Abstract
The anti-angiogenic agent, diamino propane tetraiodothyroacetic acid (DAT), is a thyro-integrin (integrin αvβ3) antagonist anticancer agent that works via genetic and nongenetic actions. Tetraiodothyroacetic acid (tetrac) and DAT as thyroid hormone derivatives influence gene expression after they transport across cellular membranes. To restrict the action of DAT to the integrin αvβ3 receptors on the cell surface, we used DAT-conjugated PLGA nanoparticles (NDAT) in an active targeting mode to bind to these receptors. Preparation and characterization of NDAT is described, and both in vitro and in vivo experiments were done to compare DAT to NDAT. Intracellular uptake and distribution of DAT and NDAT in U87 glioblastoma cells were evaluated using confocal microscopy and showed that DAT reached the nucleus, but NDAT was restricted from the nucleus. Pharmacokinetic studies using LC-MS/MS analysis in male C57BL/6 mice showed that administration of NDAT improved the area under the drug concentration curve AUC(0–48 h) by 4-fold at a dose of 3 mg/kg when compared with DAT, and Cmax of NDAT (4363 ng/mL) was 8-fold greater than that of DAT (548 ng/mL). Biodistribution studies in the mice showed that the concentrations of NDAT were higher than DAT/Cremophor EL micelles in heart, lung, liver, spleen, and kidney. In another mouse model using female NCr nude homozygous mice with U87 xenografts, tumor growth was significantly decreased at doses of 1 and 3 mg/kg of NDAT. In the chick chorioallantoic membrane (CAM) assay used to measure angiogenesis, DAT (500 ng/CAM) resulted in 48% inhibition of angiogenesis levels. In comparison, NDAT at low dose (50 ng/CAM) showed 45% inhibition of angiogenesis levels. Our investigation of NDAT bridges the study of polymeric nanoparticles and anti-angiogenic agents and offers new insight for the rational design of anti-angiogenic agents.
Similar content being viewed by others
Introduction
Angiogenesis, the development of new blood vessels, is crucial for tumor growth. An established tumor needs nutrients and oxygen from the blood in order to grow and spread, and then several angiogenic factors are induced to promote the growth of new blood vessels. If the growth of blood vessels is blocked, the tumor will shrink or even disappear1. Several anti-angiogenic agents (for example, bevacizumab and sorafenib2,3) have been approved by the FDA because of their contribution to survival improvement when combined with chemotherapy or radiation in patients with advanced malignancies4,5. However, many angiogenesis inhibitor candidates are low molecular weight compounds with poor solubility and permeability and have short plasma circulation times. This limits their further clinical development due to low free drug concentration at the therapeutic target6. So, development of more effective targeting ligands to treat highly vascularised tumors remains as a great medical need.
The development of polymer-drug conjugates as prodrugs provides a chance to overcome these disadvantages and improve the pharmacokinetic (PK) properties and bioavailability of potential angiogenesis inhibitors7,8. Polymer-drug conjugates enter tissues only through gaps in angiogenic vessels, therefore with improved selectivity and reduction of systemic side effects9. Folkman’s group pioneered the concept of angiogenesis modulation and its potential impact on cancer therapy. In mice, they found that angiogenesis inhibitor-copolymer conjugates did not cross the blood-brain barrier and they accumulated less in normal organs, resulting in lower neurotoxicity10. They also demonstrated that conjugation of the potent, broad-spectrum angiogenesis inhibitor TNP-470 to monomethoxy-polyethylene glycol-polylactic acid to generate an oral formulation of nanopolymeric micelles improved TNP-470 inhibition of tumor angiogenesis in mice, and the conjugate did not cause neurotoxicity11. Akullian et al. developed an anti-angiogenic agent using XMT-1191-poly(1-hydroxymethylethylene hydroxymethyl formal) conjugate (XMT-1107) that enhanced anti-angiogenic and antitumor activity compared to its in vivo release XMT-1191 product. Additionally, XMT-1107 has enhanced anticancer activity compared to known anti-angiogenic agents TNP-470 and clinically effective sunitinib in a Caki-1 HTX model12. In a phase I study, Bendell et al. found that XMT-1191-poly(1-hydroxymethylethylene hydroxymethyl formal) conjugates inhibit methionine aminopeptidase 2 in leukocytes at all dose levels, with complete inhibition throughout a 21-day cycle in 6/7 patients evaluated for pharmacodynamics at doses above 325 mg/m2 (NCT01011972)13.
RGD (Arg-Gly-Asp) as the first anti-angiogenic small molecule targeting the integrin αvβ3 has attracted much attention. Cilengitide, a cyclic RGD-containing peptide, has finished clinical phase III for treatment of glioblastomas14,15. However, cilengitide failed to meet the primary endpoint of significantly increasing overall survival in certain patients with newly diagnosed glioblastoma16. It is now clear that the integrin αvβ3 receptor is more complex than initially thought17. Through this receptor, the thyroid hormones thyroxine (T4) and triiodothyronine (T3) activate the mitogen activated protein kinase (MAPK) and phosphoinositide 3-kinase (PI3K) signal transduction pathways that are linked to tumor cell proliferation18. From a molecular aspect, RGD peptides block the T3 receptor site, but cannot inhibit cell proliferation at the T4/T3 receptor site.
Diamino propane tetraiodothyroacetic acid (tetrac), named DAT, is a thyroid hormone derivative. It blocks the actions of agonist hormone analogs at both the T4/T3 receptor site and the T3-specific receptor site on integrin αvβ3 and controls proliferation of tumor cells19,20,21,22,23. The increased αvβ3 binding affinity of DAT versus tetrac is due to the addition of the basic moiety diamino propane (cationic) that enhances the binding into the RGD domain (aspartic acid, anionic pocket). Tetrac and its derivative DAT are hydrophobic in nature with limited aqueous solubility due to hydrophilic moieties within DAT including the COOH and the diamino propane upon raising the pH to form salt. However, low molecular weight DAT as a thyroid hormone derivative is able to diffuse normal vasculature and internalize into cells and therefore may influence gene expression24. DAT at the thyroid hormone receptor differentially regulates expression of several hundred specific genes relevant to cell division, anti-apoptosis, and angiogenesis, including VEGF, bFGF, PDGF, EGF, EGR17,24,25.
Conjugation of a biodegradable polymer with a hydrophobic small molecule such as tetrac derivative DAT may also enable imaging8. Kang et al. investigated tetrac-conjugated liposomes for tumor angiogenesis imaging. They used these small anti-angiogenic molecules with high binding affinity to integrin αvβ3 for the targeted delivery of liposomes to tumor tissues that express integrin αvβ326. Dehshahri’s group recently reported that tetrac-conjugated polyethylenimine nanoparticles (NPs) can be used for targeted delivery of plasmid encoding IL-12 gene into these αvβ3 overexpressing cells27. These recent developments of biodegradable polymer NPs represent a revolution in medicine and may lead to safer, more effective, and patient-specific therapeutics28,29,30,31. However, in vivo targeted drug delivery experimental results are still lacking.
We recently reported a strategy to synthesize tetrac-conjugated poly (lactic-co-glycolic acid) (PLGA) NPs32,33,34. Void PLGA NPs were prepared with a single emulsion method, followed by conjugation with tetrac on the surface of the PLGA NPs. The PLGA-tetrac NPs with large diameter not only reduced the side effects in mice by restricting the amount of tetrac taken up by cells, but also significantly improved the tumor bioavailability because of the enhanced permeability of tumor vasculature and the lack of lymphatic drainage—this is the enhanced permeability and retention (EPR) effect10,35,36,37,38,39. However, the density of tetrac on the NP surface is hard to control, and a loss of tetrac bioactivity was found following this chemical conjugation method33. We anticipate that the use of a high pressure microfluidizer will assist in optimizing DAT density. Therefore, design of site-specific linkers that do not affect a drug’s bioactivity and that minimize the polymer-drug conjugate’s heterogeneity is clearly the key step needed to move nanocarrier drug products into the clinic.
