Abstract
In Myanmar, Rifampicin resistant tuberculosis (RR-TB, a proxy for Multi-drug resistant TB) case detection is very low. Our study objectives were to assess the proportion of eligible TB patients who had not undergone RR-TB testing (Xpert-MTB/Rif tests) in Bago Region, Myanmar and to understand the reasons and solutions for non-testing. We conducted a mixed-methods study involving analysis of routinely collected programme data followed by key informant interviews (KIIs) with 32 health care providers. From October 2016 to March 2017, of the 2,331 eligible patients, 1,066 (46%) had not undergone Xpert-MTB/Rif testing. Patients from townships without Xpert-MTB/Rif testing facilities, new TB patients, patients whose HIV status was negative or unknown and extra pulmonary TB patients were less likely to undergo Xpert-MTB/Rif testing. From the health care providers’ perspective, the most common reasons for non-testing were: (a) lack of awareness of the eligibility criteria; (b) difficulties in collecting sputum and transportation from eligible patients to the testing sites. We conclude that nearly half of eligible patients were not tested for RR-TB. Training of health care providers about the latest eligibility criteria and improvement in sputum collection and transportation systems particularly for townships without Xpert-MTB/Rif testing facilities are required to improve RR-TB testing.
Similar content being viewed by others
Introduction
Multi-drug resistant tuberculosis (MDR-TB), i.e., infection with Mycobacterium tuberculosis that is resistant to the two most potent anti-TB drugs namely, rifampicin and isoniazid, is an important challenge for TB control worldwide. Early detection and prompt treatment of patients with MDR-TB is crucial to reduce morbidity, mortality and transmission in the community. However, globally in 2017 only 29% of an estimated 558,000 incident MDR-TB patients were detected and of those detected, 87% were initiated on treatment1. This indicates that the national tuberculosis programmes in high TB burden countries encounter challenges in the diagnosis and treatment initiation of MDR-TB2.
Operational challenges in diagnosing and initiating patients on MDR-TB treatment are reflected in two attritions, namely ‘pre-diagnostic’ and ‘pre-treatment attrition’3. “Pre-diagnostic attrition” indicates failure to identify and test eligible patients with presumptive MDR-TB with MDR-TB laboratory tests, and “pre-treatment attrition” reflects failure to initiate diagnosed MDR-TB patients on MDR-TB treatment. It is recommended that the TB programmes in all high burden countries monitor such attritions, identify the reasons and undertake corrective measures to improve care provided to these patients4,5.
Myanmar is one of the 30 high MDR-TB burden countries with an estimated annual incidence of 13,000 MDR-TB cases (incidence rate = 25/100,000 population) in 20162. The prevalence of MDR-TB among new and retreatment TB cases is about 5% and 27% respectively, which is higher than global average of 4.1% and 19% in 20162. Services for MDR-TB diagnosis and treatment were initiated under the National TB Programme (NTP) in 2009 as a “DOT-Plus” pilot project in 10 townships, which was later renamed as “Programmatic Management of Drug-resistant TB” (PMDT) in 20116. During the initial years, the diagnosis of MDR-TB was based only on results of sputum culture and drug sensitivity testing. This could be done only in two laboratories (located at Yangon and Mandalay), and therefore due to limited access and long turnaround time to obtain results, anecdotal evidence indicates that the number of MDR-TB patients diagnosed and initiated on treatment was low. With the introduction and scale up of rapid diagnostic tests [Xpert MTB/Rif ® tests, called ‘GXP tests’ henceforth] and with this test providing results on the presence of Mycobacterium Tuberculosis Complex and rifampicin resistance (RR-TB, rifampicin resistant TB) within 2 hours with relatively high sensitivity and specificity7, it was expected that the situation would improve. By the end of 2017, 71 GXP machines were available at district TB centers in various parts of the country. For all practical purposes, in order to simplify the case management under routine programmatic conditions, RR-TB patients are considered as proxy for having MDR-TB in Myanmar.
