Abstract
Postoperative liver dysfunction remains a major concern following hepatic resection. In order to identify patients who are at risk of developing liver dysfunction, indocyanine green (ICG) clearance has been proposed to predict postoperative liver function. All patients who underwent liver resection at the Medical University Vienna, Austria between 2006 and 2015 with preoperative ICG clearance testing (PDR, R15) were analyzed in this study. Postoperative liver dysfunction was analyzed as defined by the International Study Group of Liver Surgery. Overall, 698 patients (male: 394 (56.4%); female: 304 (43.6%)) with a mean age of 61.3 years (SD: 12.9) were included in this study, including 313 minor liver resections (44.8%) and 385 major liver resections (55.2%). One hundred and seven patients developed postoperative liver dysfunction after liver resection (15.3%). Factors associated with liver dysfunction were: male sex (p = 0.043), major liver resection (p < 0.0001), and preoperative ICG clearance (PDR (p = 0.002) and R15 (p < 0.0001)). Notably ICG clearance was significantly associated with liver dysfunction in minor and major liver resections respectively and remained a predictor upon multivariable analysis. An optimal cut-off for preoperative ICG clearance to accurately predict liver dysfunction was PDR < 19.5%/min and R15 > 5.6%. To the best of our knowledge, this is the largest study analyzing the predictive value of preoperative ICG clearance assessment in patients undergoing liver resection. ICG clearance is useful to identify patients at risk of postoperative liver dysfunction.
Similar content being viewed by others
Introduction
Liver resection has become the treatment of choice for a wide range of benign and malignant disease entities. While severe morbidity and mortality has decreased in specialized centers to 20 and 1–3% respectively1,2,3, postoperative liver dysfunction still remains a major concern associated with a significant incidence of liver-related deaths4,5. Even in healthy patients without underlying liver damage, the incidence of hepatic dysfunction following major liver resection is estimated to be approximately 5%6. Known risk factors are the extent of resection, intraoperative blood loss, preoperative chemotherapy but most importantly preoperative liver function7,8,9. In patients with impaired liver function even a small resection can result in a fatal outcome3,10. Thus, a proper patient selection is crucial to exclude patients that may not benefit from hepatectomy.
In order to reduce mortality due to postoperative liver dysfunction, several strategies have been established to identify patients at risk. Indocyanine green (ICG) clearance has been validated as a valuable tool for identifying patients with impaired preoperative liver function11,12. In liver resection ICG clearance has been proposed to define patients, who are at risk of developing postoperative liver dysfunction13,14 or surgical complications15.
Currently, data on the value of preoperative ICG clearance testing to predict the development of postoperative liver dysfunction are scarce and studies are limited to small patient numbers. Moreover, there exists no analysis investigating the predictive value of ICG clearance with respect to the extent of liver resections (minor versus major liver resection). Therefore, we performed an extensive analysis of all patients who underwent liver resection in our center with available preoperative ICG clearance testing results and determined the predictive value regarding postoperative liver dysfunction.
Methods
This is a retrospective study investigating the predictive value of ICG clearance testing with respect to postoperative outcome after liver resection. All patients with available preoperative ICG clearance testing results who underwent elective liver resection of at least one segment between January 2005 and December 2016 were included in this analysis. Patients who underwent non-anatomical resections were excluded from this analysis. Overall 1008 patients underwent hepatic resection within the study period and preoperative ICG clearance testing results were available in 698 patients (63.2%). The type of liver resection was defined as major and minor resections according to the IHPBA Brisbane 2000 nomenclature (≤2 segments: minor; >2 segments: major)16. The study was reviewed and approved by the institutional review board of the Medical University Vienna. All methods were performed in accordance with the relevant guidelines and regulations. Due to the retrospective nature of this study the IRB waived the need to obtain informed consent.
