Abstract
Our purpose was to prospectively analyze the age-related changes of corneal Scheimpflug parameters in healthy subjects. Thirty-five eyes of 35 volunteers (age 14–67 years) were investigated with an average interval of 3.6 years. Changes of corneal parameters (flattest keratometric reading at anterior (K1F) and posterior surface (K1B), steepest keratometric reading at anterior (K2F) and posterior surface, anterior astigmatism, posterior astigmatism (AstigB), flat axis of anterior and posterior astigmatism (AxisB), thinnest pachymetric value (PachyMin), corneal volume (CV10-mm)) were analyzed. K1F and K2F decreased significantly during observation and showed stronger decrease in younger than in older individuals. Higher values proved to be more stable. K1B decreased significantly and the degree of decrease was dependent on its baseline value and age: in young subjects low values increased, high values decreased. AstigB decreased significantly and showed a baseline-dependent significant increase from lower and a significant decrease from higher initial values. Over time, the mean AxisB shifted significantly. PachyMin and CV decreased significantly with age, especially from higher baseline values in younger subjects. The results of this longitudinal study suggest that both corneal surfaces change significantly with age. We demonstrate for the first time that age and baseline values influence age-related changes of corneal parameters.
Similar content being viewed by others
Introduction
Aging is a physiological process and occasionally it is hard to differentiate between time dependent biological changes and damages from environmental insults1. Age-related changes occur in all structures of the eye, with various consequences2. Age has been identified as an important individual variable affecting the outcome after keratorefractive surgery3.
Corneal aging generates structural and functional changes including steepening of keratometry indices, and a rotation of the axis of astigmatism resulting in a shift from with-the-rule to against-the-rule astigmatism1,4,5,6,7,8,9,10,11. Alterations of higher-order aberrations of the cornea are also well known9. The level of astigmatism decreased significantly with age both of the anterior and posterior corneal surfaces in a study by Nemeth et al.9, although age as a primary factor was not analyzed in this report.
To differentiate between physiological and pathological changes of the aging cornea, it is indispensable to know what the physiological changes are. There are clinical situations where it is important to distinguish between pathological and normal age-related changes. The assessment of the progression of ectatic corneal disorders in young patients determines the optimal treatment and the glaucoma management in the elderly can only be personalized if we take account the changes of corneal thickness. A complete and precise evaluation of the cornea must take keratometric, astigmatic vectorial as well as pachymetric characteristics into account.
Age-dependent change of corneal thickness has been studied extensively. Corneal thickness decreases throughout infancy; during babyhood (around 3 years of age) it reaches adult thickness and, from that point on, central corneal thickness (CCT) appears to be stable over time12. However, age-related change in corneal thickness appears to be rather controversial in other studies13,14,15,16,17,18. CCT has been extensively investigated in glaucoma development in the elderly, and it is known to directly affect the strategy of glaucoma management13,14,19. Corneal ectatic disorders are characterized by progressive deformation of the corneal architecture and corneal thinning. Therefore, corneal thinning was extensively studied in young keratoconus patients20,21. Scheimpflug-based tomography provides corneal thickness map and curvature maps of both the anterior and the posterior surfaces which improves the sensitivity and specificity of keratoconus detection11,21,22.
Several studies examined normal age-related changes of corneal parameters (i.e. CCT, astigmatism, higher-order aberrations), most of what were cross sectional and not longitudinal in nature4,7,8,9,10,13,16,19,23,24. In the present study we determine age-related changes of corneal parameters using a Pentacam device in a healthy cohort aged between 14 and 67 years at baseline. To the best of our knowledge, this is the first longitudinal study evaluating age-related changes of corneal parameters measured with the Pentacam HR device covering a five-decade range of baseline age in healthy participants.