Though GXP testing sites have increased in numbers, diagnosing all RR-TB patients are still a major challenge for the NTP. As per the National Strategic Plan (NSP) 2016–2020, the Myanmar NTP had set a target of notifying 4,816 RR-TB cases in 20168. However, in 2016 only 3,213 RR-TB cases were notified —a short fall of 1,603 (33%) cases (2016 NTP data). The reasons for the shortfall were not completely known and anecdotal evidence indicated that the reasons vary across different states and regions of the country. A previous study from Yangon and Mandalay regions showed high pre-treatment attrition rates (30%)9. But there have not been any studies describing the magnitude and reasons for pre-diagnosis attrition in Myanmar (definitions of pre-treatment and pre-diagnosis attrition are mentioned in the second paragraph). Recently, in order to accelerate the RR-TB case finding in the country, the NTP has set targets for testing 70% and 75% of all eligible presumptive RR-TB cases in 2016 and 2017 respectively by GXP tests.
Bago Region in Myanmar has a population of 5 million (~10% of Myanmar’s population)10. If the national RR-TB prevalence estimates are applied to the TB patients diagnosed in Bago region, in 2016, about 550 RR-TB cases (177 RR-TB patients among 3,552 new smear positive TB cases and 372 RR TB patients among 1,373 retreated TB cases) should have been detected. However, only 179 (33%) of the estimated 550 RR-TB patients were detected in 2016 indicating that either the RR-TB prevalence is low in the region or that the TB programme is not able to diagnose RR-TB cases. [2016 Bago Region TB data, personal communication]
We hypothesized that low RR-TB detection in Bago region is more likely due to pre-diagnosis attrition. This is because, the population in Bago Region is sparsely distributed, is predominantly rural in nature and the numbers of GXP testing machines/facilities are few. Therefore, we undertook an operational research study to understand the magnitude and reasons for pre-diagnosis attrition.
The specific objectives were as follows. Among TB patients enrolled for first-line anti-TB treatment under the NTP in Bago Region between October 2016–March 2017: first, to assess the number (and proportion) who were presumptive RR-TB patients and eligible for GXP testing, and of those eligible, to determine the number (and proportion) who underwent GXP testing and their demographic, clinical characteristics; second, in those who had undergone GXP testing, to assess the duration between date of eligibility for GXP testing and date of GXP testing; and third, to understand the health provider perspectives on the reasons for failure to identify and test eligible TB patients with GXP tests.
Methods
Study design
This was a sequential explanatory mixed methods study beginning with the quantitative phase and then the qualitative phase, to explain or enhance the quantitative results11. For the first two objectives (quantitative phase) we used a retrospective cohort study design and involved secondary analysis of data routinely collected by NTP. For the third objective, we used a descriptive study design (qualitative phase) and conducted key informant interviews (KIIs) with 28 township TB coordinators and laboratory technicians of 4 GXP sites in Bago Region.
Setting
Myanmar is a low middle income South-East Asian country with population of ~51 million. There are 74 districts (330 townships)10. About 70% of the population lives in rural areas. Health coverage of rural population is predominantly provided through primary health care facilities.
The Myanmar NTP is managed by a team lead by a Program Manager at the central level in Nay Pyi Taw and TB Officers at regional and district levels. TB diagnostic and treatment services are integrated into the public health care system. Each township in the country has a township TB coordinator who is primarily responsible for coordinating all the activities of NTP (diagnosis, treatment, recording and reporting, drug management etc.). TB cases are predominantly diagnosed by sputum smear microscopy and chest radiography. All detected TB cases are classified using standard WHO recommended case definitions and enrolled in the “paper based TB registers” of the respective township TB center for TB treatment as per NTP guidelines12. Prior to initiating the patients on TB treatment, certain groups of TB patients are classified as “presumptive RR-TB patients” and these patients are eligible to undergo GXP tests upfront to detect rifampicin resistance [GXP test is mainly used for the purpose of RR-TB diagnosis]. The 2016 NTP criteria for classifying TB patients as presumptive RR-TB patients are given in Table 1. Patients with rifampicin resistance (with the GXP test), are enrolled for second line drug treatment (also known as MDR-TB treatment) as per the national PMDT guidelines6.
