Abstract
The aim of this study is to determine the relationship between AS and subsequent depression. This study was conducted using a nationwide dataset available in Korean National Health Insurance System (KNHIS). We identified 11,465 newly diagnosed AS patients and 57,325 patients without AS in the ratio of 1:5 matched by sex, age, and index date, between 2010 and 2014. We investigated any latent characteristics in the patients’ demographic information and chronic comorbidities that could trigger a depression when diagnosed with AS. By comparing the cohort data, the hazard ratio of developing subsequent depression in AS patients was calculated and adjusted based on several risk factors. Despite the adjustment of demographic variables and chronic comorbidities, the risk of depression was 2.21 times higher in the AS cohort than in the control group. Multivariate analysis showed that AS patients with female gender, old age and low-income status showed higher risks of developing depression. Additionally, the presence of chronic comorbidities including diabetes mellitus, hypertension, hyperlipidemia, cancer, stroke, and chronic kidney disease increased the patients’ risk of depression. The AS patients with stroke were reported to have the highest risk of depression. This population-based cohort study showed that AS significantly increased the subsequent risk of developing depression. Moreover, the development of a depression is influenced by certain demographic variables and different chronic comorbidities.
Similar content being viewed by others
Introduction
Ankylosing spondylitis (AS) is a chronic inflammatory rheumatic disease that mainly affects the axial skeleton, resulting in structural and functional impairments1. The main symptoms of AS patients include musculoskeletal pain, stiffness, and fatigue2. In addition, the first wave of symptoms usually starts before 30 years, and the progressive nature of the disease affects the physical function, causing deterioration of the patients’ professional capacity and quality of life3. AS is irreversible and requires lifelong treatments. This poses an increased risk of developing psychological disorders such as depression4. Compared with rheumatoid arthritis, the nationwide longitudinal follow-up data of depression prevalence among AS patients is scarce in its size and depth.
Numerous studies have already shown that the prevalence of depression is higher among the patients with chronic disease and that the psychological aspect of treatment is as critical as the clinical treatment5,6,7. Recent studies reveal that patients with patients with AS have an increased risk of developing chronic diseases such as diabetes mellitus and cardiovascular and cerebrovascular diseases8,9,10,11. Therefore, in the clinical approach to AS patients, it is essential to determine any other existing chronic diseases and be aware of the risks of developing depression from such diseases.
This study aims to have reviewed the prevalence of diagnosing depression in AS patients versus the general population using a nationwide population-based cohort study. Furthermore, our team compared the prevalence of chronic disease in AS patients to the general population based on the Korean National Health Insurance System (KNHIS) data and examined varying risks of developing depression in patients with existing chronic diseases.
Methods
Data source
This study used a nationwide dataset available in the Korean National Health Insurance System (KNHIS) collected from 2010 to 2014. In South Korea, the government has implemented an obligatory National Health Insurance (NHI) system, covering 97% of the population and allowing patients to pay only about 30% of the total healthcare cost. The remaining 3% of the population is the lowest income households, and the Medical Aid Program covers all their medical expenses. Healthcare institutions submit claims for the remaining 70% of the total medical cost to the government. Therefore, the medical information of almost all patients in healthcare institutions are prospectively integrated into the KNHIS claim database. The KNHIS claim database includes extensive information on the diagnoses and comorbidity codes classified by the International Classification of Diseases, 10th revision (ICD-10), demographic characteristics, admission and ambulatory care, prescription records, and procedure codes.
Data collection
We filtered the ICD-10 codes to identify all patients with AS who were included in the KNHIS database from January 2010 to December 2014. The ICD-10 codes for AS (M45.0–45.9) in the Rare Intractable Diseases (RIDs) program were used. The NHI has included AS in the Rare Intractable Diseases (RIDs) registration program since 2009. In the RID grogram, patients were diagnosed with AS if they met the modified New York criteria12. The NHI reviews the RID program application again to ensure the diagnostic criteria are met. (Because patients with an RID receive more coverage and pay only about 10% of the total medical cost) This process ensures that diagnoses for the RID program are reliable13.