ICG clearance testing
ICG clearance was measured as previously described15. In brief, patients received 0.25 mg/kg ICG intravenously on the day before the liver resection. The plasma disappearance rate (PDR) and the ICG retention rate (R15) were measured by pulse spectrometry with a LiMON device (Pulsion Medical Systems, Munich, Germany). The surgical strategy was not changed upon the results from the ICG clearance testing.
Study endpoints
The primary endpoint was the incidence of liver dysfunction defined by the ISGLS criteria as abnormal bilirubin levels and prothrombin time on or after postoperative day five17. Secondary endpoints were postoperative complications (according to the Clavien-Dindo classification18, lengths of stay and overall survival.
Statistics
Metric data were expressed as means with SD or median with interquartile range (Q1–Q3) and comparison between groups was performed with the Mann-Whitney U test or an unpaired t-test as indicated. Categorical values were compared with Fishers-exact test or a chi-square test. A logistic regression was used to model occurrence of liver dysfunction. Results are presented with odds ratios (OR) and corresponding 95% confidence intervals (95% CI). For this IGG clearance were log-transformed with a basis of 10. Survival probabilities were calculated using a Kaplan-Meier-analysis and group comparison was performed using a log-rank test. Al performed tests are based on a significance level of 0.05. Statistical analysis was performed using GraphPad Prism, version 6 (GraphPad Prism Software®, La Jolla, CA) and SAS (©SAS Institute Inc., Cary, NC, USA).
Results
Patient characteristics
Patient characteristics are show in Table 1. Overall, 698 patients were included in this study. The majority of patients were male (n = 394; 56.4%) and underwent major liver resection (n = 385; 55.2%). The indications for liver resections were predominantly metastases (n = 390; 55.9%) followed by primary liver cancer (31.2%) and benign diseases (12.9%). The median follow-up was 23.3 months (8.9–49.7).
ICG clearance
The median PDR was 21.1%/min (17.7–25.3) and the median R15 was 4.0% (2.0–7.0). There was no significant difference between patients undergoing major or minor resections with respect to preoperative ICG clearance testing. However, patients with hepatocellular carcinoma (HCC) had a significantly impaired ICG clearance compared to patients with other indications for liver resection (metastasis, cholangiocarcinoma or benign disease) (PDR: 19.5%/min (16.4–25) vs. 21.6%/min (18–25.7); p = 0.009) (Suppl. Figure 1a,b). Additionally, patients with HCC a significantly higher fibrosis score in the resected specimen (Suppl. Figure 1c). Of note, there was no significant difference in PDR (p = 0.152) or R15 (p = 0.251) in patients with or without preoperative portal vein embolization (PVE). When analyzing the association between MELD score and ICG clearance we found a significant correlation between PDR (p < 0.0001; r = −0.236) and R15 (p < 0.0001; r = 0.238) (Suppl. Figure 2).
Postoperative liver dysfunction
Overall, 107 patients developed postoperative liver dysfunction after liver resection (15.3%). In these patients, PDR levels were significantly lower compared to patients with normal postoperative liver function (18.8 (16.1–23.1) vs. 21.8 (18–26); p < 0.0001) (Fig. 1a). Conversely, R15 was significantly higher in patients with liver dysfunction (6 (3–8.9) vs. 3.9 (2–6.8); p < 0.0001) (Fig. 1b). Notably, patients with liver dysfunction had a significantly shorter median overall survival compared to patients without liver dysfunction (median 22.9 vs 43.1 months; OR 1.9 (1.4–2.5), p = 0.004) (Fig. 1c).
Factors associated with liver dysfunction in a univariate analysis were: male sex (p = 0.043), type of resection (major, minor liver resection) (p < 0.0001), and preoperative ICG clearance (PDR (p = 0.002) and R15 (p < 0.0001)). In a multivariate analysis male sex (OR 1.76 (95% CI 1.02–3.02); p = 0.043); major resection (OR 8.5 (95% CI 4.3–16.5); p < 0.0001) and a higher ICG clearance (R15, based on a log10 transformation) (OR 2.15 (95% CI 1.05–1.00) p = 0.035) remained with a significantly increased risk for liver dysfunction (Table 2).
