Abstract
Non-small cell lung cancer (NSCLC) is the most commonly diagnosed lung cancer and is associated with poor prognosis. This study aimed to analyze if serum C-reactive protein (CRP), albumin (Alb), and CRP/Alb ratio could provide prognostic information in patients with NSCLC. 387 patients with primary NSCLC were included in this analysis. Cox proportional hazards regression was used to estimate hazard ratio (HR) and 95% confidence interval (CI) of death with adjustment for some potential confounders. The multivariate regression analyses revealed the statistically significant associations of decreased survival of patients with NSCLC with elevated CRP, decreased Alb, and elevated CRP/Alb ratio. The HRs of mortality were 1.56 (95% CI: 0.80–3.04) and 2.64 (95% CI: 1.35–5.16) for patients in the second and the highest tertiles of CRP (P-trend = 0.003). For albumin, the HR was 0.50 (95% CI: 0.29–0.85) for the normal group. The CRP/Alb ratio strongly predicted the survival of patients in the highest tertile with a fourfold risk of dying compared with those in the lowest tertile (HR = 4.14, 95% CI: 2.15–7.98). The subgroup analysis according to various patient characteristics confirmed these associations. In conclusion, serum CRP, albumin, and CRP/Alb ratio are predictive of survival for Chinese patients with NSCLC.
Similar content being viewed by others
Introduction
Lung cancer is among the most common causes of cancer-related death and is associated with poor treatment outcome1. Non-small cell lung cancer (NSCLC) is the most diagnosed lung cancer. The majority of patients with NSCLC are usually diagnosed at later stages when curative treatments are unavailable2. In this regard, identifying prognostic factors is important because they can contribute to clinical decision making and help individualize treatments for this heterogeneous patient population. A number of prognostic factors in NSCLC have been described. In a systematic review of literature published between 1990 and 2001, Brundage et al.3 found 169 prognostic factors described in 887 studies on predicting the survival of patients with NSCLC. However, most of these factors are not readily available in routine practice.
Systemic inflammation has long been associated with carcinogenesis, tumor proliferation, and dissemination4. Inflammation may also significantly contribute to the prognostic assessment of patients with NSCLC. C-reactive protein (CRP), a routinely measured marker of chronic inflammation, is a reliable biomarker for perioperative management because it can aid in the early detection of surgical site infection5. Furthermore, CRP is an acute reactant protein that is increasingly expression in the presence of infection, trauma, tissue necrosis, tumor, and several types of inflammatory diseases. CRP is an important prognostic indicator in patients with several malignancies, including urological6, pancreatic7, hepatocellular8, and colorectal cancers9. In addition, some studies10,11,12,13,14,15 indicated that elevated serum CRP levels may predict poor survival in patients with NSCLC. However, other studies demonstrated that elevated CRP levels are unrelated to low survival16,17.
Another substantial aspect that is closely linked to the survival of patients with cancer is nutritional status; that is, one third of deaths are caused by malnutrition rather than the cancer itself18. Albumin (Alb) reflects nutritional state and response to inflammation, and is associated with the treatment outcome of NSCLC. Serum albumin is an important prognostic factor for survival of patients with NSCLC19,20,21. Some new indeices based on albumin have been reported for predicting the survival of patients with lung cancer, such indices include prognostic nutritional index22, Glasgow prognostic score23, fibrinogen and albumin score24, albumin and neutrophil combined prognostic grade25, and albumin-to-fibrinogen ratio26. If CRP and albumin can predict the survival of patients with NSCLC, then their combination may better predict the outcome than the use of CRP or albumin alone. CRP/Alb ratio is an independent prognostic factor in patients with pancreatic27, nasopharyngeal28, colorectal29 and esophageal cancers30. CRP/Alb ratio may also predict for disease progression and death in patients with NSCLC31,32,33. However, the evidence is still limited in China, where the incidence and mortality of lung cancer are relatively higher than those in other countries worldwide13,17,33. Hence, we hypothesized that elevated CRP, decreased albumin, and elevated CRP/Alb ratio are associated with poor survival of patients with NSCLC. We prospectively tested the hypothesis by using the Suzhou Lung Cancer Survival (SLCS) study.
