maposa (Biostatistician) for statistical analysis contribution. Alain Lobandji and Nzeba Madi for assisting with the immunohistochemistry methodology.
Author information
Authors and Affiliations
Contributions
M.M., Y.P. and C.P. were involved in the design and research methodology of the study. M.M. performed the analysis and wrote the manuscript. R.M. and P.M. contributed to data analysis. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
McCabe, M., Perner, Y., Magobo, R. et al. Microsatellite Instability assessment in Black South African Colorectal Cancer patients reveal an increased incidence of suspected Lynch syndrome. Sci Rep 9, 15019 (2019). https://doi.org/10.1038/s41598-019-51316-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-51316-4
This article is cited by
-
Racial disparities in colorectal cancer clinicopathological and molecular tumor characteristics: a systematic review
Cancer Causes & Control (2024)
-
Left-sided colorectal cancer distinct in indigenous African patients compared to other ethnic groups in South Africa
BMC Cancer (2022)
-
Evaluating utility and feasibility of mismatch repair testing of colorectal cancer patients in a low-middle-income country
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.