Of note, ICG clearance was significantly associated with liver dysfunction in minor and major liver resections, respectively.
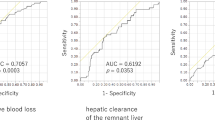
Optimal cut-off values for ICG clearance testing
The best cut-off value for predicting liver dysfunction was calculated by using the Youden-index. An optimal cut-off for preoperative ICG clearance to accurately predict liver dysfunction was a PDR < 19.5%/min and an R15 > 5.6%. Patients with impaired ICG clearance according to these cut-off values were significantly older, were more likely to be male and had less likely a benign cause for liver resection (Table 3). Notably, the grade of fibrosis in the liver was higher compared to patients who did not fulfill these criteria.
Most strikingly, patients with impaired ICG clearance developed two times more likely a postoperative liver dysfunction (Fig. 2) that also resulted in more, and more severe complications and ultimately to a significantly prolonged length of hospitalization. Sensitivity for R15 (>5.6%) was 57% and the specifity was 66.5% resulting in a false positive (FP) rate of 33.5% and a false negative (FN) rate of 43%. For PDR (<19.5%/min) sensitivity was 57.4% and specifity 64.9% (FP: 35.1% FN: 42.5%).
Discussion
To the best of our knowledge, this is the largest study analyzing the predictive value of preoperative ICG clearance assessment in patients undergoing liver resection with respect to postoperative liver dysfunction and clinical outcome. ICG clearance identified patients at risk of postoperative liver dysfunction and significantly worse clinical outcome. Especially in patients undergoing major liver resection, preoperative ICG clearance testing has proven to be clinically relevant given the relatively high incidence of liver dysfunction compared to minor liver resections. Short-term survival was significantly diminished in patients who developed liver dysfunction after liver resection, however long-term outcome was similar to patients without liver dysfunction. These findings are line with previous reports that post-operative complications don’t affect long-term outcome19,20,21. Ultimately, as shown by Padickakudy et al. it might be that serotonin plays a bivotal role in liver regeneration and tumor progression. While patients with high serotonin levels have a lower risk for developing post-operative liver dysfunction, the risk for developing tumor progression is significantly higher compared to patients with low levels of serotonin levels (who are vice versa at higher risk for developing liver dysfunction)22. However, these findings remain to be verified in future and larger clinical studies.
Several approaches are currently pursued to determine preoperative liver function including functional imaging-based analysis23, analysis of intra-platelet serotonin24 or HVPG measuring25,26. In contrast to most of these strategies, ICG clearance testing is cheap, non-invasive and readily available allowing for discrimination between high and low risk patients.
In this study, patients with a worse ICG clearance were generally older, more likely to be male and had a higher grade of liver fibrosis in the resected specimen compared to patients with normal values. These results are in line with several other studies showing a connection between ICG clearance and liver fibrosis11,27. However, in a previous publication Wong et al. reported no difference between R15 rates in patients with or without liver cirrhosis28. This discrepancy might be explained by the smaller patient number and the relatively high proportion of HCC patients compared to our study.
A worse ICG clearance was associated with the development of postoperative liver dysfunction. These results are in accordance with previous smaller studies13,29,30. By using a cut-off of a PDR of <19.5%/min and an R15 > 5.6% a group of patients was identified with a significantly worse outcome. Tomimaru et al. reported that platelet count was superior to ICG clearance testing (R15) in the prediction of postoperative liver dysfunction31. In the present study we didn’t find any association between platelet numbers and the incidence of liver dysfunction, which may be explained by the high proportion of patients with normal liver function.
In a recent study by Zou et al. R15 was significantly associated with liver dysfunction in minor liver resections but not major liver resections32. These results are contrary to our study as ICG clearance was found to be associated with liver dysfunction in both minor and major liver resections. We assume that the conflicting results can be explained by the relatively low incidence of liver dysfunction in minor liver resections in our cohort and by the lower percentage of HCC patients, which are known for a high percentage of liver damage33.