There are two more sub-groups of patients who are not included in township TB register and are also eligible for GXP testing. They are: a) HIV seropositive patients with TB symptoms; and b) certain cases to be considered individually by MDR-TB committee (e.g., persons with TB symptoms with past history of TB treatment)6. However, no line list of these “presumptive RR-TB patients” are maintained anywhere and therefore, our study does not include these patients.
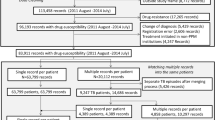
In Bago Region, there are 28 township health facilities that diagnose and treat TB patients. Each of these 28 townships has a township TB coordinator. It is the primary responsibility of the township TB coordinators and the laboratory technicians to identify patients with presumptive RR-TB and ensure that they undergo GXP testing. GXP testing facilities are available in 4 townships (Bago, Pyay, Taungoo and Taryarwadi) and the sputum samples from non-GXP townships (n = 24) are transported to these four GXP sites for GXP testing. The process followed for GXP testing in Bago region is shown in Fig. 1. In 2016, in townships without GXP testing facilities, the sputum samples were collected and transported to the designated GXP facilities twice a month by township TB coordinators and in 2017, it was transported more frequently on a weekly basis.
Study population
For the quantitative part of the study, all TB patients enrolled for first-line anti-TB treatment under the NTP between October 2016 and March 2017 in the 28 townships of the Bago Region were included. For the qualitative part of the study, the township TB coordinators (employed and in-place in January 2018) in all 28 townships and TB laboratory technicians from the 4 GXP sites were included.
Data collection and data validation
For the quantitative part of the study, for each TB patient enrolled in the 28 township TB registers, we applied the criteria given in Table 1 to identify presumptive MDR-TB patients (based on the information recorded in the TB registers). For each patient, their status of GXP test eligibility was assessed at two time points: First, at enrollment and second, at the end of intensive phase of treatment (to identify non-converters). All patients who fulfilled one or more criteria were line listed and this list provided the number of presumptive MDR-TB patients eligible for GXP testing. In order to assess what proportion were tested we looked at the corresponding columns in the TB registers, GXP registers of the four GXP sites and the township TB coordinator’s list (if it was maintained). If there was no information on GXP testing from these three sources, then we classified such patients as “GXP not tested”. For each patient tested by GXP, we assessed whether they were tested before or after initiation of TB treatment.
The data collected from the TB registers included date of enrolment, Township TB number, name of patient, age, gender, name of township, type of TB patients (new/relapse/failure/ loss to follow up/other/transfer in), HIV status (negative/positive/unknown), initial smear result (negative/positive), 2/3 month follow up smear result (negative/positive), GXP number and result.
Details of all eligible presumptive RR-TB patients from paper-based records from 28 townships were entered in a structured data collection format created in EpiData (version 3.1, The EpiData Association, Odense, Denmark). Thereafter, the electronic database was imported to STATA (version 14.2, StataCorp, College Station, Texas, USA) and analyzed.
For the qualitative part of the study, we conducted key informant interviews (KII) with 28 Township TB coordinators and 4 laboratory technicians of the GXP testing sites [total n = 32] without any exclusion. The interview guide (for the qualitative study) was developed based on the preliminary findings for the quantitative study which showed considerable gaps in testing. All interviews were conducted face-to-face and audio recorded. The KII were conducted by one of the two co-authors (KWYK and KTS) with technical guidance of another co-author (Saw Saw). All three co-authors are experienced and trained in TB and qualitative research methods. The interviewers (KWYK and KTS) were not part of NTP but working as Operational Research Fellows for The Union and Department of Medical Research in Myanmar. The KII interview guides are given in Appendix 1.
Data analysis
Quantitative part
Data are summarized in numbers (and proportions) for categorical variables and medians (and interquartile ranges) for continuous variables.
Multivariable log binomial models (multivariable Poisson regression models with robust standard error estimates if log binomial models failed to attain convergence) were used to assess the association between measured demographic and clinical characteristics with lack of GXP testing in those eligible. The association has been described in relative risks and adjusted relative risks with its 95% CI. We did not exclude patients with missing values. Instead, we assigned a value for missing data in each variable and estimated the relative risk and adjusted relative risk for this missing value. For statistical significance we have used a p-value < 0.05.