Herein, we report a general method to prepare DAT-conjugated PLGA NPs (NDAT) in water using a microfluidizer, starting from DAT-conjugated PLGA (PLGA-DAT). Because DAT is conjugated to the polymer via amide bonds and the amide bonds are hydrolytically stable, systemic toxicity due to DAT is avoided. NDAT has a longer plasma circulation time and enhances the possibility of NDAT binding thyro-integrin αvβ3 receptors, and NDAT as a NP would prohibit DAT access to the cell nucleus. We used poly (vinyl alcohol) (PVA) and deoxycholic acid (DCA) as emulsifiers to stabilize the NPs. A high concentration of emulsifier used without therapeutic effect is still a safety concern, for example, 5% PVA injected subcutaneously (s.c.) caused anemia and infiltrated various organs and tissues40. Highly concentrated PVA solution can increase osmolality and cause pain on injection41, and it may also influence the NPs’ bioactivity and binding with protein and then synergistically affect the biological fate of the NPs in vivo42,43,44. Here, a tangential flow filtration (TFF) method was used to remove the PVA.
Multiple experimental models were used to study DAT and NDAT properties in vitro and in vivo. To compare DAT and NDAT in vitro, we did an αvβ3-ligand binding assay and also studied the intracellular uptake and distribution of DAT and NDAT in U87 glioblastoma cells. In addition, we used LC-MS/MS to investigate the pharmacokinetics of DAT and NDAT in mouse plasma and their biodistribution in plasma and harvested organs from mice following administration of DAT and NDAT. In a different mouse model, we measured tumor weights from mice with U87 glioblastoma xenografts after NDAT treatment. Finally, experiments were done to study the efficacy of inhibition of angiogenesis by DAT and NDAT in a chick chorioallantoic membrane (CAM) model. Our current report supports the development of the next generation of DAT conjugated to NPs for cancer therapeutics.
Results and Discussion
Characterization of DAT and PLGA-DAT
PLGA-DAT consists of a hydrophobic biodegradable PLGA block and DAT tethers, conjugated via amide bonds as shown in Fig. 1a. The amine group of DAT is conjugated to the N-hydroxysuccinimide ester-activated carboxyl group via a diamino linkage. Further synthetic details for DAT and PLGA-DAT are provided in Supplementary Fig. S2. The presence of 79% of lactide units makes the biodegraded polymer more hydrophobic and thus it degrades more slowly because it absorbs less water45. The 79% of lactide units number was calculated from 1H NMR spectra using the known molecular weight of DAT, and DAT content was 12.9% in the resultant PLGA-DAT, calculated based on the repeat number of lactide and glycolide units.
For DAT, all the characteristic 1H NMR peaks were present (Fig. 1b), indicating that the noncleavable linker was conjugated to tetrac: diamino linkage (-CH2- of alkyl chain 1.94, 2.63 and 3.10 ppm), aminopropanol linkage (-CH2- of alkyl chain 1.65, 2.55 and 3.92 ppm), methylene group in the phenylacetic acid (3.17 ppm), and benzene ring (-ArH- groups at 7.14 and 7.77 ppm). This noncleavable linker may help to avoid nonspecific release of tetrac and tune affinity for the transporter. After DAT was conjugated to PLGA, all characteristic NMR peaks of the PLGA blocks were present (Fig. 1b): (lactide units CH3– and –CH– at 1.49 ppm and 5.22 ppm, glycolide units –CH2– at 4.91 ppm) and tetrac peaks a’, b’ (7.17 ppm, 7.88 ppm of its -ArH- groups). Peak h’ at 3.69 ppm in the PLGA-DAT spectrum was downfield-shifted from 3.10 ppm (peak h, the CH2 group in DAT), as was peak j’ at 2.60 ppm from 1.94 ppm (peak j, CH2 group in DAT). DAT peaks e (2.63 ppm), f (2.55 ppm) were shifted to 2.55 ppm (e’), 2.50 ppm (‘f’) in the PLGA-DAT spectrum. PLGA-DAT conjugation was also characterized with 13C NMR spectra (Supplementary Fig. S3). Only five major resonances from the PLGA polymer chain were apparent in the 13C NMR spectrum. Methyl and methine carbons of polylactide are at 20.28 and 72.47 ppm, respectively. Methylene carbons of polyglycolide are at 64.51 ppm, and 167.06 and 169.61 ppm peaks are from the carbonyl groups of PLGA. However, the expected carbon signals from DAT were not identifiable in the PLGA-DAT 13C NMR spectrum. To further identify PLGA-DAT conjugation, 1H-13C HSQC/HSQC-DEPT 2D and 1H-13C HMBC 2D NMR spectra were collected and also indicated that the PLGA was conjugated to DAT (Fig. 2). In the HSQC spectrum (Fig. 2a), the 1H/13C crosspeaks at 3.69 (h’)/52.8, 2.60 (j’)/25.5, and 2.55 (e’)/41.2 ppm were attributed to methylene groups in the diamino linkage. Crosspeaks at 2.50 (f’)/40.1, 1.15 (i’)/30.0, and 3.88 (c’)/71.6 belong to methylene groups in the aminopropanol linkage. The strong crosspeaks at 5.22 (k’)/69.4 and 4.88 (g’)/61.3 were attributed to methine and methane groups of the PLGA polymer units, and 1.46 (m’)/16.8 ppm was attributed to the methyl end group in the PLGA. In the HMBC spectrum (Fig. 2b), 1H-13C correlations between H-h’, j’ and C-n’ (3.69/170.9, 2.60/170.9, respectively) supported the PLGA-DAT structural assignment, further indicating that the PLGA was conjugated to DAT. Crosspeaks at 3.63/138.8, 3.63/142.0, and 3.63/173.0 ppm showed correlations between H-d’ and C-a’, o’, l’, respectively, of the tetrac part of the molecule.
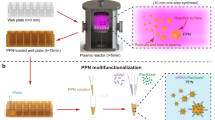
Preparation and characterization of NDAT
The cellular uptake of NPs may be size-dependent, and therefore a narrow distribution of NP sizes is important in considering clinical translation46,47,48. Nano-emulsions are kinetically stable liquid-in-liquid dispersions49, however, particle size and size distribution are affected by shear force. Conventional sonication’s drawbacks are the hard-to-form homogeneous shear force and formation of large temperature gradients50,51. To eliminate inhomogeneous shear force that leads to nonuniform rupturing, we passed the crude emulsion through a microfluidizer, which contains a shearing geometry with a fixed narrow gap—this gap can produce uniform simple shear. A spatially uniform simple shear force and better heat transfer owing to large surface areas leads to the monodisperse emulsion of smaller droplets52. After organic solvent is evaporated, PLGA-DAT can self-assemble to form NDAT in aqueous phase (Fig. 3a), and its biodegradable core is formed so that a chemotherapy drug can be encapsulated for controlled release for combination chemotherapy. Figure 3b shows the TEM image of NDAT prepared from PLGA-DAT. The overall diameter of NDAT was 95 ± 15 nm based on TEM measurement, which was confirmed with dynamic light scattering (DLS) (Supplementary Fig. S4), and is in accordance with the typical sizes of NPs of polymers previously reported53. Under TEM investigation, the bigger NDAT had better contrast because it contained more iodine per single NP. It should be noted that NDAT with surface protrusions was obtained. The formation of these protrusions is probably because of the presence of DAT on the surface of the NPs. DLS gives the hydrodynamic radius, while TEM gives the actual size of the particles. A single small molecule DAT will not be observed under TEM. TEM sample preparation typically consists of a drop-casting and drying process, and perhaps during the drying process there is assembly of several DATs within the NPs. Each DAT contains at least 4 iodine molecules and should have better contrast in TEM compared to the polymers (PLGA), thus the protrusions’ morphology was observed. This was not observed in void PLGA because it does not contain any DAT. Zeta potential of NDAT was −9 mv based on DLS characterization.