The clinical consequences of an impaired liver function need to be carefully considered when selecting patients for liver resection. On the one hand extensive resection should be avoided, parenchymal sparing surgery and combinations with intraoperative ablations of small lesions instead of major liver resections should be favored34,35. Alternative approaches to prevent postoperative liver dysfunction are the augmentation of the future liver remnant (FLR) by performing portal vein embolization or the ALPPS procedure. Consequently, the question which reference of FLR should be anticipated in patients with poor ICG clearance needs to be evaluated in future clinical studies.
We are aware that there are several limitations of this analysis which are inherent to the retrospective nature of this study. However, a large patient number and a long follow up may outweigh the latter restrictions. The large overlap of PDR and R15 values observed in patients with and without liver dysfunction certainly limits the predictive capacity of ICG clearance testing as a single tool to evaluate a patient before liver resection. Thus, we suggest to combine the results with clinical status, type of hepatectomy and other important factors including established liver damage, the use of neoadjuvant chemotherapy or any other relevant comorbidities to estimate the risk of liver resection.
We further narrowed the tested variables in the uni- and multivariate analysis to clinically relevant and already established factors that may contribute to liver dysfunction, thus, there is the chance that we missed further parameters which are connected to liver dysfunction. However, to prevent a model overfit and to have reproducible results we limited the tested values to the (in our opinion) most important variables.
Conclusions
We conclude that in patients with poor ICG clearance at a cut-off of the PDR of 19.5%/min and an R15 of 5.6% in combination with other risk factors such as male sex, major liver resections should be considered with caution and patients informed accordingly. Besides that, ICG clearance testing is a valuable tool to identify patients at risk of developing postoperative liver dysfunction.
References
Hashimoto, D. A. et al. Is Annual Volume Enough? The Role of Experience and Specialization on Inpatient Mortality After Hepatectomy. Annals of surgery 266, 603–609, https://doi.org/10.1097/SLA.0000000000002377 (2017).
Farges, O. et al. “Surgeons’ intuition” versus “prognostic models”: predicting the risk of liver resections. Annals of surgery 260, 923–928; discussion 928–930, https://doi.org/10.1097/SLA.0000000000000961 (2014).
Clavien, P. A., Petrowsky, H., DeOliveira, M. L. & Graf, R. Strategies for safer liver surgery and partial liver transplantation. N Engl J Med 356, 1545–1559, https://doi.org/10.1056/NEJMra065156 (2007).
Mullen, J. T. et al. Hepatic insufficiency and mortality in 1,059 noncirrhotic patients undergoing major hepatectomy. Journal of the American College of Surgeons 204, 854–862; discussion 862–854, https://doi.org/10.1016/j.jamcollsurg.2006.12.032 (2007).
Skrzypczyk, C. et al. Relevance of the ISGLS definition of posthepatectomy liver failure in early prediction of poor outcome after liver resection: study on 680 hepatectomies. Annals of surgery 260, 865–870; discussion 870, https://doi.org/10.1097/SLA.0000000000000944 (2014).
Rossler, F. et al. Defining Benchmarks for Major Liver Surgery: A multicenter Analysis of 5202 Living Liver Donors. Annals of surgery 264, 492–500, https://doi.org/10.1097/SLA.0000000000001849 (2016).
Fukushima, K. et al. Assessment of ISGLS definition of posthepatectomy liver failure and its effect on outcome in patients with hepatocellular carcinoma. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract 18, 729–736, https://doi.org/10.1007/s11605-013-2423-y (2014).
Allard, M. A. et al. Posthepatectomy portal vein pressure predicts liver failure and mortality after major liver resection on noncirrhotic liver. Annals of surgery 258, 822–829; discussion 829–830, https://doi.org/10.1097/SLA.0b013e3182a64b38 (2013).