Quantitative part
For the data collected through KIIs, we removed the identifying details of participants and their audio files were anonymized. All KII interviews were conducted in Burmese language and transcribed verbatim in Burmese. We did a content analysis. Two coders (KWYK and KTS) independently reviewed all transcripts and developed codes manually. After the codes were developed, emerging themes were identified in consultation with two other co-authors (TO, Saw Saw)—who also had access to all transcripts. The themes are presented as a list of reasons for attrition and a list of possible solutions to address this problem (along with the supporting ‘quotes’). The qualitative data analysis was initially conducted in Burmese and the final results were translated into English. Forward and backward translations of the results were done to ensure accuracy of the translation. The qualitative data analysis was done after the end of all the interviews and we did not check for saturation in-between. We have integrated the results of quantitative and qualitative part of the study through narration13.
Adherence to guidelines
We have adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines and ‘Consolidated Criteria for Reporting Qualitative Research (COREQ) in conducting and reporting the study14,15.
Ethical approval
We obtained permission to conduct the study from the Myanmar NTP. We obtained ethics approval from the Department of Medical Research, Myanmar and Ethics Advisory Group of International Union Against Tuberculosis and Lung Disease (The Union), Paris. Informed consent was obtained from the study participants for the qualitative part of our study. We adhered to the approved methods while conducting the study.
Results
Quantitative part
Eligible for GXP testing and GXP testing status
A total of 5,658 TB patients were enrolled for TB treatment between October 2016 and March 2017 in Bago Region. Of the six eligibility criteria (shown in Table 1), none of the patients had history of contact with an MDR-TB patient or diabetes mellitus status recorded. Therefore, we were able to assess for GXP eligibility based on four criteria. With this, we found that 2,331 (41%) patients were eligible for GXP testing. The number of patients who fulfilled various eligibility criteria are shown in Table 2.
Of those 2,331 patients eligible for GXP testing, 1,066 (46%) had not undergone GXP tests. The demographic and clinical characteristics of all enrolled patients, GXP eligible patients and those who had not undergone GXP tests are shown in Table 3. Adjusted analysis indicated the following: Patients from townships without GXP testing facilities were 6.4 times more likely to not undergo GXP tests when compared to patients from townships with GXP testing facilities. Patients who were new TB cases were 3.8 times more likely to not undergo GXP tests when compared to retreatment TB patients. Patients whose HIV status was negative or unknown were 1.7 times and 2.2 times more likely to not undergo GXP tests when compared to HIV positive patients. Extra-pulmonary TB patients were 2 times more likely to not undergo GXP test when compared to pulmonary TB patients. Additionally, patients aged 45–64 years (when compared to those aged 15 to 44 years) were more likely to undergo GXP test.
Of those patients who had undergone GXP test, 26 patients (2% of GXP tested patients) were diagnosed as RR-TB and 23 of them (88% of detected RR-TB) were initiated on MDR-TB treatment. The remaining 3 patients died before initiating MDR-TB treatment (data not shown in the table).
Duration between the treatment initiation and GXP testing
In those who had undergone GXP tests (n = 1,265 patients), we assessed whether they had received GXP testing before or after the initiation of TB treatment [Ideally, patients should have GXP testing before initiating TB treatment with first line anti-TB drugs]. Because of the deficiencies in recording dates, for 417 (33%) patients, we could not ascertain whether they had undergone GXP test before or after TB treatment initiation. In the remaining 848 patients, 381 (44%) had undergone GXP tests at least a day after initiating TB treatment (median delay 6 days (IQR: 1–10 days). The delays of these 381 patients disaggregated by demographic and clinical characteristics are shown in Table 4. Patients from townships without GXP machines had longer delays when compared to patients from townships with GXP machines.
Qualitative part
Health care provider perspectives for not testing eligible patients with GXP tests
All participants (n = 32) provided consent to participate in KII. The analysis of KII data yielded 6 thematic reasons for not identifying and testing eligible patients for GXP tests and 5 thematic solutions for addressing this issue. The reasons and solutions (along with supporting quotes) are given in Table 5. The most commonly quoted reasons pertained to the themes: unaware of the current guidelines regarding the eligibility criteria for GXP tests, challenges in sputum collection and transportation from patients to the GXP testing sites, human resource constraints (non- availability of additional human resources to cope with the workload) followed by challenges in educating the importance of GXP tests to the patients so that they also make efforts to undergo these tests.