Results
Characteristics of patient with NSCLC
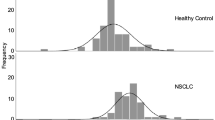
For the 387 patients included in this study, 241 were male and 146 were female, and mean age of these patients were 62 years. A total of 105 deaths occurred during a median follow-up of 19.1 months. Baseline characteristics of the patients by tertiles of CRP level are presented in Table 1. Higher CRP level was associated with male, higher white blood cell count, lower BMI and albumin, ever smoking, later cancer stage and non-resection. Baseline characteristics according to albumin concentration are presented in Table 2. A low albumin concentration was associated with male patients, high CRP and white blood cell count, low BMI, and current smoking habits. The other characteristics of the patients by CRP level and albumin concentration are presented in Supplementary Materials Tables 1 and 2, respectively.
Associations of death with CRP, albumin and CRP/Alb ratio in patients with NSCLC
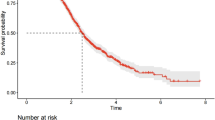
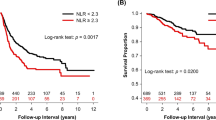
Results of multivariate analysis with adjustments for different confounders are presented in Table 3. An increased CRP concentration was significantly associated with increased risk of death. With the basic adjustment in model 1, compared with the patients in the lowest tertile, the HRs of mortality were 1.61 (95% CI: 0.83–3.10) and 3.32 (95% CI: 1.73–6.40) for those in the second and the highest tertiles (P-trend < 0.001). In addition, compared with patients having low albumin level, the HR of mortality was 0.51 (95% CI: 0.31–0.82) for the group of patients with clinically normal albumin. Further adjustment of other clinical and pathological factors showed similar results for CRP and albumin (model 2). Additional adjustment for white blood cell count and patient history of chronic disease only slightly attenuated the association (model 3: top vs. bottom tertile of CRP HR = 2.64; 95% CI: 1.35–5.16, P-trend = 0.003; albumin ≥35 g/L vs. <35 g/L HR = 0.50; 95% CI: 0.29–0.85). Figures 1 and 2 show that the hazard of mortality for CRP (P < 0.001) and albumin (P < 0.001) were proportional, and patients with elevated CRP or decreased albumin had an increased risk of death.
With the basic adjustment in model 1, the HRs of mortality were 2.30 (95% CI: 1.18–4.49) and 5.16 (95% CI: 2.73–9.78) for patients in the second and highest tertiles of the CRP/Alb ratio (P-trend < 0.001), compared with those in the lowest tertile. Further adjustment of other clinical and pathological factors yielded similar results (model 2). Additional adjustment for white blood cell count and patient history of chronic disease only slightly weakened the association (model 3: HR = 4.14; 95% CI: 2.15–7.98; P-trend < 0.003) (Table 3). Figure 3 shows the proportional hazards by CRP/Alb ratio (P < 0.001).
Associations of death with CRP and albumin in subgroup analysis
The results of subgroup analysis according to various patient characteristics confirmed these associations (Table 4). The increased CRP or decreased albumin level was associated with increased risk of death. Notably, the association between CRP and death varied obviously with age and tumor type, whereas in the stratified analyses of cancer stage and other characteristics, the trend did not have much fluctuation. The association between albumin and mortality varied substantially when stratified by cancer stage and tumor resection history.
Discussion
To the best of our knowledge, this study was first to simultaneously investigate CRP, albumin, and CRP/Alb ratio in relation to the survival of Chinese patient with NSCLC. The results demonstrate that both elevated CRP and decreased albumin levels were significantly associated with poor survival among Chinese patients with NSCLC. Moreover, an increased CRP/Alb ratio was more strongly predictive of mortality. Our findings might suggest that the combination of systemic inflammation and nutritional status affects outcome in patients with NSCLC.
