Abstract
In this study, using latent class analysis (LCA), we investigated whether there are any homogeneous subclasses of individuals exhibiting different profiles of metabolic syndrome (MetS) components. The current study was conducted within the framework of the Tehran Lipid and Glucose Study (TLGS), a population-based cohort including 6448 subjects, aged 20–50 years. We carried out a LCA on MetS components and assessed the association of some demographic and behavioral variables with membership of latent subclasses using multinomial logistic regression. Four latent classes were identified:(1) Low riskclass, with the lowest probabilities for all MetS components (its prevalence rate in men: 29%, women: 64.7%), (2) MetS with diabetes medication (men: 1%, women: 2.3%), (3) Mets without diabetes medication (men: 32%, women: 13.4%), (4) dyslipidemia (men: 38%, women: 19.6%). In men the forth subclass was more significantly associated with being smoker (odds ratio: 4.49; 95% CI: 1.89–9.97). Our study showed that subjects with MetS could be classified in sub-classes with different origins for their metabolic disorders including drug treated diabetes, those with central obesity and dyslipidemia associated with smoking.
Similar content being viewed by others
Introduction
Metabolic syndrome (MetS) is characterized by a clustering of various interrelated risk factors including abdominal obesity, dyslipidemia, low-HDL-cholesterol, hyper-triglyceridemia and high blood pressure; which together culminate in adverse consequences, including type 2 diabetes and cardiovascular disease (CVD). Concerns have recently been raised about the validity of diagnosis of MetS using current standard cut offs1,2. Examples of some of these uncertainties are: (1) Unknown causes of Mets while it has been originally hypothesized that insulin resistance is the underlying pathology influencing all MetS components; research has shown that not all individuals meeting criteria of MetS are insulin resistant (2) lack of experimental evidences for the cutoff points of components for MetS diagnosis; proposed MetS criteria specify different cut points for men and women regarding waist circumference and HDL cholesterol, suggesting that the risk conferred by some MetS components differs by gender, (3) considering different numbers of MetS components as a risk continuum was a more valuable risk predictor than identifying MetS, (4) unknown subclasses of MetS. Several statistical ways including factor analysis have been used in order to find underlying biology of MetS3,4. Considering the possibility that relationship among MetS components may meaningfully differ in different subclasses, LCA can identify distinct profiles of persons based on their presentation of MetS components. So, it has a person-centered approach which is concerned with the structure of groups (or cases), as oppose to factor analysis which is variable-centered i.e. it a works with correlation between variables. On the other hand, LCA includes discrete latent categorical variables with multinomial distribution, but factor analysis includes continuous latent variables with the assumption of normal distribution5.
Cluster analysis, in comparison to LCA has less robust empirically-based indices for class number decisions and quality of class solutions6. Prior methods to identify the underlying features of the MetS may not be usable foraddressing the question of whether a condition that is present or absent explains the observed manifestations of metabolic syndrome7. LCA aims to classify similar individuals into groups (or latent clusters), in which each latent cluster is viewed as consisting of homogeneous individuals with regards to the observed variables (in our case, components of MetS), and the different latent clusters are viewed as representing the unobserved heterogeneity among individuals in these observed variables8. This study aimed to examine: 1) whether there are any homogeneous subclasses of individuals exhibiting different profiles of MetS components and 2) whether there is an association between these subclasses and individual characteristics like age, education, smoking and physical activity.
Result
Men (n = 2597) had a mean (SD) age of 34.2(8.2) years and 32% of them were smokers; corresponding values were 33.9(8.40) and 4.2% in women (n = 3851). Proportions of men and women with each metabolic syndrome component are shown in Table 1. The results show that except HDL, the prevalence of all MetS components was more common in men than women.
Number of latent clusters
A four-class basic model considered as optimal had the highest entropy of 0.74 with a better interpretation compared to others (Supplementary Table 1). Table 2 shows the conditional probabilities of a “Yes” response (item response probabilities) to MetS components. These probabilities form the basis for interpretation and labeling of the latent classes. The greater probabilities appear in bold font, to highlight the overall pattern. The largest class (low risk class) with the prevalence of 60.6% showed the lowest probabilities for all metabolic syndrome components and characterized by individuals who were healthy regarding MetS components except for HDL. The second latent class, (MetS with diabetes medication) with a prevalence of 1.3% was the smallest one with high probability for high glucose component (0.97) and use of glucose-lowering medications (1.00). The third latent class (MetS without diabetes medication) with prevalence of 13.7% was distinguished by high prevalence of MetS components (all item responses ≥ 0.5) except high glucose with an item response of 0.4. Individuals in this class had no medication for diabetes. The fourthclass (dyslipidemia), with a prevalence of 24.4%, was distinguished by higher probabilities of high TG (1.00) and low-HDL (0.91) (Table 2).