Discussion
This is one of the first studies from the Myanmar NTP to assess the magnitude and reasons for pre-diagnosis attrition. The study highlights that 41% of the total TB patients were eligible for GXP testing among TB patients enrolled for first line anti-TB treatment according to 2016 NTP GXP eligible criteria. However, nearly half of them were not tested by GXP. Patient characteristics associated with non-testing were: female sex, patients from TB township without GXP testing facilities, new TB cases, extra-pulmonary TB cases, HIV negative or HIV unknown TB cases. In those who underwent GXP testing, about 44% received the test after initiating TB treatment. The major strength of this study was having a qualitative component to better understand health care provider perspectives on reasons for the programmatic gaps identified in the study.
There were three major limitations of the study: First, since we used routine programme data, there could be errors in recording information on patient care i.e., health care providers may have provided services, but may not have recorded them. Since the programme conducts routine supportive supervisory visits which include on-site verification of records and reports, the errors in recording (if any) are likely to be minimal and random. We strongly feel that programmatic gaps observed in this study, are indicative of the actual gaps in implementation rather than gaps due to errors in recording and reporting information. Second, our analysis and interpretation is restricted to the variables that are routinely collected in the NTPs records. We know that some variables like socio-economic status and distance of the patient’s residence from the health facility can play a major role in eligible patients’ accessing GXP testing services. Since we have not collected information on these variables, we are unable to account for their influence in our analysis. Therefore, the magnitude and direction of association between demographic and clinical variables on GXP testing could be affected by un-measured confounding. Third, in the qualitative part of the study we interviewed only the health care providers and not the patients. Therefore, we are unable to provide the patient perspectives on pre-diagnosis attrition. Moreover, it is possible that health care providers may have given answers that are programmatically desirable. We tried to minimize this by explaining the nature and importance of this research to the study participants and the KIIs were conducted by co-investigators who were not supervisors of the participants.
Despite these limitations, the study’s findings have the following implications on policy and practice.
First, the magnitude of patients eligible for GXP testing was found to be 41% in our study. Since the proportion eligible is highly contextual and is dependent on the local NTP criteria, we are unable to compare this proportion with similar studies from other countries who follow different national eligibility criteria. However, the proportion described in our study could be an underestimate as none of the patients had information on “diabetes mellitus” or “contact with an MDR-TB” recorded in the patient files. This was due to lack of specific ‘fields’ for recording this information in the NTP records. To ensure better implementation of the guidelines and also to facilitate monitoring, we recommend that NTP should revise their recording formats to capture information on all eligibility criteria.
Second, 54% of the patients eligible for GXP testing received the test with 46% pre-diagnosis attrition. Previous studies from India, Bangladesh, Cambodia have reported pre-diagnosis attrition ranging from as low as 17% (in Cambodia) to as high as 60% (in India)16,17,18,19. The proportion GXP tested in Bago Region (as per our study results was below the 70% target set by the NTP for GXP testing and also falls well below the 90% target set in the End TB Strategy for the detection and treatment of all forms of TB including MDR-TB20. This study provides reasons and some solutions to address this gap from the health care providers’ perspective. Of particular concern is the lack of awareness about the current guidelines for GXP testing among health care providers. This could have been avoided by training and better in-house communication and information transmission system among the NTP staff about the current guidelines. The NTP should consider implementing these suggested solutions and monitor the improvements over a period of time. Along with the revisions in patient recording formats, the NTP should revise the reporting format so that cohort information on the number of patients eligible for GXP tests, number tested, and number of RR-TB patients detected and initiated on treatment can be monitored routinely and acted upon.
Third, several patient characteristics were associated with non-testing among GXP eligible patients. From the KIIs it was clear that they were following old NTP criteria, which did not include new smear positive patients, HIV negative or unknown patients for GXP testing. Therefore, these cases were missed. Similarly, patients from townships without GXP testing facilities were facing challenges in sputum collection and transportation. Therefore, the attrition was higher in these townships. Although the reason why attrition was relatively higher in female patients is not clearly known, the relative difference was too small to warrant further investigation. Similarly, only 2% of the TB patients aged (<15 years) were identified as GXP eligible patients when compared to other age groups where nearly 50% of the patients were eligible for GXP-tests. This raises concerns about the adequacy of the present criteria in early detection of RR-TB among younger age groups.