Chronic inflammation, which is an emerging focus of cancer research in recent years, may play a key role in carcinogenesis and tumor progression34. Persistent inflammatory state produces various inflammatory cytokines in response to tissue necrosis and the presence of tumor cells, which has an important effect on cancer progression35. CRP, a typical inflammation marker, is an acute-phase protein produced in the liver. Its main biologic function is to recognize pathogens and damaged cells in the host and to mediate their elimination by recruiting component system and phagocytic cells36. Our findings support the positive associations between CRP and risk of mortality in NSCLC patients37,38. CRP level was classified into two groups in a number of previous studies10,11,12,13,14,15, and only French study39 observed a dose-response association between CRP and mortality with a 1.8-fold higher risk of death among stage I and II but not stage III and IV NSCLC patients when comparing the highest with the lowest group of CRP (>20 mg/L vs. undetectable). In present study of Chinese NSCLC patients, a dose-dependent relationship was also found between CRP and death regardless of cancer stage.
Upon stratification according to tumor type, a strong positive association was observed between the CRP and the mortality of patients with squamous cell carcinoma, whereas the association in patients with adenocarcinoma was relatively weak. Similarly, Siemes et al.40 reported that the increased risk of death was associated with higher CRP for squamous cell carcinoma of lung rather than adenocarcinoma. However, Mssago et al.11 reported that CRP was a poor independent prognostic factor for patients with non-squamous NSCLC. Thus, additional studies are needed to verify whether the relationship between CRP levels and survival among lung cancer patients vary with the histologic subtypes.
Upon examination of the association in terms of cancer stage, we classified the cancer stage into two groups (stage I/II/III and IV) due to the small number of patients with stage I/II NSCLC. CRP was positively associated with mortality in NSCLC patients regardless of cancer stage. Alifano et al.39 showed a CRP level above 20 mg/L was significantly associated with poor survival compared with undetectable CRP in patients with stage I/II unlike in patients with stage III/IV. However, other studies have reported that patients with elevated CRP levels had a poor survival in advanced NSCLC11,13,15. In addition, we found that CRP was positively associated with mortality in patients with tumor resection, which support the positive association between CRP and mortality in patients with resectable NSCLC10,12,14.
Malnutrition commonly occurs in cancer patients, especially in patients with advanced NSCLC who have an important energy expenditure caused by increased tumor metabolism19. Albumin concentration is inversely associated with the magnitude of systemic inflammatory response due to increased catabolism and the downregulation of hepatic synthesis by cytokines tumor necrosis factor alpha41. Using the clinical reference value25 as cutoff, a significant 0.50-fold lower risk of death was observed in patients with normal albumin level. Notably, substantial difference was found in the association between albumin and mortality when stratifying our analyses in terms of cancer stage and tumor resection status. The inverse association was limited to stage IV patients and those without cancer resection. Conversely, Li et al.26 showed that albumin could be a prognostic biomarker regardless of cancer stage, and Miura et al.20 found that preoperative albumin could predict overall survival in 556 resected NSCLC. The potential cause of these differences remains unclear, but the number of patients with early cancer stage or surgical resection may have been too small to detect a significant association in the aforementioned studies in other patient populations.
As expected, we observed a strong positive association between CRP/Alb ratio and risk of mortality in patients with NSCLC. Fairclough et al.42 proposed the concept of CRP/Alb ratio in 2009. Recent studies in other patient population also revealed that the CRP/Alb ratio was predictive of disease progression and mortality in patients with NSCLC31,32,33. A study reported the prognostic effect of CRP/Alb ratio on the survival of patients with advanced NSCLC in Korea31. The other two studies found that CRP/Alb ratio could predict the long-term outcome in Chinese33 and Japanese32 patients with operable NSCLC. Our study did not have specific restriction on cancer stage but also observed a strong positive association between CRP/Alb ratio and the mortality of patients with NSCLC.