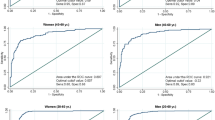
Sex differences in subclass membership
Sex was entered as a grouping variable in the LCA to establish whether the item-response probabilities are invariant across the two genders. A four-class solution was found optimal for both genders and the pattern of item response probabilities suggested identical latent class labels for males and females. We also assessed whether the prevalence of subclasses was the same or different across genders and found that overall difference in the prevalence was highly significant (p < 0.001) (Table 3). Characteristics of individuals and the proportion of the MetS components were reported for each subclass in both men and women (Table 4).
Association of covariates with latent cluster membership
A multinomial logistic regression analysis was conducted to identify predictors associated with metabolic syndrome class membership using latent class 1, low risk class, as the reference; this showed that higher age was associated with significantly higher odds of belonging to the other classes versus latent class 1 in both genders. Men in latent class 3 were more likely to have low physical activity and smoking experience than those in the latent class 1. Being a current smoker was associated with significantly higher odds of belonging to the latent class 4 compared to latent class 1 (OR = 4.49 for men). Compared to the latent class 1, women in the latent class 2 were more likely to be current smoker (Table 5). We did additional analysis onlyonparticipants with available insulin data (n = 2785) and showed that increasing HOMA-IR was significantly associated with both MetS subclasses (Table 6). However, considering latent class 2 (MetS with diabetes medication) as the reference group showed that with 1 SD increase in HOMA-IR, the odds for being classified into class 3 (MetS without diabetes medication) was 23% lower than the odds for being classified into class 2 (MetS with diabetes medication) in men; the corresponding value was 19% in women (OR = 0.67, 95% CI 0.52–0.88 in men and 0.81, 0.65–1.01 in women) (Table 6).
Discussion
The person-centered analytic approach of LCA sought to improve the comprehension of metabolic syndrome, by identifying latent classes based on MetS component patterns. Considering clustering of MetS components can be an effective approach in preventive strategies. Some studies emphasized the clustering and combining patterns of MetS components7,9. LCA revealed four distinct subclasses of MetS among an Iranian population, aged 20–50 years: (1) low risk, (2) MetS with diabetes medication, (3) MetS without diabetes medication, (4) dyslipidemia.
Clinicians believe that risk factors of cardiovascular disease tend to accumulate, and thus the risk of developing cardiovascular disease increases along with increments in their clustering abilities10,11. Findings of our study demonstrate that two latent classes (the second and third) were consistently associated with many features of Mets; these latent classes may demonstrate a specific clinical situation generating the observed features of MetS. Our results indicate this clustering of MetS components in two different patterns. The second latent class was more relevant to the insulin resistance.
Longitudinal studies have shown that there are different risks of mortality following the different combination of MetScomponents12,13; our results showed different combination pattern of Mets components as well. For example, in the combination of MetS components among individuals of latent class 3, we found out that the high glucose component haslimited role in the concept of MetS. Based on these patterns, the individuals of latent classes 2 and 3 probably have different chance of developing complications of metabolic syndrome.
The prevalence of each subclass differed between men and women, although both genders had the same number of latent classes and the same item response probabilities. Age, education, low physical activity and smoking status were somehow correlated with MetS latent class membership. The LCA method produces estimates of conditional probabilities indicating the association between the observed measures and latent classes. In our analysis, latent class 1, the largest group, characterized by very low association with all MetS components. Latent class 2 was strongly associated with high glucose and glucose-lowering medications and was also related to the other Mets components, possiblyrepresenting a pathophysiologic state producing the observed components of the Mets7. Since insulin resistance is supposed to be the core of MetS14,15,16, the latent class 2 could be a good surrogate forthisdefinition. The latent class 3 was also related to all MetS components with response item probability >0.5 except for the high blood glucose component; additional analysis showed that the association of insulin resistance with this class is lower than that with latent class 2. None of individuals in this subclass used diabetes medication, a finding contrary to the insulin resistance hypothesis for MetS, which may show that some people with MetS have other origins for their MetS components17,18. Obesity can be a good explanation for developing MetS in latent class 3 because body fat, not insulin resistance, can be an inflammatory cardio metabolic risk marker. In our study, individuals in the MetS without diabetes medication subclass were more obese than other groups, with a response item probability of 0.65 for the high waist component.