Starlinger, P. et al. Perioperative von Willebrand factor dynamics are associated with liver regeneration and predict outcome after liver resection. Hepatology 67, 1516–1530, https://doi.org/10.1002/hep.29651 (2018).
van den Broek, M. A. et al. Liver failure after partial hepatic resection: definition, pathophysiology, risk factors and treatment. Liver international: official journal of the International Association for the Study of the Liver 28, 767–780, https://doi.org/10.1111/j.1478-3231.2008.01777.x (2008).
Zipprich, A. et al. Incorporating indocyanin green clearance into the Model for End Stage Liver Disease (MELD-ICG) improves prognostic accuracy in intermediate to advanced cirrhosis. Gut 59, 963–968, https://doi.org/10.1136/gut.2010.208595 (2010).
Lisotti, A. et al. Indocyanine green retention test as a noninvasive marker of portal hypertension and esophageal varices in compensated liver cirrhosis. Hepatology 59, 643–650, https://doi.org/10.1002/hep.26700 (2014).
de Liguori Carino, N. et al. Perioperative use of the LiMON method of indocyanine green elimination measurement for the prediction and early detection of post-hepatectomy liver failure. European journal of surgical oncology: the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 35, 957–962, https://doi.org/10.1016/j.ejso.2009.02.003 (2009).
Akita, H. et al. Real-time intraoperative assessment of residual liver functional reserve using pulse dye densitometry. World journal of surgery 32, 2668–2674, https://doi.org/10.1007/s00268-008-9752-0 (2008).
Krieger, P. M. et al. Evaluation of chemotherapy-associated liver injury in patients with colorectal cancer liver metastases using indocyanine green clearance testing. Ann Surg Oncol 18, 1644–1650, https://doi.org/10.1245/s10434-010-1494-1 (2011).
Strasberg, S. M. Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg 12, 351–355, https://doi.org/10.1007/s00534-005-0999-7 (2005).
Rahbari, N. N. et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149, 713–724, https://doi.org/10.1016/j.surg.2010.10.001 (2011).
Dindo, D., Demartines, N. & Clavien, P. A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240, 205–213 (2004).
Pang, T. C. et al. Complications following liver resection for colorectal metastases do not impact on longterm outcome. HPB: the official journal of the International Hepato Pancreato Biliary Association 17, 185–193, https://doi.org/10.1111/hpb.12327 (2015).
Khandoga, A. et al. Differential significance of early surgical complications for acute and long-term recurrence-free survival following surgical resection of hepatocellular carcinoma: do comorbidities play a role? European journal of gastroenterology & hepatology 29, 1045–1053, https://doi.org/10.1097/MEG.0000000000000912 (2017).
She, W. H. et al. Short- and long-term impact of reoperation for complications after major hepatectomy for hepatocellular carcinoma. Surgery 160, 1236–1243, https://doi.org/10.1016/j.surg.2016.06.008 (2016).
Padickakudy, R. et al. Bivalent role of intra-platelet serotonin in liver regeneration and tumor recurrence in humans. J Hepatol 67, 1243–1252, https://doi.org/10.1016/j.jhep.2017.08.009 (2017).
Asenbaum, U. et al. Post-hepatectomy liver failure after major hepatic surgery: not only size matters. European radiology, https://doi.org/10.1007/s00330-018-5487-y (2018).
Starlinger, P. et al. The profile of platelet alpha-granule released molecules affects postoperative liver regeneration. Hepatology 63, 1675–1688, https://doi.org/10.1002/hep.28331 (2016).
Stremitzer, S. et al. Value of hepatic venous pressure gradient measurement before liver resection for hepatocellular carcinoma. Br J Surg 98, 1752–1758, https://doi.org/10.1002/bjs.7672 (2011).