The strengths of our study include its overall large sample size, comprehensive collection of various patient characteristics to allow careful adjustment for potential confounders. However, a small number of patients were involved in several subgroup analyses, which limited the statistical power. Lung cancer has long relied on testing for the molecular biomarkers, such as epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK)43. In the present study, we did not collect the samples to determine the driver gene mutation. However, a meta-analysis demonstrated that there were significantly increased odds of presenting the EGFR and ALK-EML4 mutations in adenocarcinomas compared to NSCLC44. Our ongoing patient enrollment could provide an additional opportunity to specifically investigate some of these associations in greater depth.
In conclusion, our study shows that increased CRP, decreased Alb level, and increased CRP/Alb ratio were associated with poor survival among Chinese patients with NSCLC.
Materials and Methods
Participant identification
The SLCS study, which was initiated in 2015, is an ongoing patient cohort for exploring long-term predictors of lung cancer survival among patients living in Southeastern China (Suzhou). This study mainly emphasizes on the potential influence of nutritional status and environmental pollutants on lung cancer survival. Patients who were diagnosed with primary lung cancer and who were 18 years old or older were included in the study. Although our inclusion criteria did not have other specific restrictions, such as status and type of medical treatments, data were carefully collected during the enrollment period and their effects on any examined association were explored throughout the analysis. The patient enrollment was started in January 2016, and 455 patients diagnosed with primary lung cancer have been included as of April 2018. Considering the small number of small cell lung cancer cases (n = 49), our analysis only included patients with NSCLC (n = 406). This study was approved by the Research Ethics Committee of Soochow University (Approval No. ESCU-2015-0002), and written informed consent was obtained from each patient. We also confirmed that all methods were performed in accordance with the relevant guidelines and regulations.
Data and blood sample collection
In-person interviews were conducted using a structured questionnaire during recruitment to collect patients’ characteristics on demographics and habitual lifestyle, including smoking, alcohol drinking, and physical activity. Based on the collected data, smoking status was grouped into three categories (never, former, or current smoker), and drinking status was classified into two groups (yes or no). Former smokers were defined as patients who had smoked but already quitted for at least one year, and current smokers were determined as those who are still smoking at the time of investigation or those who gave up smoking for less than one year. Patients who are drinking alcohol on average of at least once a week within the six previous months were considered as patients with drinking habit (yes). Field measurements were implemented to obtain patient anthropometrics, including height, weight, and waist and hip circumstance. In addition to the patient interviews, their medical records were also reviewed to collect their clinical information, including the pathological type, cancer stage, and lung cancer treatments.
Blood biochemistry and blood cell analysis were also obtained from their test report during enrollment, including liver function, renal function and other blood indicators. Furthermore, 5 mL whole blood was drawn from the antecubital veins of each patient and then transferred into a tube with ethylenediaminetetraacetic acid during recruitment after an overnight fasting. The plasma was obtained through centrifugation (3,000 rpm at 25 °C for 10 min) within 2 h after sample collection. All samples were numbered and stored at −80 °C until further analysis.
Measurements of biomarkers
Serum CRP, albumin, and white blood cell count were all extracted from the patient test report from two hospitals. CRP, albumin and white blood cell count were all conducted in laboratories of both institutions as routine examinations for each patient. Among the three indicators, the serum CRP level was measured through nephelometry by using a fully automatic Siemens ADVIA 2400 Biochemical Analyzer System (Siemens Healthcare Diagnosis Inc, NY, USA). The lower detection limit was 1 mg/L. The serum albumin concentration was measured through bromocresol green staining method by using an Olympus 5400 Automatic Biochemical Analyzer (Olympus Corporation, Tokyo, Japan). Furthermore, a combination of electrical impedance, radiofrequency and cytochemistry was used to determine the blood count by using the Sysmex/XE-2100 blood cell analysis line (Sysmex Corporation, Kobe, Japan).