A more favourable PK profile can be achieved with high drug loading of the PLGA NPs used54. When we tried to remove PVA using a centrifugation method, the NPs aggregated and were difficult to disperse and had a low yield. The reason may be that the centrifugation forces and the presence of DAT on the surface of the NPs affected their stability. To reduce the amount of surfactant, we used TFF, which minimizes centrifugation forces and accumulation of NPs at the membrane surface. During TFF, solution volume was kept constant by adding new water as filtrate was removed. NDAT solution (0.5 mg/mL) was filtered at a flow rate of 20 mL/min, giving a flux of around 110 L/h × m2. Fifteen volumes of water were added compared to the initial feed volume to remove about 85% of the PVA and 98% of DCA using TFF. PVA was much more difficult to remove due to its low permeability and high molecular weight. The amount of PVA was determined with a colorimetric method based on the formation of PVA and iodine complex55. A small amount of PVA was still binding on the surface of NPs after TFF purification. PVA and DCA have amphiphilic features, thus, they prefer to adsorb at a water/ethyl acetate interface. After ethyl acetate diffused into the aqueous phase, the droplets of emulsion shrank, and DAT had amphiphile structural features; it segregated into the water/ethyl acetate interface, a process that is driven by the minimization of the Helmholtz free energy. For long-term storage, 2% sucrose was added to the NPs as a cryoprotectant to prevent aggregation56,57. Then, a small amount of PVA and DCA were kinetically trapped within the PLGA NP surface owing to the glassy nature of PLGA.
αvβ3-Ligand binding assay of tetrac, DAT, and NDAT
Integrin αvβ3 is highly expressed in angiogenic endothelial cells and has been implicated in angiogenic processes. To evaluate the integrin αvβ3 binding ability of tetrac, DAT, and NDAT, we tested these compounds in a αvβ3-ligand binding assay. The 50% inhibitory concentration (IC50 value) of NDAT was 0.15 nM and of DAT was 0.32 nM, which were 416 and 195 times, respectively, higher than that of tetrac (62.4 nM) (Fig. 4). The higher binding affinity of NDAT may be attributed to a diamino linkage and could increase inhibitory activity to integrin αvβ3. Our group has previously compared potency of DAT and NDAT in vitro in a perfused MDA-MB breast cancer cell culture system for 9 days; results indicated that the antiproliferative effect of NDAT is greater than that of DAT because the DAT is distributed throughout the intracellular and extracellular volumes, whereas little NDAT enters the intracellular space58. NDAT combines both delivery systems (active targeting via αvβ3 tumor targeting and its microenvironment as well as the passive EPR transport into leaky tumors). A NP surface carrying a number of DAT molecules is more effective than the αvβ3 antagonist DAT molecule.
Intracellular uptake and distribution of DAT and NDAT in U87 glioblastoma cells
To further understand NDAT’s more effective binding to integrin αvβ3’s cell surface receptor and its inability to enter cells, the intracellular uptake and distribution of DAT and NDAT in U87 glioblastoma cells with 4 hours’ incubation was studied with confocal microscopy (Fig. 5). Results showed that DAT passed through cell membrane and penetrated to the cell nucleus, however, NDAT did not go to the nucleus. This observation is in a good agreement with experimental results reported previously34.
Confocal microscopy images of U87 cells incubated for 4 hours with Cy5 dye-labelled DAT (a) and NDAT (b). DAT reached the nucleus, and NDAT was restricted from going inside the nucleus. Cells were counter-stained with DAPI (4′,6-diamidino-2-phenylindole) to visualize the nuclei: blue for DAPI and red for Cy5. Magnification, 63X.
LC-MS/MS determination of DAT and NDAT in plasma
In preparation for the in vivo mice study to determine the PK of DAT and NDAT, we tested DAT and PLGA-DAT (as a standard for NDAT because it is a single entity of NDAT) in blank mouse plasma and set up a liquid chromatography-tandem mass spectrometry (LC-MS/MS) method with in-source decay or fragmentation of PLGA-DAT and a simple extraction procedure with a short chromatographic run time (Fig. 6). The tandem mass spectrometer is a triple quadrupole system consisting of three quadrupoles (Q); Q1 and Q3 are mass filters and Q2 is a collision cell. The method developed here relies on in-source fragmentation of PLGA-DAT followed by MS/MS fragmentation of the DAT ion molecule that results from in-source decay. Briefly, after chromatographic separation, the PLGA-DAT underwent an in-source collision-induced dissociation (CID) in the ionization source of the mass spectrometer with an extremely high declustering potential (DP, 180 V), where the DAT was generated and used as the surrogate signal ions to quantify PLGA-DAT in samples, similar in concept as described for quantification of PEGylated compounds59,60. Specifically, the tandem mass spectrum of the [M + H]+ m/z 862.9 precursor ion of DAT confirmed the integrity as shown in Fig. 6a. The predominant charged protonated precursor [M + H]+ of PLGA-DAT was observed at 862.9 m/z after the in-source CID, indicating that DAT was released from PLGA-DAT. The most abundant signal in product ion 845.7 m/z was observed after the further CID fragmentation of DAT ion molecule resulting from in-source decay. The mass difference between the parent ion and daughter ion was that of neutral loss of ammonia(Fig. 6b). When running LC-MS/MS at a low DP voltage (75 V), a broad peak of PLGA-DAT appeared due to the polymeric species being incompletely dissociated (data not shown). As expected, the PLGA-DAT eluted after DAT in the LC-MS/MS chromatogram. This is because the higher hydrophobicity of PLGA polymer increases its interaction with the column stationary phase in reversed phase HPLC. As shown in Fig. 6c, the 50 ng/mL of deuterium-labelled DAT-D7 (used as internal standard) and 150 ng/mL DAT exhibited good signal-to-noise (S/N) ratio and eluted as a sharp peak at the same retention time, 1.89 min. The detected S/N was higher, resulting in lower limit of quantitation (LOQ). Fifty ng/mL of DAT-D7 and 500 ng/mL PLGA-DAT exhibited good S/N ratio. Free DAT eluted as a single peak with a retention time of 1.89 min, whereas the PLGA-DAT conjugate eluted as a wide series of peaks around 2.40 min (Fig. 6d) due to the heterogeneity of PLGA-DAT. A small peak of PLGA-DAT showed the same retention time as DAT-D7 and this can be attributed to the physiological degradation of PLGA in mouse plasma and release of free DAT. The linear range of PLGA-DAT and DAT in multiple reaction monitoring (MRM) mode using electrospray ionization was 3 orders of magnitude and no saturation of response was observed up to 3000 ng/mL (Supplementary Fig. S7a,b). The overall mean recoveries for DAT and PLGA-DAT were above 80% (Supplementary Fig. S7c,d).