Latent class 4 was associated mainly with low HDL and elevated triglycerides, but had a weak association with other Mets components. We know that low HDL and high TG are metabolically linked and TG/HDL is an independent risk factor for cardiovascular diseases19. Since smoking has a strong association with latent class 4, it seems that this subclass mostly includes smokers, with a low prevalence of obesity, compared to other high risk sub groups (latent classes 2 and 3); there was stronger association between this group and smoking (OR = 4.5) compared to others (OR = 2.3) in our male population. Previous studies have confirmed the association between smoking and dyslipidemia20,21. It needs to be mentioned that the prevalence of smoking was very low in our female population.
Sex differences in the prevalence of latent class 3 were striking, with almost twice as many men in this subclass. Results indicated higher proportion of women (64.4%) classified into the latent class 1 compared to men (29%). Latent class 1 was the most prevalent subclass in women but was the ranked third among men. The differences in the subclass prevalence between women and men is consistent with men having a higher risk of MetS than women, a finding contrary to national MetS prevalence estimates, with higher prevalence of MetS in women (32.9%) compared to men (22.9%) and European data, i.e. 10% in men and 13% in women22. Although previous studies in the TLGS confirm the prevalence of MetS as being higher in females23,24, the difference between their results and ours could be due to the age distribution. Since mean age for menopause is 50 years in Iranian women25, most of our female participants were not menopausal.
MetS subclasses were identified related to the covariates in a manner consistent with previous researches. Smokers had higher odds of being classified into latent class 2, latent class 3 and latent class 4 compared to those in latent class 1, with high significance for latent class 4 in men and latent class 2 in women. These results are consistent with those reported by Yankey et al. who found that smoking was significantly associated with increased odds of hypertension and hyperglycemia after adjusting for confounders26. Other studies have also reported a strong association between smoking and dyslipidemia20,21,27. Both men and women with low physical activity were more likely to be in the latent class 3 than in the latent class 1. Meta-analyses of prospective cohort studies conducted on. individuals from different populations reported that a high level of leisure time physical activity was statistically associated with decreased risk of the MetS28; findings also reported in another short term study conducted among Korean male workers29. Older men and women weremore likely to belong to the three classes than latent class 1; the odds favoring metabolic syndrome significantly increased with age, and decreased with education level30. Twoprevious studies showed a higher prevalence of MetS in elderly subjects and a larger number of component clustering of the syndrome in elderly patients, compared with younger patients31,32.
Overall, clustering of components of MetS can be helpful and valuable in reinforcing the hypothesis that different pathophysiological mechanisms are engaged in this process. The most important finding in our study is that among individuals of latent classes of 2 and 3, some of the Mets components did not play an influential role (e.g. of latent class 2 “high blood pressure” and “high waist”; of latent class3 “high glucose”). This results are consistent with previous studies33,34.
Women in low risk group had a very high prevalence of low HDL (65%), while the prevalence of other MetS components was very low in women. Previous studies showed that the low HDL cholesterol is the most common metabolic abnormality in the Middle East including Iran, especially in women35,36. Among Iranian women aged 25–64 years, the prevalence of low HDL cholesterol is 84%36 which is so different from western countries37. The amount of low HDL cholesterol is low even in people without metabolic syndrome38. In our study the low risk group had the lowest prevalence of low HDL cholesterolamong all subclasses.
The most important short comings of LCA are that it can detect an unobserved structure only if each of its classes is large enough to be detected. Detecting rare latent classes would be difficult when sample size decreases. Another limitation of LCA is due to the temptation to attach too much meaning to a latent class and reification of the labels assigned to each class for easier interpretation39. As another limitation in our study, changing cut off points for defining MetS components may results in different LCA outputs. Furthermore, behavioral changes among people over time may also change the subclasses identification. Considering young and midlife adults, before menopause age, allows the results to be comparable between both genders. On the other hand, we selected this age range to avoid the effect of co-morbidities and medications on the results. Although this age range increases the internal validity of the results, it may decrease their external validity. Our study has several strengths. (1) Using a new approach to classify high risk people based on their observed cardio metabolic risk factors. (2) We used a large sample size. (3) Utilizing community-based data from the TLGS, although this sample is not nationally representative and inferences cannot be extended to the other communities especially rural populations.
Conclusion
Using LCA showed that subjects with MetS could be classified in sub-classes with different origins for their metabolic disorders including drug treated diabetes, those with central obesity and dyslipidemia associated with smoking.