Patient follow-up
This study primarily determined the overall survival, which was calculated from the date of baseline questionnaire to the date of death. Follow-up was initiated from the date of patient enrollment until May 8, 2018 or until patient death from any cause. The long-term survival of patients was assessed every 6 months. Data were collected from at least one of the following sources: (1) inpatient or outpatient records from the hospital; (2) local death registration system; and (3) patient or family telephonic contact. A small proportion of patients (4.7%, n = 19) were lost during the follow-up and were excluded from the present analysis. A total of 387 patients with NSCLC were included in the present analysis.
Statistical analysis
Continuous variables were expressed as the means with the standard deviation, and were compared using one-way ANOVA. The Chi-Square or Mann-Whitney U test was used to compare the categorical variables, which was presented as the number and percentage of patients. Albumin was grouped according to the clinical standard threshold25. The CRP concentration and CRP/Alb ratio were classified into tertiles.
Survival analysis was performed using the Kaplan-Meier method, and the differences were assessed using the Log-Rank test. Hazard ratios (HR) and 95% confidence intervals (CI) of NSCLC death were estimated using the Cox proportional hazards regression model. Three models with different covariates were constructed to account for potential confounders. The first model was adjusted for demographic characteristics including age at baseline interview (years), sex, body mass index (kg/m2), family history of cancer (yes or no), patient history of chronic obstructive pulmonary disease (yes or no), smoking status (never, former, or current smoker), and drinking habit (yes or no). The second model included the variables in the model 1 and was additionally adjusted for clinical information including tumor type (adenocarcinoma, squamous cell carcinoma, or other tumor types), cancer stage (I/II or III/IV), and treatment (with tumor resection, without resection but with other therapies such as chemotherapy and radiotherapy, without either resection, or other therapies). Considering the impact of white blood cell count on the CRP45 and the influence of chronic liver disease on the albumin46, analyses were further adjusted for the history of chronic liver disease (yes or no) and white blood cell count (continuous) in the third model.
For the analyses of CRP and CRP/Alb ratio, P values for the linear trends were calculated by fitting the median values of CRP and CRP/Alb ratio as continuous variables. We also constructed stratified analyses by age (<60 years vs. ≥60 years), sex, smoking status (never smoker vs. ever smoker), tumor type (adenocarcinoma vs. squamous cell carcinoma), cancer stage (I to III vs. IV), and tumor resection (yes vs. no) to assess whether the examined associations varied substantially according to these characteristics. All statistical analyses were performed using the SPSS 19.0 software. All tests were two-sided, and statistically significance was considered at P < 0.05.
References
Ferlay, J. et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. International journal of cancer 136, E359–386, https://doi.org/10.1002/ijc.29210 (2015).
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2015. CA: a cancer journal for clinicians 65, 5–29, https://doi.org/10.3322/caac.21254 (2015).
Brundage, M. D., Davies, D. & Mackillop, W. J. Prognostic factors in non-small cell lung cancer: a decade of progress. Chest 122, 1037–1057 (2002).
Diakos, C. I., Charles, K. A., McMillan, D. C. & Clarke, S. J. Cancer-related inflammation and treatment effectiveness. The Lancet. Oncology 15, e493–503, https://doi.org/10.1016/s1470-2045(14)70263-3 (2014).
Watt, D. G., Horgan, P. G. & McMillan, D. C. Routine clinical markers of the magnitude of the systemic inflammatory response after elective operation: a systematic review. Surgery 157, 362–380, https://doi.org/10.1016/j.surg.2014.09.009 (2015).
Zhou, L. et al. Prognostic Role of C-Reactive Protein In Urological Cancers: A Meta-Analysis. Scientific reports 5, 12733, https://doi.org/10.1038/srep12733 (2015).
Szkandera, J. et al. Validation of C-reactive protein levels as a prognostic indicator for survival in a large cohort of pancreatic cancer patients. British journal of cancer 110, 183–188, https://doi.org/10.1038/bjc.2013.701 (2014).