Pharmacokinetics of DAT and NDAT in vivo
To test the ability of NDAT to enhance PK in vivo, we studied the plasma DAT level following administration of DAT/Cremophor EL and NDAT to mice. The logarithmic concentration time curve of DAT in plasma after s.c. injection of DAT/Cremophor EL and NDAT is shown in Fig. 7. Cmax was at 2.8 hours after s.c. injection of DAT/Cremophor EL micelles, and the plasma DAT concentration was 548 ng/mL to 7 ng/mL from 0.25 hours to 48 hours. This result is similar to the clinical PK of paclitaxel/Cremophor EL in human blood61,62. On the other hand, s.c. injection of the same DAT-equivalent dosage of NDAT resulted in a plasma DAT concentration of 4363 ng/mL to 189 ng/mL from 0.25 hours to 48 hours, which was 2 orders of magnitude higher. This was a 4-fold higher AUC0–48h than for DAT/Cremophor EL, and lower clearance (2.4 mL/hour) than for DAT/Cremophor EL (9.1 mL/hour), reflecting the 10-fold difference in concentration63. The plasma PK profile of NDAT is best described by a two-compartment model with a distributional phase (T1/2α = 0.4 hours) and elimination phase (T1/2 β = 15.5 hours). We know that NPs accumulate into extravascular tumor tissue through a passive process that requires a high plasma DAT level and can be maintained longer to facilitate time-dependent extravasation through the leaky tumor microvasculature. NDAT can result in higher DAT tumor concentration (Table 1, and Supplementary Figs S8, S9). In these mouse PK studies of NDAT, the plasma NDAT level declined biophysically with a distributive T1/2α of 0.4 hours. The distribution phase appeared approximately 6 hours after administration of NDAT. Decline in the plasma concentration of DAT in the terminal phase is slow, and the plasma DAT level can maintain 300 ng/mL after 48 hours post-administration of NDAT. This high plasma level of DAT is associated with high systemic exposure consistent with paclitaxel conjugate with poly-L-glutamic acid, which is ongoing in a phase III trial (NCT00108745)64,65. However, longer Tmax (2.87 hours) of s.c. administered DAT/Cremophor EL was observed. A reason for this may be that DAT/Cremophor EL has slow transport through the extracellular matrix prior to reaching capillaries. The DAT/Cremophor EL declined in a monophasic manner. This may contribute to longer Tmax, and first distribution phase is not observed66.
Mouse plasma DAT level versus time profiles. Different formulations of DAT/Cremophor EL micelles (black) and NDAT nanoformulation (red) were administered subcutaneously into mice at dose of 3 mg (DAT-equivalent)/kg body weight. NDAT was purified with dialysis (without using tangential flow filtration, TFF) before injection. Data are shown as mean ± SD (n = 4).
NDAT versus DAT showed greater antiproliferative activity and inhibition of ERK phosphorylation (p-ERK1/2) without any significant effect on total ERK. Representative western blot bands for phospho-ERK1/2 and total ERK1/2 are shown in Fig. S6.
Biodistribution of DAT and NDAT in vivo
Two distinct phases in the plasma DAT concentration versus time were observed (Fig. 7), and in the initial steep distributional phase, NDAT nanoformulation may enhance the delivery of DAT to different organs and therefore possibly cause certain side effects. Subsequently, biodistribution studies were performed by injecting s.c. 3 mg/kg of DAT/Cremophor EL micelles and NDAT into mice. Then, the DAT levels in plasma and harvested heart, lung, liver, spleen, and kidney were determined at 4 and 48 hours with LC-MS/MS (Fig. 8). Limited amounts of DAT were detected in plasma and all organs after 48 hours (Fig. 8b), indicating that clearance of DAT/Cremophor EL micelles was consistent with previous reports of Cremophor EL-mediated paclitaxel distribution67. The concentration of NDAT was higher than DAT/Cremophor EL micelles in all tissues. Compared with DAT/Cremophor EL micelles, the biodistribution of NDAT at equivalent DAT dose showed an EPR effect for NPs. The highest concentrations of DAT were in the spleen, heart, and liver at 4 hours. Between 4 and 48 hours after administration, the DAT level in spleen, heart, and liver decreased 15-fold, 9-fold, and 3-fold, respectively. This may be because serum proteins bind to NDAT, which is then recognized by scavenger receptors on the macrophage cell surface68. This result is also consistent with previous reports that introduction of RGD-based targeting moieties leads to an increase in immunogenicity and protein adsorption on the nanoparticles69. PLGA nano has greater tendency to accumulate in the heart, which is in agreement with other PLGA nano delivery systems versus a PLGA-polyethylene glycol (PEG) nano system that showed lesser delivery into the heart70. The exact mechanism is not clear except that PLGA NPs have high entrapment into the heart, which can be reduced by PEGylation. The toxicity of DAT is related to the free DAT level in different tissues, and here the free DAT level is relatively low because DAT was chemically conjugated with PLGA polymer, thus side effects from NDAT are expected to be less than from the free DAT form. To avoid accumulation of NDAT in tissues, once-a-week administration of NDAT should be selected for multi-dose administration.
Biodistribution of DAT administered subcutaneously into mice at equivalent DAT amount of 3 mg/kg body weight (a) as NDAT nanoformulation, and (b) as DAT/Cremophor EL micelles formulation. Shown are DAT amounts in plasma and major organs (heart, lung, liver, spleen, and kidney) determined at 4 and 48 hours. Data are shown as mean ± SD (n = 4), and all data have significance (P < 0.001) for NDAT compared to DAT.
Xenograft tumor weight after NDAT treatment
To further study the antitumor effect, U87 glioblastoma cells were implanted in each flank of nude mice, and then the mice were treated daily for 27 days with void PLGA NPs or NDAT at equivalent DAT amounts of 0.1, 0.3, 1, and 3 mg/kg body weight (Fig. 9). NDAT at doses of 1 and 3 mg/kg led to significant reduction of tumor growth. Mean tumor weights were reduced by 61% for 1 mg/kg treatment and 83% for 3 mg/kg treatment. In contrast, treatment with low doses of NDAT (0.1 and 0.3 mg/kg) did not significantly reduce tumor weight. Our results agree with our hypothesis that anti-angiogenic therapy reduces glioma growth in vivo that is related to U87 glioblastoma cell regression following vascular reduction. Results also showed that tumor weight reductions after NDAT treatment are indeed dose-dependent.
NDAT administered daily for 20 days at 1 mg/kg, s.c. resulted in greater tumor volume suppression versus DAT administered daily for 20 days at 10 mg/kg, s.c. (Fig. 10a). Neither DAT or NDAT at daily s.c. doses of 0.3, 1, 10, or 30 mg/kg body weight (DAT equivalent) for 2 weeks in male or female mice showed any histological changes in key organs examined including heart, lung, liver, kidney, and brain (data not shown).
(a) NDAT administered daily for 20 days at 1 mg/kg subcutaneously (s.c.) resulted in greater tumor volume suppression versus DAT administered daily for 20 days at 10 mg/kg, s.c. (b) Images for suppression of b-FGF-induced angiogenesis in the chick chorioallantoic membrane (CAM) model by DAT versus NDAT at 500 ng/CAM. Data illustrate greater anti-angiogenesis efficacy of NDAT versus DAT at the same concentration.
Chorioallantoic membrane assay of angiogenesis
The CAM model was used to simulate in vivo anti-angiogenic activities of NDAT. First, basic fibroblast growth factor 2 (FGF2, or b-FGF) was used to stimulate angiogenesis, and then equivalent DAT amounts of unconjugated DAT and NDAT were administered. DAT induced 48% inhibition of angiogenesis levels at 500 ng/CAM, while NDAT induced 45% inhibition of angiogenesis levels at low doses (50 ng/CAM), which was 10-fold less than that of unconjugated DAT (Table 2). This result is similar to our previous human medullary thyroid carcinoma xenograft study in nude mice33. PLGA-tetrac NPs with one-tenth of tetrac doses achieved the same angiogenesis inhibition as that of unconjugated tetrac. We presume that the successful treatment is due to two reasons: (1) NDAT improves the solubility of DAT and is more likely to freely pass through the surface epithelium and reach the vessels in the stroma71, and (2) NPs prohibit cell entry of DAT and improve the efficiency of DAT’s action at the hormone receptor on the extracellular domain of plasma membrane integrin αvβ3. NDAT has greater potency than unmodified DAT at the integrin and affects a broader range of cancer-relevant genes25. Images for suppression of b-FGF-induced angiogenesis in the CAM model by DAT versus NDAT at 500 ng/CAM are shown in Fig. 10b. Data illustrate greater anti-angiogenesis efficacy of NDAT versus DAT at the same concentration.