Patients and Methods
Subjects and clinical examinations
Our study comprised 35 healthy participants of European descent with 20/20 Snellen equivalent distance visual acuity with low refraction error (lower than 1.5 diopters [D]) but without other ophthalmological disorders. Following the tenets of the Declaration of Helsinki, written informed consent was signed by all participants and/or their parent and/or legal guardian for study participation prior to enrollment. The study protocol was approved by the Regional and Institutional Research Ethics Committee of the University of Debrecen (DEOEC-RKEB/IKEB 3313-2011). Exclusion criteria were: refraction error more than 1.5 D (including pathologic myopia and hyperopia), active inflammatory or infective systemic or ocular disease, current treatment with systemic or local drugs, use of eyedrops, contact lens wear, previous ocular surgery, abnormality in the lens or retina on biomicroscopic examination, precedent chemical injury or delayed epithelial healing, age less than 14 years, and pregnancy or lactation. Prior to a standard ophthalmological investigation, three images were captured of one randomly selected eye of each patient with high-resolution Pentacam (Pentacam HR, Oculus Optikgeräte GmbH, Wetzlar, Germany, software version 1.17r139) using a 12-mm wide Scheimpflug imaging technique. The device was set to a 25 images/second mode and images were taken in auto mode at perfect eye-set. In case of image distortion (e.g. blinking) or lack of data, the snapshot was repeated. The Pentacam evaluates five different parameters. The quality of the measurement is evaluated for each parameter by the equipment. A measurement is only considered reliable, if the quality of all the five parameters is approved by the equipment by giving an OK signal to the examiner. Data from all three images per session were averaged into session-level values.
All participants underwent repeated ophthalmological examination during a follow-up period of 3.6 years on average. At the baseline and follow-up visit the following parameters were recorded for each eye: examination date, Snellen visual acuity, spherical equivalent. The following data were exported from Pentacam to Microsoft Excel (Microsoft Corp, Redmond, Washington): Holladay equivalent keratometry values in the flat (K1) and steep (K2) meridian of the front and the back surface, maximal keratometry values of the front surface (Kmax), corneal astigmatism of the front and the back surface (Astig F and Astig B, respectively), corneal thickness at the thinnest point of the cornea (Pachy Min), the volume of the cornea in a diameter of 10 mm centered on the anterior corneal apex (C Vol D 10 mm), index of surface variation (ISV), index of vertical asymmetry (IVA), index of height asymmetry (IHA) and index of height decentration (IHD). The change in Pentacam parameters were analyzed always in comparison with the baseline values.
CCT is known to decrease throughout the day, with highest values found in the morning25. Therefore, all examinations in this study were performed between 8 and 10 am to correct for daily corneal thickness changes.
Statistical methods
Outcome parameters reported by the Pentacam system were mostly treated as untransformed continuous variables on their natural scales and units. Exceptions included corneal axis angles, which were consolidated into the range 0° to 90° to derive a laterality-independent measure of location within the range running from horizontal to vertical; and posterior corneal astigmatism values, which were sign reversed. Jackson’s cross cylinder power vector components (J0 and J45) were calculated for the anterior corneal surface (i.e., the simulated keratometric data) with the method described by Thibos et al.5. Unadjusted comparisons of follow-up vs baseline readings were based on paired t-tests if normality assumptions were satisfied or Wilcoxon’s matched-pairs signed-ranks tests otherwise. Male subjects were compared to females in terms of age using Wilcoxon’s rank-sum test. Multilevel mixed-effects linear regression was used for adjusted estimation of changes in outcome parameters through follow-up time. Adjustment variables included baseline readings of the outcome parameter, baseline age, and interaction terms between age and follow-up time, and between baseline reading and follow-up time (sex proved unnecessary to adjust for). Findings were expressed as estimated annual changes with 95% confidence intervals either as a function of baseline variable(s) (in presence of a significant interaction) or as a single overall estimate (in absence of significant interactions), and visualized using scatter plots of baseline reading of outcome parameter vs. age at baseline, with symbology indicating direction, significance, and magnitude of change over time. The statistical package applied was Stata version 11. The significance criterion was set at α < 0.05.