Zheng, Z. et al. Prognostic role of C-reactive protein in hepatocellular carcinoma: a systematic review and meta-analysis. International journal of medical sciences 10, 653–664, https://doi.org/10.7150/ijms.6050 (2013).
Kwon, K. A. et al. Clinical significance of preoperative serum vascular endothelial growth factor, interleukin-6, and C-reactive protein level in colorectal cancer. BMC cancer 10, 203, https://doi.org/10.1186/1471-2407-10-203 (2010).
Hara, M. et al. Preoperative serum C-reactive protein level in non-small cell lung cancer. Anticancer research 27, 3001–3004 (2007).
Masago, K. et al. Clinical significance of pretreatment C-reactive protein in patients with advanced nonsquamous, non-small cell lung cancer who received gefitinib. Oncology 79, 355–362, https://doi.org/10.1159/000323486 (2010).
O’Dowd, C., McRae, L. A., McMillan, D. C., Kirk, A. & Milroy, R. Elevated preoperative C-reactive protein predicts poor cancer specific survival in patients undergoing resection for non-small cell lung cancer. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer 5, 988–992, https://doi.org/10.1097/JTO.0b013e3181da78f9 (2010).
Ni, X. F. et al. Elevated serum C-reactive protein, carcinoembryonic antigen and N2 disease are poor prognostic indicators in non-small cell lung cancer. Asia-Pacific journal of clinical oncology 11, e22–30, https://doi.org/10.1111/ajco.12091 (2015).
Shinohara, S. et al. Prognostic Impact of Postoperative C-reactive Protein for Non-small Cell Lung Cancer Following Lobectomy. Anticancer research 38, 3193–3198, https://doi.org/10.21873/anticanres.12584 (2018).
Koch, A., Fohlin, H. & Sorenson, S. Prognostic significance of C-reactive protein and smoking in patients with advanced non-small cell lung cancer treated with first-line palliative chemotherapy. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer 4, 326–332, https://doi.org/10.1097/JTO.0b013e31819578c8 (2009).
Gioulbasanis, I. et al. Mini Nutritional Assessment (MNA) and biochemical markers of cachexia in metastatic lung cancer patients: interrelations and associations with prognosis. Lung cancer (Amsterdam, Netherlands) 74, 516–520, https://doi.org/10.1016/j.lungcan.2011.05.009 (2011).
Chi, P. D. et al. High-density lipoprotein cholesterol is a favorable prognostic factor and negatively correlated with C-reactive protein level in non-small cell lung carcinoma. PLoS One 9, e91080, https://doi.org/10.1371/journal.pone.0091080 (2014).
Garcia-Luna, P. P., Parejo Campos, J. & Pereira Cunill, J. L. Causes and impact of hyponutrition and cachexia in the oncologic patient. Nutricion hospitalaria 21(Suppl 3), 10–16 (2006).
Fiala, O. et al. Serum albumin is a strong predictor of survival in patients with advanced-stage non-small cell lung cancer treated with erlotinib. Neoplasma 63, 471–476, https://doi.org/10.4149/318_151001n512 (2016).
Miura, K. et al. Clinical significance of preoperative serum albumin level for prognosis in surgically resected patients with non-small cell lung cancer: Comparative study of normal lung, emphysema, and pulmonary fibrosis. Lung cancer (Amsterdam, Netherlands) 111, 88–95, https://doi.org/10.1016/j.lungcan.2017.07.003 (2017).
Ikeda, S. et al. Serum albumin level as a potential marker for deciding chemotherapy or best supportive care in elderly, advanced non-small cell lung cancer patients with poor performance status. BMC cancer 17, 797, https://doi.org/10.1186/s12885-017-3814-3 (2017).
Shoji, F. et al. Predictive impact for postoperative recurrence using the preoperative prognostic nutritional index in pathological stage I non-small cell lung cancer. Lung cancer (Amsterdam, Netherlands) 98, 15–21, https://doi.org/10.1016/j.lungcan.2016.05.010 (2016).