Conclusions
In summary, we demonstrated a facile approach to prepare DAT-conjugated PLGA NPs (NDAT). A rapid and reliable LC-MS/MS method was developed to evaluate the fate of DAT in mouse plasma following administration by s.c. injection into mice of unconjugated DAT and NDAT. In PK studies, NDAT remained in plasma at a concentration 10 times higher than unconjugated DAT. In a CAM growth factor-mediated angiogenesis model, NDAT at one-tenth the dose of tetrac can achieve the same vascular supply decrease as that of unconjugated DAT due to the NPs’ preferential tumor accumulation, which can increase efficacy and decrease toxicity. NDAT at 1 and 3 mg/kg significantly decreased U87 tumor growth in mice. Our study may help to improve understanding of the mechanisms of NDAT and guide future preclinical trials. The self-assembled NDAT may find promising applications in combining anti-angiogenics with chemotherapy.
Methods
Materials
Diamino tetraiodothyroacetic acid (DAT), deuterium-labelled DAT-D7 as internal standard, and DAT-conjugated PLGA polymer (PLGA-DAT) were synthesized by DPx Fine Chemicals (Regensburg, Germany). PLGA (average MW 8,000 g/mol), lactide:glycolide (79:21), Cremophor EL, acetonitrile (>99%), DMSO (99.9%), ethyl acetate (99.8%), poly (vinyl alcohol) (PVA, hydrolysed 88%, average MW 31,000 g/mol), deoxycholic acid (DCA, >99%), formic acid (>99.5%), and bovine serum albumin (BSA) were purchased from Sigma-Aldrich (St. Louis, MO) and used without further purification unless otherwise noted. Freeze-drying was performed using a Millrock Tech MD85 Console Manifold Freeze Dryer (Millrock Technology, Kingston, NY). Deionized water with resistivity of 18.0 MΩ was used in all experiments. Purified αvβ3 and anti-αvβ3 conjugated with biotin were obtained from Bioss Inc (Woburn, MA), streptavidin HRP conjugate were from Thermo Fisher Scientific (Grand Island, NY), fibrinogen was from Millipore Sigma (Burlington, MA), Cy5-NHS dye was from Lumiprobe (Hunt Valley, MD), and 3,3′,5,5′-tetramethylbenzidine (TMB) and TMB-stop solution were from ABCAM Inc (Cambridge, MA). Blank mouse plasma for the PK study of PLGA-DAT versus DAT was from BioreclamationIVT (Westbury, NY).
Preparation of DAT/Cremophor EL formulation
DAT (10 mg) was dissolved in 0.4 mL Cremophor EL/ethanol (1:1, v/v) and then added to 2 mL of water. The solution was sonicated for ~30 seconds using a probe sonicator. An optically transparent nano-emulsion formulation was obtained72. The nano-emulsion size was confirmed using dynamic light scattering (DLS).
Preparation of NDAT via single emulsion/solvent diffusion process
PLGA-DAT (100 mg) was dissolved in ethyl acetate (10 mL), yielding a 10 mg/mL polymer solution that was stirred for 30 minutes at room temperature. Subsequently, the polymer solution was added dropwise to water (100 mL) containing PVA (1 g) and DCA (1 g) and sonicated for 2 minutes. The crude emulsion was passed through a high shear force LM 10 microfluidizer (Microfluidics Corp., Westwood, MA) at 20,000 psi. The entire solution was passed through the microfluidizer 3 to 5 times until samples had uniform size. Nano-emulsion size was also confirmed with DLS. The solutions were dialyzed against water using a dialysis membrane (MWCO 12–14 kDa) for 2 days to remove ethyl acetate. To remove residual emulsifier, a tangential flow filtration system (TFF, Pall Corp., Port Washington, NY) with a 300 kDa MWCO membrane was used, and the residual emulsifier was evaluated55,73.
Freeze-drying
The freeze-drying procedure was performed to impart stability and improve the shelf-life of the developed formulations. In brief, 100 mL of the NP suspension was placed in a 600 mL glass flask. Sucrose 2% (w/v) was added as a cryoprotectant to preserve the NP properties during the freezing step. Then the solution was frozen at −85 °C for 12 hours and afterward it was sublimated for 48 hours under pressure of 20 mT at room temperature. Finally, the NPs were collected and preserved in a freezer at 4 °C for later evaluation and analysis57.
Determination of the DAT conjugation efficiency and loading capacity
The conjugation efficiency of DAT into NDAT was determined by analysing centrifuged NDAT compared to the initial amount of DAT74. After lyophilization, the weighed NDAT powder was dispersed in 15 mL acetonitrile and sonicated for 10 minutes until a clear solution was observed. The amount of DAT in the acetonitrile was determined at 227 nm using HPLC. DAT conjugation efficiency was 98%, and DAT loading capacity was 9% w/w, which were calculated from Eqs 1 and 2, respectively:
and
Confocal fluorescence microscopy imaging
U87 cells were plated on a coverslip in a 6-well plate at 0.5×106 cells/mL with appropriate growth media and allowed to attach for about 24 hours. Then the media was aspirated and 1 mL of fresh media was added. Cells were treated with 100 uL of Cy5-NDAT and Cy5-DAT for 4 hours. After incubation, the cells were removed and washed several times with PBS and then fixed in 1% formaldehyde (Sigma-Aldrich). Confocal imaging was performed using a Leica TCS SP5 confocal microscope with a 63x objective. A 633 nm laser was used for excitation, and emission was detected between 650 nm and 720 nm.
PK study of DAT and PLGA-DAT (as standard for NDAT) in blank mouse plasma with LC-MS/MS
LC-MS/MS analysis was performed on an API 4000 triple quad mass spectrometer (ABSCIEX, Framingham, MA) configured with a Shimadzu LC-20AD pumping system, a SIL-20AC auto sampler, and CTO-20AC column oven. The system was operated under Analyst 1.62 control. Chromatographic separation of DAT was achieved on a Discovery® BIO (Sigma-Aldrich) Wide Pore C18 300 Å column, 50 × 2.1 mm ID, packed with 3.0 μm particles and the flow rate was 0.4 mL/minute under gradient conditions: 25–92% B in 2.8 min, 92% B in 1 min, and 98–25% in 1 min, where solvent A was 0.2% formic acid in water and solvent B was 0.1% formic acid in 90% acetonitrile and 10% isopropanol. The total run time was 6 minutes. The column oven temperature was 35 °C and sample injection volume was 10 µL. Multiple ion monitoring (MRM) transitions for PLGA-DAT, DAT, and internal standard DAT-D7 were m/z 862.9 > 845.9 with a declustering potential (DP) of 180 V, 862.9 > 845.7 with a DP of 95 V, and 869.9 > 851.7 with a DP of 95 V, respectively. The instrument was operated in a positive ion mode with a turbo V electrospray source, with parameters: curtain gas, 20 psi; heated nebulizer temperature 500 °C; ion spray voltage, 4500 V; gas 1, 60 psi; gas 2, 55 psi; EP, 10 V; CE, 44 V; CXP, 27 V; and collision gas, 6.0 psi. Dwell time for each transition was 150 ms. Calibration curves were plotted using linear regression with a weight factor of 1/x. PK data analysis was carried out using WinNonlin software (version 5.2, Pharsight, Mountain View, CA) with one compartment first order, no lag time, first order elimination and two compartments first order, macro-constants, no lag time, first order elimination. The area from 0 to 48 hours under the DAT concentration time curve was used to determine the area under the curve (AUC). All other parameters including Cmax, Tmax and t1/2 were determined with WinNonlin software as well.