Cucchetti, A. et al. Hepatic venous pressure gradient in the preoperative assessment of patients with resectable hepatocellular carcinoma. J Hepatol 64, 79–86, https://doi.org/10.1016/j.jhep.2015.08.025 (2016).
Danin, P. E. et al. Non-invasive Evaluation of NAFLD with Indocyanine Green Clearance Test: a Preliminary Study in Morbidly Obese Patients Undergoing Bariatric Surgery. Obes Surg 28, 735–742, https://doi.org/10.1007/s11695-017-2914-0 (2018).
Wong, J. S. et al. Liver stiffness measurement by transient elastography as a predictor on posthepatectomy outcomes. Annals of surgery 257, 922–928, https://doi.org/10.1097/SLA.0b013e318269d2ec (2013).
Yokoyama, Y. et al. Value of indocyanine green clearance of the future liver remnant in predicting outcome after resection for biliary cancer. Br J Surg 97, 1260–1268, https://doi.org/10.1002/bjs.7084 (2010).
Haegele, S. et al. Perioperative Non-Invasive Indocyanine Green-Clearance Testing to Predict Postoperative Outcome after Liver Resection. PloS one 11, e0165481, https://doi.org/10.1371/journal.pone.0165481 (2016).
Tomimaru, Y. et al. Platelet count is more useful for predicting posthepatectomy liver failure at surgery for hepatocellular carcinoma than indocyanine green clearance test. J Surg Oncol 113, 565–569, https://doi.org/10.1002/jso.24166 (2016).
Zou, H. et al. A Comparative Study of Albumin-Bilirubin Score with Child-Pugh Score, Model for End-Stage Liver Disease Score and Indocyanine Green R15 in Predicting Posthepatectomy Liver Failure for Hepatocellular Carcinoma Patients. Digestive diseases 36, 236–243, https://doi.org/10.1159/000486590 (2018).
Forner, A., Reig, M. & Bruix, J. Hepatocellular carcinoma. Lancet 391, 1301–1314, https://doi.org/10.1016/S0140-6736(18)30010-2 (2018).
Moris, D. et al. Parenchymal-Sparing Versus Anatomic Liver Resection for Colorectal Liver Metastases: a Systematic Review. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract 21, 1076–1085, https://doi.org/10.1007/s11605-017-3397-y (2017).
Desjardin, M. et al. Parenchymal sparing surgery for colorectal liver metastases: The need for a common definition. European journal of surgical oncology: the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 43, 2285–2291, https://doi.org/10.1016/j.ejso.2017.10.209 (2017).
Author information
Authors and Affiliations
Contributions
C.S. wrote the main manuscript, designed the study, performed the study, performed analysis. I.P. performed the study. F.F. performed the study. A.P. performed the study. M.M. performed analysis. S.K. performed the study. U.A. performed the study. P.S. performed the study. S.S. performed the study. M.B. performed the study, designed the study. K.K. designed the study.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schwarz, C., Plass, I., Fitschek, F. et al. The value of indocyanine green clearance assessment to predict postoperative liver dysfunction in patients undergoing liver resection. Sci Rep 9, 8421 (2019). https://doi.org/10.1038/s41598-019-44815-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-44815-x
This article is cited by
-
Predictive Value of Preoperative ICG-R15 Testing in Post-hepatectomy Liver Failure Following Major Liver Resection: Indian Experience
Indian Journal of Surgical Oncology (2024)
-
A novel nomogram predicting overt hepatic encephalopathy after transjugular intrahepatic portosystemic shunt in portal hypertension patients
Scientific Reports (2023)
-
Preoperative planning and intraoperative real-time navigation with indocyanine green fluorescence in robotic liver surgery
Langenbeck's Archives of Surgery (2023)
-
Relative enhancement index can be used to quantify liver function in cirrhotic patients that undergo gadoxetic acid–enhanced MRI
European Radiology (2023)
-
Indocyanine green fluorescence imaging-guided laparoscopic right posterior hepatectomy
Surgical Endoscopy (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.