Yotsukura, M. et al. Value of the Glasgow Prognostic Score as a Prognostic Factor in Resectable Non-Small Cell Lung Cancer. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer 11, 1311–1318, https://doi.org/10.1016/j.jtho.2016.04.029 (2016).
Chen, P. et al. Plasma fibrinogen and serum albumin levels (FA score) act as a promising prognostic indicator in non-small cell lung cancer. OncoTargets and therapy 10, 3107–3118, https://doi.org/10.2147/ott.s138854 (2017).
Sun, H. et al. Albumin and Neutrophil Combined Prognostic Grade as a New Prognostic Factor in Non-Small Cell Lung Cancer: Results from a Large Consecutive Cohort. PloS one 10, e0144663, https://doi.org/10.1371/journal.pone.0144663 (2015).
Li, S. Q. et al. Albumin-to-fibrinogen ratio as a promising biomarker to predict clinical outcome of non-small cell lung cancer individuals. Cancer medicine 7, 1221–1231, https://doi.org/10.1002/cam4.1428 (2018).
Liu, Z. et al. Prognostic Value of the CRP/Alb Ratio, a Novel Inflammation-Based Score in Pancreatic Cancer. Annals of surgical oncology 24, 561–568, https://doi.org/10.1245/s10434-016-5579-3 (2017).
Zhang, Y. et al. Exploration and Validation of C-Reactive Protein/Albumin Ratio as a Novel Inflammation-Based Prognostic Marker in Nasopharyngeal Carcinoma. J Cancer 7, 1406–1412, https://doi.org/10.7150/jca.15401 (2016).
Shibutani, M. et al. Prognostic Significance of the Preoperative Ratio of C-Reactive Protein to Albumin in Patients with Colorectal Cancer. Anticancer research 36, 995–1001 (2016).
Xu, X. L., Yu, H. Q., Hu, W., Song, Q. & Mao, W. M. A Novel Inflammation-Based Prognostic Score, the C-Reactive Protein/Albumin Ratio Predicts the Prognosis of Patients with Operable Esophageal Squamous Cell Carcinoma. PLoS One 10, e0138657, https://doi.org/10.1371/journal.pone.0138657 (2015).
Koh, Y. W. & Lee, H. W. Prognostic impact of C-reactive protein/albumin ratio on the overall survival of patients with advanced nonsmall cell lung cancers receiving palliative chemotherapy. Medicine 96, e6848, https://doi.org/10.1097/md.0000000000006848 (2017).
Miyazaki, T. et al. Ratio of C-reactive protein to albumin is a prognostic factor for operable non-small-cell lung cancer in elderly patients. Surgery today 47, 836–843, https://doi.org/10.1007/s00595-016-1448-8 (2017).
Zhang, F. et al. The C-reactive protein/albumin ratio predicts long-term outcomes of patients with operable non-small cell lung cancer. Oncotarget 8, 8835–8842, https://doi.org/10.18632/oncotarget.13053 (2017).
Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell 144, 646–674, https://doi.org/10.1016/j.cell.2011.02.013 (2011).
Groblewska, M., Mroczko, B., Sosnowska, D. & Szmitkowski, M. Interleukin 6 and C-reactive protein in esophageal cancer. Clinica chimica acta; international journal of clinical chemistry 413, 1583–1590, https://doi.org/10.1016/j.cca.2012.05.009 (2012).
Volanakis, J. E. Human C-reactive protein: expression, structure, and function. Molecular immunology 38, 189–197 (2001).
Jin, Y. et al. Prognostic value of circulating C-reactive protein levels in patients with non-small cell lung cancer: a systematic review with meta-analysis. Journal of cancer research and therapeutics 10(Suppl), C160–166, https://doi.org/10.4103/0973-1482.145854 (2014).
Jing, X. et al. Association between serum C-reactive protein value and prognosis of patients with non-small cell lung cancer: a meta-analysis. International journal of clinical and experimental medicine 8, 10633–10639 (2015).