After AS diagnosis, the following categories were used to find demographic variables and comorbidity rate. The low-income household group was defined as the bottom quintile of the general population. Urban resident group were stratified from cities consisting of more than 1 million population (Seoul, Busan, Incheon, Daegu, Daejeon, Ulsan, and Gwangju).
Using ICD-10 codes, the selected baseline comorbidities included diabetes mellitus (ICD-10, E11-14), hypertension (ICD-10, I10-13,15), hyperlipidemia (ICD-10, E78), and stroke (ICD-10, I63, 64). Comorbidities were recognized if the disease appeared in subjects prompted three or more visits in the principal and/or secondary diagnose. To increase the diagnostic code validity, the suitability of prescription drugs was reviewed for selected diseases.
Patients with cancer were selected from patients diagnosed with ICD-10 codes beginning with “C” and registered in the government’s special medical subsidy program. Likewise, patients with end-stage renal disease (ESRD) were chosen from patients who had ICD-10 codes N18 or N19 and underwent renal replacement therapy such as hemodialysis and peritoneal dialysis. Lastly, patients with depression were selected from those who had undergone medical treatment with ICD-10 codes F32 or F33.
Study design and cohort
From the KNHIS database, we identified the AS group which consisted of newly diagnosed AS patients from 2010 to 2014. To firmly support the data on the prevalence of developing depression after diagnosed with AS, 2,993 patients who were diagnosed with depression at least once since 2002 were excluded from the study. Then, the gender and age for newly diagnosed AS patients were matched with the control group in a 1:5 ratio. Patients in the control group were randomly sorted before being selected from top to bottom to prevent selection bias. The group without five control individuals was excluded in the matching process (n = 1,089). The result of our study compared the prevalence of depression among 11,465 newly diagnosed AS patients and 57,325 patients in the control group in December 2015 (Fig. 1).
Ethical statement
The study protocol was approved by the KNHIS institutional review board. An informed-consent exemption was granted by the board.
Statistical analysis
The Chi-squared test was used to examine the different demographic variables and disease phenotypes between the AS and control cohorts. The depression-free survival rate and differences between the two groups were evaluated using the Kaplan–Meier method and the log-rank test, respectively. The Cox proportional hazards regression analysis was used to calculate the hazard ratio (HR) and 95% confidence interval (CI) of depression for AS patients compared with the control group. The multivariate Cox proportional hazards model was used to identify the risk factors of depression and adjusted hazard ratio within the AS cohort. Statistical analyses were performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA). P-values less than 0.05 were considered statistically significant.
Results
Characteristics and depression incidence between the two cohorts
The distributions of demographic variables and chronic disease between AS patients and control cohorts are shown in Table 1. Because of the 1:5 age-sex stratified matching, the proportion of sex and mean age was identical for both groups. On the other hand, AS patients are generally distributed in the low-income household group and living in urban areas. Comorbidities, including diabetes mellitus, hypertension, hyperlipidemia, cancer, stroke, and chronic renal disease, were higher in AS patients (p < 0.001). During the follow-up period, the incidence of newly diagnosed depression was 10.84% (n = 1,243) in the AS group (n = 11,465) and 5.05% (n = 2,894) in the control group (n = 57,325). Hence, the incidence of depression in the AS group was significantly higher than that in the control group (p < 0.001) (Table 1).
Risk of depression in AS patients
Among 68,790 patients (11,465 AS patients and 57,325 control subjects), a total of 4,137 individuals developed depression (1,243 AS patients and 2,894 control subjects during the follow-up of 37,275.35 and 195,703.29 person-years, respectively.) The incidence rate of depression in the AS cohort was greater than that in the control group (33.35 versus 14.79 per 1,000 person-years).