Ethical approval
The study protocol had been approved by the ethical board of University of Debrecen.
Statement of human and animal rights
The study protocol and execution complied with the Declaration of Helsinki.
Informed consent
All patients provided informed consent.
Results
Our study included thirty-five randomly selected eyes of 35 healthy volunteers of European descent (22 women and 13 men; 19 right and 16 left eyes). Participants were predominantly female (63%). There was no statistically significant difference regarding age between genders (p = 0.348). The mean age at the first visit was 31.8 years (SD: 12.4, range: 14.2–66.9 years). The average time interval between visits was 3.6 years (SD: 0.92, range: 2.1–5.7 years). The mean age at the control visit was 35.4 years (SD: 12.3, range: 16.4 to 69.2 years).
Detailed keratometric results of the anterior and posterior corneal surfaces and the differences between the two visits are displayed in Table 1. Both keratometric values (K1 and K2) on the anterior corneal surface decreased significantly during observation (p = 0.002 and 0.048, respectively), with no accompanying changes to K max. No significant changes in K1 and K2 were observed with unadjusted analysis on the posterior surface. The astigmatism parameter only changed significantly with aging on the posterior surface of the cornea (p = 0.022). The mean deviation from horizontal of the flat axis angle on the posterior surface (K1 B) was 8.5° (SD = 7.3°, range: 0.9–35.4°) at baseline and 10.2° (SD = 7.3°, range: 1.6–33.3°) at the end of follow-up. The difference was significant (p = 0.027). There was no significant difference between baseline and follow-up for the flat axis angle on the anterior corneal surface (K1 F) (p = 0.602). Regarding power vectors of the anterior surface, Jackson’s cross cylinder power vector component at 45° demonstrated weak changes with advancing age (p = 0.047).
The examination of pachymetric features of the cornea revealed that corneal thickness at the thinnest point of the cornea (Pachy min) decreased significantly with age (p < 0.001) (Table 2). In line with this, corneal volume in the central 10 mm also decreased significantly with age (p < 0.001). During follow-up, the Pentacam indices IHA and IHD showed significant increase (p ≤ 0.001), while ISV and IVA did not change (Table 2).
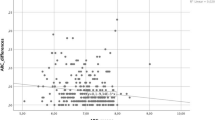
Taking baseline age into account, the front keratometric values (K1 and K2) decreased more substantially in younger than in older individuals, as shown in Fig. 1. Although unadjusted analysis shows no significant changes in K1 and K2 on the posterior surface, adjusted statistical modeling revealed that the keratometric reading on the posterior corneal surface in flat axis (K1B) changes in a heterogeneous fashion across baseline value and, to some extent, age. Low-range keratometric values, which are observed in younger subjects, increase significantly with time, while those in the high range do the opposite (Fig. 1).
Scatter plots of anterior and posterior K1 and K2 parameters of normal healthy corneas against age with model-predicted tendencies of change over time. K1 = flat-axis keratometric value in diopters (D) on anterior (F) and posterior (B) corneal surface; K2 = steep-axis keratometric value in diopters (D) on anterior (F) and posterior (B) corneal surface; NS = non-significant.
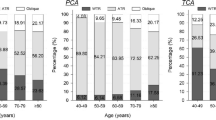
Neither the keratometric astigmatism parameter on the anterior surface of the cornea nor the J0 vector changed significantly with time. Adjusted analysis also shows that these two readings are stable across follow-up throughout the entire range of baseline readings and ages (Fig. 2). The borderline significant change detected in Jackson’s cross cylinder power vector component at 45° (unadjusted p = 0.047) is explained by a significant increase in older subjects with low to mid-range initial J45 values; values in younger subjects and in those with mid to high-range baseline readings did not change with advancing age (Fig. 2). Investigation into age-related progression of posterior corneal surface astigmatism revealed baseline dependent tendencies: if the baseline value of the astigmatism parameter was low, it tended to significantly increase, and if it was high, to significantly decrease during follow-up; this was true across the whole range of baseline age in our sample (Fig. 2).