To determine the concentration of PLGA-DAT in mouse plasma, 20 µL plasma was added to 10 µL of 50 ng/mL DAT-D7 and then extracted with 200 µL of acetonitrile by vortexing vigorously and sonicating for 15 minutes, followed by centrifugation at 18,800 × g for 50 minutes at 4 °C. Supernatant (200 µL) was removed and dried under N2. Dried samples were reconstituted with 0.1% formic acid in 100 µL of 40% acetonitrile and the mixture was vortexed. The 20 µL sample was used for LC-MS/MS analysis as described above for DAT. To determine accuracy and precision, two calibration curves for DAT and PLGA-DAT were prepared by spiking DAT and PLGA-DAT at different concentrations (0.5 to 1000 ng/mL) into 20 µL mouse plasma using a 2-fold series dilution method. DAT and PLGA-DAT were extracted and analysed with LC-MS/MS. Ratios of peak areas to the corresponding internal standard DAT-D7 were plotted against DAT and PLGA-DAT concentrations. Calibration curve fitting was done with linear regression, and the standard deviation value was within ± 20%. In order to pass our acceptance criteria, no more than 2 standard levels or 2 adjacent standard deviations in the calibration curve could fail.
Animals
All animal studies were conducted at the animal facility of the Veteran Affairs Medical Center, Albany, NY, in accordance with the institutional guidelines for humane animal treatment and according to the current NIH guidelines. Animal protocols were approved by the Veteran Affairs Medical Center Institutional Animal Care and Use Committee (Albany, NY).
In vivo PK study
Male C57BL/6 mice were aged 5–6 weeks, weighed 18–20 g, and were purchased from Harlan Laboratories (Indianapolis, IN). Mice were maintained under specific pathogen-free conditions and housed 5–6 per cage under controlled conditions of temperature (20 ± 2 °C), humidity (50 ± 10%), and 12 hours light/dark cycle. Animals were fed a standard pelleted mouse chow. Mice were allowed to acclimatize for 5 days prior to the start of the study. A total of 12 mice were randomized by weight into 3 groups (n = 4). Mice were not anesthetized during the study. The total volume of the DAT or NDAT solution administered was 0.12 mL. The DAT/Cremophor EL formulations were administered parenterally at doses of 3 mg/kg and 30 mg/kg body weight, and NDAT formulations were administered at a dose of 3 mg DAT-equivalent/kg body weight. Blood (30 µL) was collected using a heparinized capillary from the retro orbital venous plexus at 0.25, 0.5, 1, 3, 6, 12, 24, and 48 hours post administration for PK profile determination using established LC-MS/MS methods on the API 4000 triple quad mass spectrometer.
In vivo biodistribution study
Male C57BL/6 mice as described above were used for treatment and subsequent tissue sample collection for a biodistribution study. Sixteen mice were randomized by weight into 4 groups (n = 4 each). Single doses at equivalent DAT amount of 3 mg/kg body weight were administered s.c. of DAT/Cremophor EL micelles (2 groups of mice) or of NDAT (2 groups of mice). One group of DAT-treated and one group of NDAT-treated mice were sacrificed at 4 hours, and the other two groups were sacrificed at 48 hours. After sacrifice, blood, liver, spleen, kidney, lungs, and heart were harvested and homogenized with 1 mL of acetonitrile, followed by centrifugation at 18,800 x g for 30 minutes at 4 °C. Supernatant (1 mL) was removed and dried under N2. Dried samples were reconstituted with 0.1% formic acid in 100 µL of acetonitrile.
Xenograft tumor weight study
Human glioblastoma U87 cells (ATCC, Manassas, VA) were used for the tumor weight study. Cells were grown in DMEM supplemented with 10% fetal bovine serum, 1% penicillin, and 1% streptomycin. Cells were cultured at 37 °C to sub-confluence and treated with 0.25% (w/v) trypsin/EDTA to effect cell release from culture flask. Twenty immunodeficient, female NCr nude homozygous mice (Envigo, Indianapolis, IN) were aged 5–6 weeks and weighed between 18 and 20 g. Mice were implanted s.c. with 2 × 106 U87-luc cells in each flank. After 2 weeks when the tumor reached targeted volume (<2,000 mm3), the mice were randomized according to tumor volume into 5 groups (n = 4 each). Mice were treated daily for 27 days s.c. with void PLGA NPs, or NDAT at equivalent DAT amounts of 0.1, 0.3, 1, and 3 mg/kg body weight. All mice were sacrificed after 27 days and tumors were harvested.
CAM growth factors-mediated angiogenesis assay
The relative anti-angiogenesis potency of DAT and NDAT were examined in the chick chorioallantoic membrane (CAM) model of angiogenesis as previously described75,76,77, using ten-day old chick embryos. Fibroblast growth factor 2 (FGF2, 1 μg/mL, dissolved in PBS), was used as a standard pro-angiogenic agent to induce new blood vessel branches on the CAM. Sterile 1.0 cm diameter disks of #1 filter paper were pretreated with 3 mg/mL cortisone acetate and air dried under sterile conditions. PBS (control) and FGF2 with DAT or NDAT (50 and 500 ng/CAM) were then applied to the pretreated disks and dried. The disks were placed on growing CAMs in an area between pre-existing vessels. After incubation at 37 °C with 55% relative humidity for 3 days, the CAM tissue directly beneath each filter disk was resected from the control and treated CAM samples. Tissues were washed 3 times with PBS, placed in 35-mm Petri dishes and examined under an SV6 stereomicroscope (Karl Zeiss, Thornwood, NY) at 50x magnification. Digital images of the CAM sections were collected using a 3-CCD color video camera system, and analyzed with Image-Pro software (Media Cybernetics, Silver Spring, MD). The numbers of vessel branch points contained in a circular region equal to the area of each filter disk were counted. One image was counted in each CAM preparation, and findings from 8 CAM preparations/group were used for each treatment condition.
Statistics
Statistical values reported were calculated with GraphPad Prism 7 software (GraphPad, San Diego, CA) and statistical significance was defined as P < 0.05.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Change history
03 October 2023
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1038/s41598-023-43642-5
References
Ferrara, N. & Kerbel, R. S. Angiogenesis as a therapeutic target. Nature 438, 967–974 (2005).
Carmeliet, P. Angiogenesis in health and disease. Nat. Med. 9, 653–660 (2003).
Mousa, S. A. & Davis, P. J. In Angiogenesis Modulations in Health and Disease (eds Mousa, S.A. & Davis, P.J.) (Springer, 2013).
Sagar, S. M., Yance, D. & Wong, R. Natural health products that inhibit angiogenesis: A potential source for investigational new agents to treat cancer. Curr. Oncol. 13, 14–26 (2006).
Kerbel, R. S. Tumor angiogenesis. N. Engl. J. Med. 358, 2039–2049 (2008).
Smith, D. A., Di, L. & Kerns, E. H. The effect of plasma protein binding on in vivo efficacy: Misconceptions in drug discovery. Nat. Rev. Drug Discov. 9, 929–939 (2010).
Rautio, J. et al. Prodrugs: Design and clinical applications. Nat. Rev. Drug Discov. 7, 255–270 (2008).
Markovsky, E. et al. Administration, distribution, metabolism and elimination of polymer therapeutics. J. Control. Release 161, 446–460 (2012).
Folkman, J. Tumor angiogenesis: Therapeutic implications. N Engl J Med 285, 1182–1186 (1971).
Satchi-Fainaro, R. et al. Targeting angiogenesis with a conjugate of HPMA copolymer and TNP-470. Nat. Med. 10, 255–261 (2004).
Benny, O. et al. An orally delivered small-molecule formulation with antiangiogenic and anticancer activity. Nat. Biotechnol. 26, 799–807 (2008).
Akullian, L., Stevenson, C., Lowinger, T. & Fram, R. Abstract #670: Anti-angiogenic and antitumor activity of XMT-1107, a fumagillin-derived polymer conjugate, and its in vivo release product XMT-1191. Cancer Res. 69, 670–670 (2009).