Fourth, by implementing the solutions recommended by the health care providers, gaps in GXP testing for female patients, new TB cases, HIV negative or unknown TB patients could be addressed by training and monitoring health care staff activities. For implementing the solutions to address the gaps in GXP testing for patients from TB townships without GXP testing facilities may require additional financial investment to increase the number of GXP testing facilities and/or improve the sputum collection and transportation systems21. However, gaps in GXP testing for extra-pulmonary patients may remain high due to the challenges in collecting appropriate biological specimens for GXP testing (e.g., cerebrospinal fluid, pleural fluid) at peripheral health facilities.
Fifth, in patients who had undergone GXP testing, nearly 44% had this test after being initiated on first line TB treatment. The delay was higher in TB patients from townships without GXP testing facilities. This is primarily due to the practice of fortnightly/weekly sputum collection and transportation from these townships. Although this finding is positive and as per the NTP guidelines that patients are initiated on TB treatment immediately after TB diagnosis (without waiting for GXP result confirmation), it is of concern that patients at high risk for RR-TB initiate treatment without proper diagnosis. In order to address this complex situation, the existing sputum collection and transportation system should be improved while achieving shorter turnaround times.
Lastly, in the qualitative component of the study, issues related to human resource (unavailability of TB focal person in certain townships, frequent turnover of TB focal person) were one of the main reasons for high pre-diagnosis attrition. Allocation of dedicated human resources for TB activities and ensuring their continuous presence is an important solution to narrow this gap.
Conclusion
In Bago region, 41% of the TB patients enrolled on first line anti-TB treatment were eligible for GXP testing. Pre-diagnosis attrition was high with nearly half of the eligible patients not tested with GXP tests. Training of TB health care providers about the latest GXP testing criteria, improvement in sputum collection and transportation system particularly for townships without GXP testing facilities, allocation of dedicated human resource for TB activities, and enhanced recording, reporting, supervision and monitoring are urgently required to reduce the attrition.
Data Availability
The data can be obtained from the corresponding author after approval from the National TB Programme and the Department of Medical Research, Ministry of Health and Sports, Government of Myanmar. Anyone interested in the raw data may please contact the corresponding author.
References
World Health Organization. Global Tuberculosis report 2018 (2018).
World Health Organization (WHO). Global Tuberculosis Report 2017. World Health organization (WHO) WHO/HTM/TB/2017.23 (2017).
Shewade, H. D. et al. Low pre-diagnosis attrition but high pre-treatment attrition among patients with MDR-TB: An operational research from Chennai, India. Journal of Epidemiology and Global Health 7, 227–233 (2017).
MacPherson, P., Houben, R. M., Glynn, J. R., Corbett, E. L. & Kranzer, K. Pre-treatment loss to follow-up in tuberculosis patients in low- and lower-middle-income countries and high-burden countries: a systematic review and meta-analysis. Bulletin of the World Health Organization 92, 126–138 (2014).
Subbaraman, R. et al. The Tuberculosis Cascade of Care in India’s Public Sector: A Systematic Review and Meta-analysis. Plos Medicine 13, e1002149 (2016).
National Tuberculosis Programme (NTP). Guidelines for the Manangement of DR-TB in Myanmar 2017. 14, (National Tuberculosis Programme, 2016).
Steingart, K. R. et al. In Cochrane Database of Systematic Reviews (ed. Steingart, K. R.) CD009593, https://doi.org/10.1002/14651858.CD009593.pub2 (John Wiley & Sons, Ltd, 2013).
National Tuberculosis Programme. National Strategic Plan for Tuberculosis 2016–2020. (National Tuberculosis Programme (Myanmar) 2016).
Htet, K. K. K. et al. Rifampicin-resistant tuberculosis patients in Myanmar in 2016: how many are lost on the path to treatment? The International Journal of Tuberculosis and Lung Disease 22, 385–392 (2018).