Scatter plots of anterior and posterior astigmatism parameters and the power vectors J0 and J45 of normal healthy corneas against age with model-predicted tendencies of change over time. Astig F (D) = corneal astigmatism of the front surface in diopters, Astig B (D) = corneal astigmatism of the back surface in diopters, J0 = Jackson’s cross cylinder power vector component at 0 degrees for the anterior corneal surface; J45 = Jackson’s cross cylinder power vector component at 45 degrees for the anterior corneal surface; NS = non-significant.
Adjusted analysis shows that both the volume of the central 10 mm diameter of the cornea and the Pachy min parameter decrease significantly, especially from higher baseline measured values, with some suggestion of dependence on baseline age. Readings that are low at baseline, and also those registered in older subjects, seem to have a limited capacity to change (Fig. 3).
Scatter plots of the C Vol D 10 mm and Pachy min parameters of normal healthy corneas against age with model-predicted tendencies of change over time. C Vol D 10 mm = the volume of the central 10 mm diameter of the cornea; Pachy min = corneal thickness at the thinnest point of the cornea (μm); NS = non-significant.
Based on our analysis, the estimated annual change of Pentacam parameters of a normal, healthy eye are demonstrated in Table 3. It is found that, on the anterior surface of the cornea, K1 and K2 decrease significantly (although maintaining a stable Kmax); on the posterior surface, however, only high-range values of the flat keratometry parameter (K1) decrease significantly over time (p = 0.019). Front astigmatism seems to remain stable with aging, while higher initial absolute values of posterior astigmatism tend to reduce. Anterior axes of astigmatism do not seem to vary over time; initially horizontal posterior axes shift significantly towards the vertical, and those in the vertical or oblique angle at baseline do so towards the horizontal position. While J0 seems to be stable, J45 significantly increases from a low baseline (p = 0.012). The volume of the central 10 mm diameter of the cornea and the Pachy min parameters decrease stronger in thicker corneas.
Discussion
A wide range of changes occur in the aging cornea, some of which are clinically relevant for planning surgical procedures such as correcting astigmatism and myopia, for glaucoma management, and also for the management of corneal ectatic disorders. Reports on age-related changes of corneal thickness in healthy eyes are somewhat contradictory. Central corneal thickness seemed to be stable (mean change of CCT was −1.9 ± 14 μm) over 1.5 years in children12, while other studies reported no significant association between corneal thickness and age17,26. On the other hand, Rieth et al. detected significantly increased corneal thickness in the elderly in a cross sectional study16. In line with our observations, vast majority of previous studies report a statistically significant inverse relationship between age and corneal thickness13,14,15,18,23,24. In the present work we detected a 14-μm average decrease at the thinnest point of the cornea representing the strongest decrease reported in longitudinal studies so far (5 to 14 μm across 8.2 years, 3.5 μm across 3.8 years, 2.6 μm across 5 years reported by Weizer, Brandt and Hashemi et al., respectively)14,15,18. The mean ages of the longitudinal study samples were 50 to 60 years at the baseline visit14,15,18, which may explain why our younger patient population (mean age 31.8 years) showed more pronounced corneal thinning. This observation indicates that corneal tissue degradation is more pronounced in younger ages. There is only one study that analyzed thinnest point thickness change with a Pentacam device18. At the baseline in this study individuals were between 41 and 64 years old (average 49.9 years) and had a mean corneal thickness of 524.9 μm (SD 32), which is 13 μm thinner than in our younger study group of 14 to 67-year-old subjects (average 31.8 years). The difference in corneal thickness between these two different age groups confirms our observation on the age dependent corneal thinning found in our longitudinal study.