Bendell, J. C. et al. Abstract#2526: A phase 1 first-in-human study of XMT-1107, a polymer-conjugated fumagillol derivative, in patients (pts) with advanced solid tumors. J. Clin. Oncol. 32, 2526–2526 (2014).
Hariharan, S. et al. Assessment of the biological and pharmacological effects of the ανβ3 and ανβ5 integrin receptor antagonist, cilengitide (EMD 121974), in patients with advanced solid tumors. Ann. Oncol. 18, 1400–1407 (2007).
Mas-Moruno, C., Rechenmacher, F. & Kessler, H. Cilengitide: The first anti-angiogenic small molecule drug candidate design, synthesis and clinical evaluation. Anticancer Agents Med. Chem. 10, 753–768 (2010).
Hatley, R. J. D. et al. An αv-RGD integrin inhibitor toolbox: Drug discovery insight, challenges and opportunities. Angew. Chem. Int. Ed. Engl. 57, 3298–3321 (2018).
Cheng, S. Y., Leonard, J. L. & Davis, P. J. Molecular aspects of thyroid hormone actions. Endocr. Rev. 31, 139–170 (2010).
Cohen, K. et al. Thyroid hormone is a MAPK-dependent growth factor for human myeloma cells acting via αvβ3 integrin. Mol. Cancer Res. 9, 1385–1394 (2011).
Mousa, S. A. et al. Tetraiodothyroacetic acid and its nanoformulation inhibit thyroid hormone stimulation of non-small cell lung cancer cells in vitro and its growth in xenografts. Lung Cancer 76, 39–45 (2012).
Lin, H. Y. et al. Actions of L-thyroxine and Nano-diamino-tetrac (Nanotetrac) on PD-L1 in cancer cells. Steroids 114, 59–67 (2016).
Sudha, T. et al. Nanoparticulate tetrac inhibits growth and vascularity of glioblastoma xenografts. Horm. Cancer 8, 157–165 (2017).
Sudha, T. et al. Targeted delivery of cisplatin to tumor xenografts via the nanoparticle component of nano-diamino-tetrac. Nanomedicine (Lond) 12, 195–205 (2017).
Sudha, T. et al. Targeted delivery of paclitaxel and doxorubicin to cancer xenografts via the nanoparticle of nano-diamino-tetrac. Int. J. Nanomed. 12, 1305–1315 (2017).
Davis, P. J., Goglia, F. & Leonard, J. L. Nongenomic actions of thyroid hormone. Nat. Rev. Endocrinol. 12, 111–121 (2016).
Davis, P. J. et al. Cancer cell gene expression modulated from plasma membrane integrin αvβ3 by thyroid hormone and nanoparticulate tetrac. Front. Endocrinol. (Lausanne) 5, 240 (2014).
Kang, C. M. et al. 64Cu-labeled tetraiodothyroacetic acid-conjugated liposomes for PET imaging of tumor angiogenesis. Nucl. Med. Biol. 40, 1018–1024 (2013).
Sheikhsaran, F., Sadeghpour, H., Khalvati, B., Entezar-Almahdi, E. & Dehshahri, A. Tetraiodothyroacetic acid-conjugated polyethylenimine for integrin receptor mediated delivery of the plasmid encoding IL-12 gene. Colloids Surf. B. Biointerfaces 150, 426–436 (2017).
Venditto, V. J. & Szoka, F. C. Jr. Cancer nanomedicines: So many papers and so few drugs! Adv. Drug Del. Rev. 65, 80–88 (2013).
Collins, F. S. & Varmus, H. A new initiative on precision medicine. N. Engl. J. Med. 372, 793–795 (2015).
Min, Y., Caster, J. M., Eblan, M. J. & Wang, A. Z. Clinical translation of nanomedicine. Chem. Rev. 115, 11147–11190 (2015).
Kamaly, N., Yameen, B., Wu, J. & Farokhzad, O. C. Degradable controlled-release polymers and polymeric nanoparticles: Mechanisms of controlling drug release. Chem. Rev. 116, 2602–2663 (2016).
Yalcin, M. et al. Tetraidothyroacetic acid (tetrac) and tetrac nanoparticles inhibit growth of human renal cell carcinoma xenografts. Anticancer Res. 29, 3825–3831 (2009).
Yalcin, M. et al. Tetraiodothyroacetic acid (tetrac) and nanoparticulate tetrac arrest growth of medullary carcinoma of the thyroid. J. Clin. Endocrinol. Metab. 95, 1972–1980 (2010).
Bharali, D. J., Yalcin, M., Davis, P. J. & Mousa, S. A. Tetraiodothyroacetic acid-conjugated PLGA nanoparticles: A nanomedicine approach to treat drug-resistant breast cancer. Nanomedicine (Lond) 8, 1943–1954 (2013).
Alexis, F., Pridgen, E., Molnar, L. K. & Farokhzad, O. C. Factors affecting the clearance and biodistribution of polymeric nanoparticles. Mol. Pharmacol. 5, 505–515 (2008).
Cabral, H. et al. Accumulation of sub-100 nm polymeric micelles in poorly permeable tumours depends on size. Nat. Nanotech. 6, 815–823 (2011).
Cabral, H. & Kataoka, K. Progress of drug-loaded polymeric micelles into clinical studies. J. Control. Release 190, 465–476 (2014).
Mitragotri, S., Burke, P. A. & Langer, R. Overcoming the challenges in administering biopharmaceuticals: Formulation and delivery strategies. Nat. Rev. Drug Discov. 13, 655–672 (2014).
Yasunaga, M. et al. Development of antibody-drug conjugates using DDS and molecular imaging. Bioengineering (Basel) 4, (78 (2017).
Rowe, R. C., Sheskey, P. J. & Owen, S. C. Handbook of Pharmaceutical Excipients. 6th edn, (Pharmaceutical Press London, 2006).
Klement, W. & Arndt, J. Pain on iv injection of some anaesthetic agents is evoked by the unphysiological osmolality or pH of their formulations. Br. J. Anaesth. 66, 189–195 (1991).
Lynch, I., Salvati, A. & Dawson, K. A. Protein-nanoparticle interactions: What does the cell see? Nat. Nanotech. 4, 546–547 (2009).
Docter, D. et al. The nanoparticle biomolecule corona: Lessons learned - challenge accepted? Chem. Soc. Rev. 44, 6094–6121 (2015).
Li, W., Yalcin, M., Lin, Q., Ardawi, M. M. & Mousa, S. A. Self-assembly of green tea catechin derivatives in nanoparticles for oral lycopene delivery. J. Control. Release 248, 117–124 (2017).
Makadia, H. K. & Siegel, S. J. Poly lactic-co-glycolic acid (PLGA) as biodegradable controlled drug delivery carrier. Polymers (Basel) 3, (1377–1397 (2011).
Jin, H., Heller, D. A., Sharma, R. & Strano, M. S. Size-dependent cellular uptake and expulsion of single-walled carbon nanotubes: Single particle tracking and a generic uptake model for nanoparticles. ACS Nano 3, 149–158 (2009).
Xu, A. et al. A physical model for the size-dependent cellular uptake of nanoparticles modified with cationic surfactants. Int. J. Nanomedicine 7, 3547–3554 (2012).
Hickey, J. W., Santos, J. L., Williford, J. M. & Mao, H. Q. Control of polymeric nanoparticle size to improve therapeutic delivery. J. Control. Release 219, 536–547 (2015).
Gupta, A., Eral, H. B., Hatton, T. A. & Doyle, P. S. Nanoemulsions: Formation, properties and applications. Soft Matter 12, 2826–2841 (2016).
Astete, C. E. & Sabliov, C. M. Synthesis and characterization of PLGA nanoparticles. J Biomater Sci Polym Ed 17, 247–289 (2006).
Valencia, P. M., Farokhzad, O. C., Karnik, R. & Langer, R. Microfluidic technologies for accelerating the clinical translation of nanoparticles. Nat. Nanotech. 7, 623–629 (2012).