Alifano, M. et al. Preresection serum C-reactive protein measurement and survival among patients with resectable non-small cell lung cancer. The Journal of thoracic and cardiovascular surgery 142, 1161–1167, https://doi.org/10.1016/j.jtcvs.2011.07.021 (2011).
Siemes, C. et al. C-reactive protein levels, variation in the C-reactive protein gene, and cancer risk: the Rotterdam Study. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 24, 5216–5222, https://doi.org/10.1200/jco.2006.07.1381 (2006).
Chojkier, M. Inhibition of albumin synthesis in chronic diseases: molecular mechanisms. Journal of clinical gastroenterology 39, S143–146 (2005).
Fairclough, E., Cairns, E., Hamilton, J. & Kelly, C. Evaluation of a modified early warning system for acute medical admissions and comparison with C-reactive protein/albumin ratio as a predictor of patient outcome. Clinical medicine (London, England) 9, 30–33 (2009).
Iyer, S. et al. The future of lung cancer therapy: Striding beyond conventional EGFR and ALK treatments. Mol Clin Oncol 10, 469–475, https://doi.org/10.3892/mco.2019.1811 (2019).
Chapman, A. M., Sun, K. Y., Ruestow, P., Cowan, D. M. & Madl, A. K. Lung cancer mutation profile of EGFR, ALK, and KRAS: Meta-analysis and comparison of never and ever smokers. Lung cancer (Amsterdam, Netherlands) 102, 122–134, https://doi.org/10.1016/j.lungcan.2016.10.010 (2016).
Tanizaki, J. et al. Peripheral Blood Biomarkers Associated with Clinical Outcome in Non-Small Cell Lung Cancer Patients Treated with Nivolumab. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer 13, 97–105, https://doi.org/10.1016/j.jtho.2017.10.030 (2018).
Spinella, R., Sawhney, R. & Jalan, R. Albumin in chronic liver disease: structure, functions and therapeutic implications. Hepatology international 10, 124–132, https://doi.org/10.1007/s12072-015-9665-6 (2016).
Acknowledgements
This work was supported by the National Key R&D Program of China (2017YFC1310700, 2017YFC1310701), the National Natural Science Foundation of China (No. 81472974, 81673101) and the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD).
Author information
Authors and Affiliations
Contributions
Qin L.Q., Xu J.Y. and Chen G.C. conceived and designed the study. Yang J.R. and Qin L.Q. wrote the manuscript. Yang J.R. and Chen G.C. performed the statistical analysis. Xu J.Y., Li D.P. and Zhang Y.S. coordinated the research. Yang J.R., Yu N., Yang J., Zeng D.X. and Gu M.J. conducted questionnaire survey and sample collection. Yang J.R. organized the questionnaire and sample information. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, JR., Xu, JY., Chen, GC. et al. Post-diagnostic C-reactive protein and albumin predict survival in Chinese patients with non-small cell lung cancer: a prospective cohort study. Sci Rep 9, 8143 (2019). https://doi.org/10.1038/s41598-019-44653-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-44653-x
This article is cited by
-
The effect of albumin and hemoglobin levels on the prognosis of early-stage cervical cancer: a prospective, single-center–based cohort study
BMC Women's Health (2023)
-
Impact of serum albumin concentration and neutrophil–lymphocyte ratio score on gastric cancer prognosis
Langenbeck's Archives of Surgery (2023)
-
The implications of clinical risk factors, CAR index, and compositional changes of immune cells on hyperprogressive disease in non-small cell lung cancer patients receiving immunotherapy
BMC Cancer (2021)
-
Albumin-to-alkaline phosphatase ratio serves as a prognostic indicator in unresectable pancreatic ductal adenocarcinoma: a propensity score matching analysis
BMC Cancer (2020)
-
Prognostic impact of C-reactive protein-albumin ratio for the lethality in castration-resistant prostate cancer
Medical Oncology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.