Little attention was paid to corneal volume in earlier studies, although it may sensitively follow topographical and pachymetric changes of the cornea and therefore is a sensitive indicator of corneal health24,27. Recently, the change in this parameter was assessed during accommodation, in connection with phacoemulsification, refractive surgery, keratoconus and anatomical deformations28,29,30,31. No longitudinal studies determined age-related changes in corneal volume in a healthy cohort so far. In the present study we found an age-dependent decrease in corneal volume of the central 10 mm. Interestingly the change was more pronounced in case of higher baseline values and younger individuals. This change is very similar to that observed with corneal thickness however their reason is still largely unknown24. The thinner cornea in line with the higher degree of rigidity in older aged patients might be a hint of physiologically cross linking process in elderly individuals. Investigation of the age-related, long-term changes of corneal rigidity including corneal hysteresis and corneal resistance factor together with the changes of Pentacam parameters could extend our knowledge on corneal physiology and could help to understand the underlying processes. Nevertheless, some authors failed to find a significant change in CCT over a decade13,18. It is to be mentioned that central and minimum corneal thickness values are clinically relevant. The former has an impact on the precise intraocular pressure value mainly in adults, while minimum corneal thickness has an importance during the accurate evaluation of corneal ectatic disorders. Therefore, physiological age-dependent decrease of these parameters should be considered when evaluating the progression of corneal ectatic disorders. We must aim to reliably predict progression and monitor the effectiveness of corneal cross-linking treatment in corneal ectatic disorders taking normal age-related cornea changes into account.
We have found that both keratometric values (K1 and K2) on the anterior corneal surface decreased significantly during follow-up, while K max remained stable. Adjusted statistical analysis of our data revealed that anterior surface keratometric values decrease stronger in younger than in older subjects. On the other hand, higher K values proved to be more stable over time independent of age. In a middle-aged to older population sample in a longitudinal study, K max increased 0.38 Diopters (p < 0.001) in 5 years32. In contrast with these results, Orucoglu et al. reported a significant positive correlation between anterior K1 and age, without any correlation between K2 and age24. In another cross-sectional study, no significant correlations were revealed between anterior keratometry and age10. These controversial results are possibly due to differences in study design, sample size and in age of participants. In earlier studies, a significant negative correlation was reported between posterior K1 and age24 and a significant positive correlation was revealed between posterior K2 and age10. In our study, unadjusted analysis shows no significant changes in K1 and K2 values of the posterior surface. However, adjusted statistical modeling revealed that the rate of change of keratometric values of the posterior corneal surface in the flat axis (K1B) may vary with baseline value and age. Low-range keratometric values increase significantly with time, while those in the high range do the opposite, suggesting a tendency for values to progress away from distributional extremes.
It is important to investigate corneal astigmatism with highly repeatable and reproducible methods such as Scheimpflug imaging to provide reliable data on age-related changes of astigmatism in order to improve long-term outcomes after intraocular lens implantation and refractive surgery33,34,35. Previous reports on age-related changes in astigmatism were all cross-sectional studies8,9,10,24 and/or were performed with other devices6,7,36. Total refractive astigmatism has been shown to change from with-the-rule to against-the-rule with age4,7,24,32,36. According to Ho et al. and Nemeth et al. who both used Pentacam8,10 there is an age-related shift towards against-the-rule and with-the-rule astigmatism for the anterior and posterior corneal surfaces, respectively. To the best of our knowledge, the current study is the first longitudinal study in the literature examining age-related changes of keratometric astigmatism at both the anterior and posterior surfaces of the cornea. Moreover, we examined keratometry values in a population covering the widest age range reported so far. In a cross-sectional and a longitudinal study alike, the prevalence of astigmatism increased with age6,7 however, in other cross-sectional studies it was demonstrated that keratometric astigmatism decreases significantly at both the anterior and posterior surfaces of the cornea with age9,24. Our findings are similar to these, although we only found evidence for keratometric astigmatism at the posterior surface to decrease significantly (p = 0.02), while astigmatism remained stable at the anterior surface. Moreover, posterior astigmatism showed a baseline-dependent significant increase from lower and a significant decrease from higher initial values, with no evidence of heterogeneity across baseline age (Fig. 2). Our findings are in contrast with the conclusions of Németh et al. that the posterior surface of the cornea is much more stable with advancing age than the anterior surface, even though there are no differences between the two studies in ethnic composition or in methods used10. Over time, the mean flat axis angle of the posterior keratometry shifted towards horizontal from a vertical (p = 0.004) or oblique (p = 0.004) baseline, which is in line with earlier studies proving that anterior corneal topographic astigmatism drifted from with-the-rule to against-the-rule astigmatism in older subjects4,6,7,8,24.