Mason, T. G. & Bibette, J. Emulsification in viscoelastic media. Phys. Rev. Lett. 77, 3481–3484 (1996).
Bharali, D. J., Sudha, T., Cui, H., Mian, B. M. & Mousa, S. A. Anti-CD24 nano-targeted delivery of docetaxel for the treatment of prostate cancer. Nanomedicine (Lond) 13, 263–273 (2017).
Chu, K. S. et al. Nanoparticle drug loading as a design parameter to improve docetaxel pharmacokinetics and efficacy. Biomaterials 34, 8424–8429 (2013).
Sahoo, S. K., Panyam, J., Prabha, S. & Labhasetwar, V. Residual polyvinyl alcohol associated with poly (D,L-lactide-co-glycolide) nanoparticles affects their physical properties and cellular uptake. J. Control. Release 82, 105–114 (2002).
Abdelwahed, W., Degobert, G., Stainmesse, S. & Fessi, H. Freeze-drying of nanoparticles: Formulation, process and storage considerations. Adv. Drug Del. Rev. 58, 1688–1713 (2006).
Saez, A., Guzman, M., Molpeceres, J. & Aberturas, M. R. Freeze-drying of polycaprolactone and poly(D,L-lactic-glycolic) nanoparticles induce minor particle size changes affecting the oral pharmacokinetics of loaded drugs. Eur. J. Pharm. Biopharm. 50, 379–387 (2000).
Lin, H. Y. et al. Pharmacodynamic modeling of anti-cancer activity of tetraiodothyroacetic acid in a perfused cell culture system. PLoS Comp. Biol. 7, e1001073 (2011).
Li, H. et al. Direct quantitative analysis of a 20 kDa PEGylated human calcitonin gene peptide antagonist in cynomolgus monkey serum using in-source CID and UPLC-MS/MS. J. Am. Soc. Mass Spectrom. 22, 1660–1667 (2011).
Gong, J. et al. Quantitative analysis of polyethylene glycol (PEG) and PEGylated proteins in animal tissues by LC-MS/MS coupled with in-source CID. Anal. Chem. 86, 7642–7649 (2014).
Sparreboom, A. et al. Cremophor EL-mediated alteration of paclitaxel distribution in human blood: Clinical pharmacokinetic implications. Cancer Res. 59, 1454–1457 (1999).
Li, Y., Chen, N., Palmisano, M. & Zhou, S. Pharmacologic sensitivity of paclitaxel to its delivery vehicles drives distinct clinical outcomes of paclitaxel formulations. Mol. Pharmacol. 12, 1308–1317 (2015).
Vasey, P. A. et al. Phase I clinical and pharmacokinetic study of PK1 [N-(2-hydroxypropyl)methacrylamide copolymer doxorubicin]: First member of a new class of chemotherapeutic agents-drug-polymer conjugates. Cancer Research Campaign Phase I/II Committee. Clin. Cancer Res. 5, 83–94 (1999).
Singer, J. W. Paclitaxel poliglumex (XYOTAX, CT-2103): A macromolecular taxane. J. Control. Release 109, 120–126 (2005).
Luque-Michel, E., Imbuluzqueta, E., Sebastian, V. & Blanco-Prieto, M. J. Clinical advances of nanocarrier-based cancer therapy and diagnostics. Expert Opin. Drug Del. 14, 75–92 (2017).
Richter, W. F. & Jacobsen, B. Subcutaneous absorption of biotherapeutics: Knowns and unknowns. Drug Metab. Disposition 42, 1881–1889 (2014).
Li, C. et al. Biodistribution of paclitaxel and poly(l-glutamic acid)-paclitaxel conjugate in mice with ovarian OCa-1 tumor. Cancer Chemother. Pharmacol. 46, 416–422 (2000).
Kumar, R. et al. In vivo biodistribution and clearance studies using multimodal organically modified silica nanoparticles. Acs Nano 4, 699–708 (2010).
Danhier, F., Le Breton, A. & Preat, V. RGD-based strategies to target alpha(v) beta(3) integrin in cancer therapy and diagnosis. Mol. Pharm. 9, 2961–2973 (2012).
Rafiei, P. & Haddadi, A. Docetaxel-loaded PLGA and PLGA-PEG nanoparticles for intravenous application: Pharmacokinetics and biodistribution profile. Int. J. Nanomedicine 12, 935–947 (2017).
Nowak-Sliwinska, P., Segura, T. & Iruela-Arispe, M. L. The chicken chorioallantoic membrane model in biology, medicine and bioengineering. Angiogenesis 17, 779–804 (2014).
Gelderblom, H., Verweij, J., Nooter, K. & Sparreboom, A. Cremophor EL: the drawbacks and advantages of vehicle selection for drug formulation. Eur. J. Cancer 37, 1590–1598 (2001).
Dalwadi, G., Benson, H. A. & Chen, Y. Comparison of diafiltration and tangential flow filtration for purification of nanoparticle suspensions. Pharm. Res. 22, 2152–2162 (2005).
Papadimitriou, S. & Bikiaris, D. Novel self-assembled core–shell nanoparticles based on crystalline amorphous moieties of aliphatic copolyesters for efficient controlled drug release. J. Control. Release 138, 177–184 (2009).
Bridoux, A., Cui, H., Dyskin, E., Yalcin, M. & Mousa, S. A. Semisynthesis and pharmacological activities of tetrac analogs: Angiogenesis modulators. Bioorg. Med. Chem. Lett. 19, 3259–3263 (2009).
Deryugina, E. I. & Quigley, J. P. Chick embryo chorioallantoic membrane models to quantify angiogenesis induced by inflammatory and tumor cells or purified effector molecules, in Methods enzymol. Ch. 2 444, 21–41 (2008).
Marcinkiewicz, C. et al. Obtustatin: A potent selective inhibitor of α1β1 integrin in vitro and angiogenesis in vivo. Cancer Res. 63, 2020–2023 (2003).
Acknowledgements
This work was supported in part by the Pharmaceutical Research Institute (PRI) and in part by a grant from NanoPharmaceuticals LLC (Rensselaer, NY, USA). We thank Scott A. McCallum (Rensselaer Polytechnic Institute) for collecting the NMR data.
Author information
Authors and Affiliations
Contributions
W.L. did the sample preparation from the various biological matrices (plasma and tumor tissues), the PK study and the NMR analysis, wrote the initial drafts of the manuscript and Figures. M.Y. did the in vivo animal study and the CAM growth factors-mediated angiogenesis model study. D.J.B. prepared NDAT and did the confocal fluorescence microscopy imaging. Q.L. established the LC-MS/MS method for the PK analysis and analyzed the data. K.F. did the LC-MS/MS biodistribution analysis. K.A.K. consulted on the NMR data, substantially edited the manuscript, and finalized the Figures. S.A.M. conceived the project, oversaw the research, and analyzed data. All authors edited the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
S.A.M. holds stock in NanoPharmaceuticals LLC, which is developing anticancer drugs. K.A.K. is a paid consultant of NanoPharmaceuticals LLC. All other authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, W., Yalcin, M., Bharali, D.J. et al. RETRACTED ARTICLE: Pharmacokinetics, Biodistribution, and Anti-Angiogenesis Efficacy of Diamino Propane Tetraiodothyroacetic Acid-conjugated Biodegradable Polymeric Nanoparticle. Sci Rep 9, 9006 (2019). https://doi.org/10.1038/s41598-019-44979-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-44979-6
This article is cited by
-
Emerging trends in the nanomedicine applications of functionalized magnetic nanoparticles as novel therapies for acute and chronic diseases
Journal of Nanobiotechnology (2022)
-
Design and In Silico Evaluation of a Novel Cyclic Disulfide-Rich anti-VEGF Peptide as a Potential Antiangiogenic Drug
International Journal of Peptide Research and Therapeutics (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.