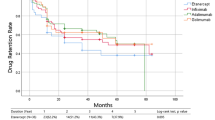
The multivariate Cox proportional hazards regression analysis was used to estimate the HR of newly diagnosed depression among AS patients based on the statistical adjustment (Model 1: age and sex, Model 2: age, sex, household income, diabetes mellitus, hypertension, hyperlipidemia, stroke, cancer, and ESRD). A markedly higher risk of developing subsequent depression was noted in AS patients than in the matched controls (adjusted HR: 2.3, 95% CI: 2.152–2.458 in Model 1 and adjusted HR: 2.211, 95% CI: 2.068–2.363 in Model 2) (Table 2). The KM curves with cumulative hazards showed a significantly higher incidence of overall depression in the AS group than the control group (p-value for the log-rank test <0.001). Moreover, the gap difference between two KM curves of the AS and control groups increased with time (Fig. 2).
Subgroup analysis of the risk of depression in AS patients
The multivariate Cox proportional hazard regression analysis was used to estimate the adjusted HR of depression among AS patients based on the demographic data and chronic disease comorbidity (Table 3). Compared to the male gender, the female gender had a higher risk of depression in AS patients (HR: 1.60, 95% CI: 1.50–1.71). Higher depression rate was observed in patients diagnosed with AS above 40 years than those diagnosed below 40 years (HR: 1.78, 95% CI: 1.65–1.90). The low-income group (bottom 20% of the general income) appeared to have a mildly higher risk of developing depression (HR: 1.28, 95% CI: 1.20–1.37). There was little difference in the risk of depression based on residence (HR: 1.08, 95% CI: 1.01–1.14). Additionally, the presence of comorbidities increased the risk of depression. AS patients with stroke have the highest risk (HR: 2.06, 95% CI: 1.73–2.43), followed by those with ESRD (HR: 2.05, 95% CI: 1.35–3.09), with cancer (HR: 1.65, 95% CI: 1.37–1.99), with hypertension (HR: 1.49, 95% CI: 1.36–1.63), with dyslipidemia (HR: 1.32, 95% CI: 1.19–1.47), and with diabetes mellitus (HR: 1.26, 95% CI: 1.12–1.41) (Table 3).
Discussion
This is a cohort study that determines the risk of subsequent depression following the diagnosis of AS based on the national administrative data. This study has shown that AS patients had higher prevalence of chronic comorbidities (diabetes mellitus, hypertension, hyperlipidemia, cancer, stroke, ESRD) compared to the control group in terms of the age and sex. In addition, the income level and location of residence affects the prevalence of AS. Even after negating the effects of demographic variables and comorbidity, the study has revealed that AS patients are 2.21 times more likely to develop the risk of depression than those without AS.
Numerous studies involving the relationship between AS and depression have been conducted2,4,6,14. In AS patients, inflammatory pain caused sleep disturbance and lowered the fatigue level in social life. In other words, the severity of the disease affects the individual’s quality of life and increases the risk of depression unless the disease activity in AS has fully subsided2,3,15. Similarly, AS patients exhibited poor functional outcome at work, and their consequent socioeconomic status influenced the prevalence of depression16,17. Recent studies reported that proinflammatory cytokines take important roles in the pathophysiology of depression18. In other words, systemic inflammation and proinflammatory cytokines of AS are associated with depression19. This is also supported by the fact that infliximab (tumor necrosis factor-α drug) is effective in the treatment of AS patients with depression20. Hence, the biological, functional, and socioeconomic factors of AS patients increase the risk of depression.
However, few studies have examined the data on subsequent depression in AS patients compared to those with rheumatoid arthritis. In the previous AS cohort study consisting 1,738 out of 967,012 subjects, 10% of the AS cohort had a doctor-diagnosed depression compared to 6% of the control group in the 13-year observational period. Furthermore, the risk of depression was higher in females and in AS patients with diabetes mellitus4. However, person-time for residents not seeking healthcare during the study time frame was not included, and any other chronic comorbidities other than diabetes mellitus were not considered.
Studies have shown that the prevalence of comorbidities including cardiovascular disease, stroke, diabetes mellitus, and renal disease is higher in AS patients10,11,21,22. The direct cause has not yet been established; however, it is speculated to be the common pathological pathway or biological background of the disease. Several studies have already presented the importance of the psychological aspect such as depression in the treatment of patients with chronic diseases. Additionally, recent studies show that drugs for chronic diseases, such as oncologic medication, corticosteroids, or biological agents, can trigger depressive episodes. Therefore, it is important to identify any chronic comorbidities in AS patients to factor in the risk of depression from those comorbidities.