Vector analysis allows for a complete description of astigmatism characteristics11. In the assessment of anterior surface power vectors, Jackson’s cross cylinder power vector component at 45° showed significant changes with advancing age (unadjusted p = 0.047), which were explained by a substantial increase in older subjects with low to mid-range initial J45 values; values in younger subjects and in those with mid to high-range baseline readings did not change with advancing age (Fig. 2). Our findings are consistent with previous results that in addition to the frontal astigmatism, the J0 vector also remains stable with age. Based on our study with almost four years of mean follow-up, the axis of anterior astigmatism did not change significantly. In summary, our observations support the idea and have clinical relevance, because age-related changes of the anterior and posterior corneal surfaces should be considered when planning a surgical procedure for astigmatism correction10. Still, further longitudinal studies are needed to explore the true mechanism and effects of this phenomenon.
Age-specific changes of indices obtained with Pentacam have not been reported so far. Although they only give auxiliary information about the cornea, it is noteworthy that the indices of surface variation (ISV) and vertical asymmetry (IVA) did not seem to change during follow-up, but those of height asymmetry (IHA) and height decentration (IHD) increased significantly. The changes of these indices occurred in less than four years, with no evidence for heterogeneity across their baseline values.
Limitations of this study include a modest sample size precluding robust conclusions and the fact that only European descent of low refractive error (<1.5 diopters) were included. We do not know at this time, whether the changes observed in our study are linear with age. Moreover, because patients with high refractive error were excluded, we cannot estimate the effect of refractive surgery on the outcomes over decades. Despite these limitations, it is important to emphasize that our results highlight the fact that K1F, K2F, K1B, AstigB, PachyMin, and CV decreased significantly, IHA, IHD, and J45 vector increased significantly, and the mean AxisB shifted significantly with age.
The strength of our longitudinal study is that it gives reliable, reproducible data obtained with a Pentacam HR device33,34,35. Moreover, the study group consisted of 14 to 67-year-old individuals providing a wide age range to estimate age-dependent changes associating to different baseline ages. We explored for the first time that age and baseline value of corneal parameters have an effect on age-dependent corneal changes. To the best of our knowledge, this is the first prospective longitudinal study with a long follow-up period that reveals the clinically relevant consequences of aging on multiple parameters of the healthy cornea measured with Pentacam. Notably, this is the first longitudinal analysis showing that corneal thickness and volume reduce with age dependent on baseline thickness and baseline age. In conclusion, the results of our study add to existing knowledge on age-dependent changes of the anterior and posterior corneal surfaces. We demonstrate for the first time in the literature that age and baseline value may predict the direction and size of keratometric changes. Further longitudinal Pentacam studies with larger samples including high refractive errors and longer follow-up periods are required to validate our findings, and to confirm the clinical importance of changes of various parameters in refractive surgery, intraocular lens implantation, and also in the progression of corneal ectatic disorders.
References
Faragher, R. G. et al. Aging and the cornea. Br. J. Ophthalmol. 81, 814–817 (1997).
Salvi, S. M., Akhtar, S. & Currie, Z. Ageing changes in the eye. Postgrad. Med. J. 82, 581–587 (2006).