Methods
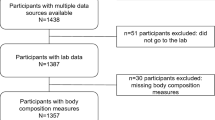
Sample
This study was conducted within the framework of the Tehran Lipid and Glucose Study (TLGS) whichis a large-scale population-based prospective cohort study with long-term follow-up, performed on a representative sample of residents of Tehran. The baseline measurements (phase 1) were performed between 1999 to 200140. For the current study, subjects aged 20–50 years were selected from the first phase (n = 6974); this range of age was used to avoid the effect of co-morbidities and menopause on our results. From these, we excluded 526 participants with missing data on MetS components, resulting in 6448 subjects. Informed written consent was obtained from all participants. The study was approved by the ethics committee of the Research Institute for Endocrine Sciences. All methods of the current study were performed in accordance with the relevant guidelines and regulations.
Measures
Measurement and definition of terms
Data were collected using interviews, physical examinations and laboratory measurements. Details of measurement of MetS components, including waist circumference (WC), fasting plasma glucose (FPG), systolic and diastolic blood pressure (SBP and DBP, respectively), high-density lipoprotein cholesterol (HDL-C), and triglycerides (TG), have been described elsewhere (12). Components of MetS were: Elevated waist circumference (≥95 cm for both Iranian men and women), elevated blood pressure (systolic/diastolic blood pressure ≥85/130 mm Hg), low HDL- cholesterol (<40 mg/dlin men and <50 mg/dlin women), elevated triglycerides (high TG) (≥150 mg/dl), and high glucose (≥100 mg/dl)41. Drug treatments including anti-hypertensive drugs, lipid medication and diabetes medication were considered as separate binary variables. Fasting serum insulin was analyzed by the electro chemiluminescence immunoassay method 42 and HOMA-IR calculated as: FPG (mmol/L) × fasting serum insulin (μU/mL)/22.5. We considered HOMA-IR more than 2.38 in men and 2.68 in women as indicating the presence of insulin resistance42. The number of participants with available insulin data was 2785 (1749 men).
Variables considered for latent class analysis
Eight dichotomous observable variables, including high glucose, low HDL, high WC, high TG, high blood pressure and drug treatments including anti hypertension, lipid medication and diabetes medication were considered forthe latent class analysis. All definitions of variables are based on the cut points defined for the metabolic syndrome definition43,44.
Consideration of sex in the LCA
In previous studies the prevalence of MetS differed by gender4. We evaluated: (1) whether men and women experienced the same number and prevalence of MetS subclasses. (2) Whether the item response probabilities differ across genders.
Measurement of covariates
We considered demographic and lifestyle variables as correlates of the MetS subclass membership: Age (years), smoking (current vs. never or past smoker), education (categorized as ≤diploma and >diploma, with ≤diploma serving as the reference group); physical activity (those with ≥3 times a week moderate to high intensity physical activity vs. those with less than 3 times a week physical activity), marital status (married vs. single, widowed, or divorced). We did an additional analysis only for participants who had insulin data (n = 2785).
Statistical analysis
There were three analytic phases. (1) Explaining the sample and developing the LCA model. (2) Evaluating sex differences in MetS subclasses. (3) Evaluating the association between covariates and MetS subclasses.
First, summary statistics were separated by sex. We then constructed LCA models with numbers of subclasses varying from two to six. Basic models without grouping variables and covariates were fitted first to obtain a general understanding of the structure of the subclasses. These models were examined for fit, parsimony and interpretability of the observed variables. Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), entropy, sample size Adjusted Bayesian Information Criteria (ABIC)45, adjusted LMR LR (ALMR LR) test, and interpretability of competing solutions were considered to select the model with the optimal number of MetS latent classes. Larger entropy and lower AIC and BIC values indicated better fitting solution. A significant P-value of the LMR LR test (P < 0.05) indicates a significant improvement in this model fit in the k-class model compared with the (k-1) class model46.
Second, optimal number of latent classes was selected for the basic model and the model was stratified by sex as a grouping variable to see whether the number of latent subclasses was identical between men and women. We found that the number of latent subclasses and item –response probabilities were identical between men and women. However, the prevalence of sub types was different across genders. As a result, measurement invariance doesn’t hold across genders for the prevalence of sub types45.
Finally, we evaluated the association between subclasses of MetS and demographic or lifestyle covariates. Low risk class served as the reference group to facilitate interpretation. Odds ratios were calculated to show the odds of being in each class, compared to being in the reference. Analyses were conducted using LCA Stata Plugin Users’ Guide Version 1.2.1 and Mplus version 5.
References
Mottillo, S. et al. The metabolic syndrome and cardiovascular risk: a systematic review and meta-analysis. Journal of the American College of Cardiology 56, 1113–1132 (2010).
De Zeeuw, D. & Bakker, S. J. Does the metabolic syndrome add to the diagnosis and treatment of cardiovascular disease? Nature Clinical Practice Cardiovascular Medicine 5, S10–S14 (2008).