This study explains the temporal association between AS and the prevalence of depression. Compared to the control group, AS patients had greater risk of depression as the time progressed from the initial diagnosis. In the fifth year following the initial diagnosis, 1.5 out of 10 AS patients and 0.5 out of 10 non-AS patients required the administration of anti-depressant drugs. Females and low-income patients were more susceptible to depression. Additionally, patients above 40 years who were diagnosed with AS were more vulnerable to depression than those below 40 years who were aware of their condition. This study examined the risk of developing depression in various comorbidities including stroke, cancer, chronic kidney disease, hypertension, diabetes mellitus, and hyperlipidemia, with the stroke comorbidity being the highest. These results, altogether, will provide substantive and applicable information of the psychological aspect in the treatment of AS patients.
There are certain limitations of our study. First, the KNHIS dataset does not contain detailed information on the physical activities, body mass index, or history of smoking, alcohol consumption, and family history of psychological disorders; all of which may be associated with psychological disorders. Although our team was not able to adjust for all potential confounding variables, the study is noteworthy for including different comorbidities and varying demographic characteristics, residential locality, and household income and proves that AS patients have significantly higher risk of developing depression. Second, miscoding of ICD-10 diagnostic code could have been done. Nevertheless, this study rechecks the appropriateness of prescription drugs to minimize error and maximize reliability of the diagnostic code. Third, because we had to use administrative data, the severity and duration of symptoms were not considered in this study. This study focused on the risk of developing depression after the point of AS diagnosis.
In conclusion, this study has shown that patients with AS is 2.21 times more likely to develop the risk of depression than the general population, even after negating several potentially influential variables of demographic characteristics and comorbid conditions. Our population-based study has also revealed that AS is more common among low-income individuals with other chronic diseases. Clinicians treating AS patients should acknowledge the demographic characteristics, comorbidity, risk factors, and latent risk for depression.
References
Braun, J. & Sieper, J. Ankylosing spondylitis. Lancet 369, 1379–1390 (2007).
Gunaydin, R., Karatepe, A. G., Cesmeli, N. & Kaya, T. Fatigue in patients with ankylosing spondylitis: relationships with disease-specific variables, depression, and sleep disturbance. Clinical Rheumatology 28, 1045–1051 (2009).
Dagfinrud, H., Kjeken, I., Mowinckel, P., Hagen, K. B. & Kvien, T. K. Impact of Functional Impairment in Ankylosing Spondylitis: Impairment, Activity Limitation, and Participation Restrictions. J Rheumatol 32, 516–523 (2005).
Meesters, J. J. L. et al. The risk for depression in patients with ankylosing spondylitis: a population-based cohort study. Arthritis Res Ther 16 (2014).
Geenen, R., Newman, S., Bossema, E. R., Vriezekolk, J. E. & Boelen, P. A. Psychological interventions for patients with rheumatic diseases and anxiety or depression. Best Pract Res Cl Rh 26, 305–319 (2012).
Martindale, J. et al. Disease and psychological status in ankylosing spondylitis. Rheumatology 45, 1288–1293 (2006).
Hyphantis, T. et al. The relationship between depressive symptoms, illness perceptions and quality of life in ankylosing spondylitis in comparison to rheumatoid arthritis. Clinical Rheumatology 32, 635–644 (2013).
Mercieca, C., van der Horst-Bruinsma, I. E. & Borg, A. A. Pulmonary, renal and neurological comorbidities in patients with ankylosing spondylitis; implications for clinical practice. Curr Rheumatol Rep 16 (2014).
Nurmohamed, M. T., van der Horst-Bruinsma, I. & Maksymowych, W. P. Cardiovascular and Cerebrovascular Diseases in Ankylosing Spondylitis: Current Insights. Curr Rheumatol Rep 14, 415–421 (2012).