Ministry of Immigration and Population. Myanmar census. (Ministry of Immigration and Population, 2014).
Williams, C. Research Methods. 5, 65–72 (2007).
National Tuberculosis Programme. BHS Mannual for TB Management (2016). (National Tuberculosis Programme (Myanmar) 2016).
Fetters, M. D., Curry, L. A. & Creswell, J. W. Achieving Integration in Mixed Methods Designs- Principles and Practices. Health services research 48, 2134–2156 (2013).
von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)statement: guidelines for reporting observational studies. J Clin Epidemiol 61, 344–349 (2008).
Tong, A., Sainsbury, P. & Craig, J. Consolidated criterio for reporting qualitative research (COREQ): a 32- item checklist for interviews and focus group. International Journal of Qualitative in Health Care 19, 349–357 (2007).
Shewade, D. et al. High pre-diagnosis attrition among patients with presumptive MDR-TB: an operational research from Bhopal district, India. BMC Health Services Research 17, 1–9 (2017).
Hossain, S. T. et al. The Multi-Drug Resistant Tuberculosis Diagnosis and Treatment Cascade in Bangladesh. PloS one 10, e0129155 (2015).
Chadha, S. S. et al. Operational challenges in diagnosing multi-drug resistant TB and initiating treatment in Andhra Pradesh, India. PLoS One 6, 1–5 (2011).
Khann, S. et al. Linkage of Presumptive Multidrug Resistant Tuberculosis (MDR-TB) Patients to Diagnostic and Treatment Services in Cambodia. PLoS One 8, 1–5 (2013).
Stop, T. B. Partnership. Global Plan to End TB, The paradigm (2016–2020). Stop TB partnership Available at, http://www.stoptb.org/global/plan/plan2/ (2016).
Shewade, H. D. et al. MDR-TB in Puducherry, India: reduction in attrition and turnaround time in the diagnosis and treatment pathway. Public Health Action 6, 242–246 (2016).
Acknowledgements
This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO/TDR). The model is based on a course developed jointly by the International Union Against Tuberculosis and Lung Disease (The Union) and Medécins sans Frontières (MSF/Doctors Without Borders). The specific SORT IT program which resulted in this publication was jointly organized and implemented by The Centre for Operational Research, The Union, Paris, France; The Department of Medical Research, Ministry of Health and Sports, Myanmar; The Department of Public Health, Ministry of Health and Sports, Myanmar; The Union Country Office, Mandalay, Myanmar; The Union South-East Asia Office, New Delhi, India; and Burnet Institute, Australia. The training program, within which this paper was developed, was funded by the Department for International Development (DFID), UK, and the United States Agency for International Development (USAID) through Challenge TB and FHI 360. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Tun Oo (T.O.), Khine Wut Yee Kyaw (K.W.Y.K.), Kyaw Thu Soe (K.T.S.), Saw Saw (S.S.), Srinath Satyanarayana (S.N.S.), Si Thu Aung (S.T.A.). Protocol development: T.O., K.W.Y.K., S.S., K.T.S., S.N.S., S.T.A. Data collection: T.O., K.W.Y.K., K.T.S. Data analysis: T.O., K.W.Y.K., S.S., S.N.S. Data interpretation: T.O., K.W.Y.K., S.S., K.T.S., S.N.S., S.T.A. Manuscript writing: T.O., K.W.Y.K., S.N.S. Final approval: S.S., S.T.A.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oo, T., Kyaw, K.W.Y., Soe, K.T. et al. Magnitude and reasons for pre-diagnosis attrition among presumptive multi-drug resistant tuberculosis patients in Bago Region, Myanmar: A mixed methods study. Sci Rep 9, 7189 (2019). https://doi.org/10.1038/s41598-019-43562-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-43562-3
This article is cited by
-
Impacts of a comprehensive tuberculosis control model on the quality of clinical services and the financial burden of treatment for patients with drug-resistant tuberculosis in China: a mixed-methods evaluation
Infectious Diseases of Poverty (2021)
-
Age and sex distribution of Mycobacterium tuberculosis infection and rifampicin resistance in Myanmar as detected by Xpert MTB/RIF
BMC Infectious Diseases (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.