Rao, S. N. et al. Effect of age on the refractive outcome of myopic photorefractive keratectomy. J. Cataract Refract. Surg. 26, 543–546 (2000).
Hayashi, K., Hayashi, H. & Hayashi, F. Topographic analysis of the changes in corneal shape due to aging. Cornea 14, 527–532 (1995).
Thibos, L. N., Wheeler, W. & Horner, D. Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom. Vis. Sci. 74, 367–375 (1997).
Gudmundsdottir, E. et al. With the rule 394 astigmatism is not the rule in the elderly. Reykjavik Eye Study: a population 395 based study of refraction and visual acuity in citizens of Reykjavik 50 years 396 and older. Iceland-Japan Co-Working Study Groups.Acta Ophthalmol. Scand. 78, 642–646 (2000).
Asano, K. et al. Relationship between astigmatism and aging in middle-aged and elderly Japanese. Jpn. J. Ophthalmol. 49, 127–133 (2005).
Ho, J. D., Liou, S. W., Tsai, R. J. & Tsai, C. Y. Effects of aging on anterior and posterior corneal astigmatism. Cornea 29, 632–637 (2010).
Nemeth, G. et al. Analysis of age-dependence of the anterior and posterior cornea with scheimpflug imaging. J. Refract. Surg. 29, 326–331 (2013).
Nemeth, G. et al. Evaluation of posterior astigmatism measured with Scheimpflug imaging. Cornea 33, 1214–1218 (2014).
Freitas Gde, O. et al. Astigmatic Vector Analysis of Posterior Corneal Surface: A Comparison Among Healthy, Forme Fruste, and Overt Keratoconic Corneas. Am. J. Ophthalmol. 167, 65–71 (2016).
Muir, K. W. et al. Central corneal thickness in children: stability over time. Am. J. Ophthalmol. 141, 955–957 (2006).
Aghaian, E., Choe, J. E., Lin, S. & Stamper, R. L. Central corneal thickness of Caucasians, Chinese, Hispanics, Filipinos, African Americans, and Japanese in a glaucoma clinic. Ophthalmology 111, 2211–2219 (2004).
Weizer, J. S., Stinnett, S. S. & Herndon, L. W. Longitudinal changes in central corneal thickness and their relation to glaucoma status: an 8 year follow up study. Br. J. Ophthalmol. 90, 732–736 (2006).
Brandt, J. D. et al. Ocular Hypertension Treatment Study Group. Changes in central corneal thickness over time: the ocular hypertension treatment study. Ophthalmology 115, 1550–1556 (2008).
Rieth, S. et al. Comparison of data from the rostock cornea module of the heidelberg retina tomograph, the oculus pentacam, and the endothelial cell microscope. Cornea 29, 314–320 (2010).
Viswanathan, D., Goldberg, I. & Graham, S. L. Longitudinal effect of topical antiglaucoma medications on central corneal thickness. Clin. Exp. Ophthalmol. 41, 348–354 (2013).
Hashemi, H. et al. Five year changes in central and peripheral corneal thickness: The Shahroud Eye Cohort Study. Cont. Lens Anterior Eye 39, 331–335 (2016).
Shih, C. Y., Graff, Zivin, J. S., Trokel, S. L. & Tsai, J. C. Clinical significance of central corneal thickness in the management of glaucoma. Arch. Ophthalmol. 122, 1270–1275 (2004).
Ambrósio, R. Jr., Alonso, R. S., Luz, A. & Coca Velarde, L. G. Corneal-thickness spatial profile and corneal-volume distribution: tomographic indices to detect keratoconus. J. Cataract Refract. Surg. 32, 1851–1859 (2006).
Belin, M. W., Villavicencio, O. F. & Ambrósio, R. R. Jr. Tomographic parameters for the detection of keratoconus: suggestions for screening and treatment parameters. Eye Contact Lens 40, 326–330 (2014).
Ambrósio, R. Jr. et al. Scheimpflug imaging for laser refractive surgery. Curr. Opin. Ophthalmol. 24, 310–320 (2013).