Chen, H. H. et al. Ankylosing spondylitis and other inflammatory spondyloarthritis increase the risk of developing type 2 diabetes in an Asian population. Rheumatology International 34, 265–270 (2014).
Kang, J. H., Chen, Y. H. & Lin, H. C. Comorbidity profiles among patients with ankylosing spondylitis: a nationwide population-based study. Annals of the Rheumatic Diseases 69, 1165–1168 (2010).
Vanderlinden, S., Valkenburg, H. A. & Cats, A. Evaluation of Diagnostic-Criteria for Ankylosing-Spondylitis - a Proposal for Modification of the New-York Criteria. Arthritis Rheum 27, 361–368 (1984).
Park, J. S., Hong, J. Y., Park, Y. S., Han, K. & Suh, S. W. Trends in the prevalence and incidence of ankylosing spondylitis in South Korea, 2010–2015 and estimated differences according to income status. Sci Rep-Uk 8 (2018).
Sundquist, K., Li, X. J., Hemminki, K. & Sundquist, J. Subsequent risk of hospitalization for neuropsychiatric disorders in patients with rheumatic diseases. Arch Gen Psychiat 65, 501–507 (2008).
Singh, J. A. & Strand, V. Spondyloarthritis Is Associated with Poor Function and Physical Health-Related Quality of Life. J Rheumatol 36, 1012–1020 (2009).
Boonen, A. Socioeconomic consequences of ankylosing spondylitis. Clin Exp Rheumatol 20, S23–S26 (2002).
Frauendorf, R., Pinheiro, M. D. & Ciconelli, R. M. Variables related to work productivity loss in patients with ankylosing spondylitis. Rev Bras Reumatol 53, 303–309 (2013).
Raison, C. L., Capuron, L. & Miller, A. H. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol 27, 24–31 (2006).
Berk, M. et al. So depression is an inflammatory disease, but where does the inflammation come from? Bmc Med 11 (2013).
Ertenli, I. et al. Infliximab, a TNF-alpha antagonist treatment in patients with ankylosing spondylitis: the impact on depression, anxiety and quality of life level. Rheumatology International 32, 323–330 (2012).
Bremander, A., Petersson, I. F., Bergman, S. & Englund, M. Population-Based Estimates of Common Comorbidities and Cardiovascular Disease in Ankylosing Spondylitis. Arthrit Care Res 63, 550–556 (2011).
Han, C. L. et al. Cardiovascular disease and risk factors in patients with rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. J Rheumatol 33, 2167–2172 (2006).
Author information
Authors and Affiliations
Contributions
J.-S.P., H.-D.J., J.-Y.H., Y.-S.P., K.H., S.-W.S., S.-Y.P. and B.-T.K. conceived the project and developed the overall research plan. K.H. performed statistical analyses. J.-S.P. and H.-D.J. wrote the manuscript. J.-S.P., H.-D.J., J.-Y.H., Y.-S.P., K.H., S.-W.S., S.-Y.P. and B.-T.K. interpreted the data and critically revised the manuscript for important intellectual content. J.-S.P., H.-D.J. and J.-Y.H. had primary responsibility for final contents. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, JS., Jang, HD., Hong, JY. et al. Impact of ankylosing spondylitis on depression: a nationwide cohort study. Sci Rep 9, 6736 (2019). https://doi.org/10.1038/s41598-019-43155-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-43155-0
This article is cited by
-
Exploring the emotional impact of axial Spondyloarthritis: a systematic review and thematic synthesis of qualitative studies and a review of social media
BMC Rheumatology (2023)
-
Association between depression, anxiety, chronic pain, or opioid use and tumor necrosis factor inhibitor persistence in inflammatory arthritis
Clinical Rheumatology (2022)
-
Dose Reduction of Tumor Necrosis Factor Inhibitor and its Effect on Medical Costs for Patients with Ankylosing Spondylitis
Rheumatology and Therapy (2021)
-
Positive association of Parkinson’s disease with ankylosing spondylitis: a nationwide population-based study
Journal of Translational Medicine (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.