Nemesure, B., Wu, S. Y., Hennis, A. & Leske, M. C. Barbados Eye Study Group. Corneal thickness and intraocular pressure in the Barbados eye studies. Arch. Ophthalmol. 121, 240–244 (2003).
Orucoglu, F., Akman, M. & Onal, S. Analysis of age, refractive error and gender related changes of the cornea and the anterior segment of the eye with Scheimpflug imaging. Cont. Lens Anterior Eye 38, 345–350 (2015).
Hirji, N. K. & Larke, J. R. Thickness of human cornea measured by topographic pachometry. Am. J. Optom. Physiol. Opt. 55, 97–100 (1978).
Siu, A. & Herse, P. The effect of age on humancorneal thickness. Statistical implications of power analysis. Acta Ophthalmol. (Copenh.) 71, 51–56 (1993).
Sedaghat, M. R., Sharepoor, M., Hassanzadeh, S. & Abrishami, M. The corneal volume and biomechanical corneal factors: Is there any correlation? J. Res. Med. Sci. 17, 32–39 (2012).
Lipecz, A. et al. Scheimpflug image-based changes in anterior segment parameters during accommodation induced by short-term reading. Eur. J. Ophthalmol. 27, 301–307 (2017).
Ozsoy, E., Gunduz, A., Demirel, E. E. & Cumurcu, T. Evaluation of Anterior Segment’s Structures in Tilted Disc Syndrome. J. Ophthalmol. 2016, 5185207 (2016).
Cui, J. et al. Evaluation of Corneal Thickness and Volume Parameters of Subclinical Keratoconus Using a Pentacam Scheimflug System. Curr. Eye. Res. 41, 923–926 (2016).
Hashemi, M. et al. Anterior segment study with the Pentacam Scheimpflug camera in refractive surgery candidates. Middle East Afr. J. Ophthalmol. 20, 212–216 (2013).
Hashemi, H. et al. Age-Related Changes in Corneal Curvature and Shape: The Shahroud Eye Cohort Study. Cornea 34, 1456–1458 (2015).
Lackner, B. et al. Repeatability and reproducibility of central corneal thickness measurement with Pentacam, Orbscan, and ultrasound. Optom. Vis. Sci. 82, 892–899 (2005).
Aramberri, J. et al. Dual versus single Scheimpflug camera for anterior segment analysis: Precision and agreement. J. Cataract Refract. Surg. 38, 1934–1949 (2012).
McAlinden, C., Khadka, J. & Pesudovs, K. A comprehensive evaluation of the precision (repeatability and reproducibility) of the Oculus Pentacam HR. Invest. Ophthalmol. Vis. Sci. 52, 7731–7737 (2011).
Gudmundsdottir, E., Arnarsson, A. & Jonasson, F. Five-year refractive changes in an adult population: Reykjavik Eye Study. Ophthalmology 112, 672–677 (2005).
Author information
Authors and Affiliations
Contributions
G.V., D.P., Z.H. and B.L.K. carried out the experiment. G.V. wrote the manuscript with support from M.F. G.N. verified the analytical methods. All authors discussed the results. M.F. and B.L.K. conceived the original idea. M.F. and G.L. supervised the project.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vitályos, G., Kolozsvári, B.L., Németh, G. et al. Effects of aging on corneal parameters measured with Pentacam in healthy subjects. Sci Rep 9, 3419 (2019). https://doi.org/10.1038/s41598-019-39234-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-39234-x
This article is cited by
-
Analysis of corneal astigmatism and aberration in chinese congenital cataract and developmental cataract patients before cataract surgery
BMC Ophthalmology (2021)
-
Rate of central corneal thickness changes in primary angle closure eyes: long-term follow-up results
BMC Ophthalmology (2021)
-
The effects of type 2 diabetes mellitus on the corneal endothelium and central corneal thickness
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.