Kahn, R., Buse, J., Ferrannini, E. & Stern, M. The metabolic syndrome: time for a critical appraisal Joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes care 28, 2289–2304 (2005).
Arguelles, W. et al. Characterization of metabolic syndrome among diverse Hispanics/Latinos living in the United States: Latent class analysis from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). International journal of cardiology 184, 373–379 (2015).
Meeusen, C., Meuleman, B., Abts, K. & Bergh, R. Comparing a Variable-Centered and a Person-Centered Approach to the Structure of Prejudice. Social Psychological and Personality Science, 1948550617720273 (2017).
Magdison, J. & Vermunt, J. K. A Nontechnical Introduction to Latent Class Models. White Paper, Tilburg: Statistical Innovations (2002).
Boyko, E. J. et al. Latent class analysis of the metabolic syndrome. Diabetes research and clinical practice 89, 88–93 (2010).
Vermunt, J. K. & Magidson, J. Latent class cluster analysis. Applied latent class analysis 11, 89–106 (2002).
Pimenta, A. M., Felisbino-Mendes, M. S. & Velasquez-Melendez, G. Clustering and combining pattern of metabolic syndrome components in a rural Brazilian adult population. Sao Paulo Medical Journal 131, 213–219 (2013).
Genest, J. Jr. & Cohn, J. S. Clustering of cardiovascular risk factors: targeting high-risk individuals. The American journal of cardiology 76, 8A–20A (1995).
Katakami, N. et al. Clustering of several cardiovascular risk factors affects tissue characteristics of the carotid artery. Atherosclerosis 198, 208–213 (2008).
Guize, L. et al. All-cause mortality associated with specific combinations of the metabolic syndrome according to recent definitions. Diabetes care (2007).
Hong, Y. et al. Metabolic syndrome, its preeminent clusters, incident coronary heart disease and all‐cause mortality–results of prospective analysis for the Atherosclerosis Risk in Communities study. Journal of internal medicine 262, 113–122 (2007).
Grundy, S. M. Hypertriglyceridemia, insulin resistance, and the metabolic syndrome. The American journal of cardiology 83, 25–29 (1999).
Ferrannini, E., Haffner, S., Mitchell, B. & Stern, M. Hyperinsulinaemia: the key feature of a cardiovascular and metabolic syndrome. Diabetologia 34, 416–422 (1991).
Taniguchi, C. M., Emanuelli, B. & Kahn, C. R. Critical nodes in signalling pathways: insights into insulin action. Nature reviews Molecular cell biology 7, 85–96 (2006).
Karnchanasorn, R., Ou, H.-Y., Chuang, L.-M. & Chiu, K. C. Insulin resistance is not necessarily an essential element of metabolic syndrome. Endocrine 43, 92–99 (2013).
Escobar-Morreale, H., Villuendas, G., Botella-Carretero, J., Sancho, J. & San Millan, J. Obesity, and not insulin resistance, is the major determinant of serum inflammatory cardiovascular risk markers in pre-menopausal women. Diabetologia 46, 625–633 (2003).
Hadaegh, F. et al. Triglyceride/HDL-cholesterol ratio is an independent predictor for coronary heart disease in a population of Iranian men. Nutrition, Metabolism and Cardiovascular Diseases 19, 401–408 (2009).
Kelishadi, R. et al. Are active and passive smoking associated with cardiometabolic risk factors in adolescents? The CASPIAN-III Study. Paediatrics and international child health, 1–8 (2016).
Erem, C., Hacihasanoglu, A., Deger, O., Kocak, M. & Topbas, M. Prevalence of dyslipidemia and associated risk factors among Turkish adults: Trabzon lipid study. Endocrine 34, 36–51 (2008).
Isomaa, B. et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes care 24, 683–689 (2001).
Hadaegh, F. et al. Prevalence of metabolic syndrome by the Adult Treatment Panel III, International Diabetes Federation, and World Health Organization definitions and their association with coronary heart disease in an elderly Iranian population. Annals Academy of Medicine Singapore 38, 142 (2009).
Zabetian, A., Hadaegh, F. & Azizi, F. Prevalence of metabolic syndrome in Iranian adult population, concordance between the IDF with the ATPIII and the WHO definitions. Diabetes research and clinical practice 77, 251–257 (2007).
Shobeiri, F. & Nazari, M. Age at menopause and its main predictors among Iranian women. Cell J (Yakhteh) 8 (2014).
Yankey, B. N., Strasser, S. & Okosun, I. S. A cross-sectional analysis of the association between marijuana and cigarette smoking with metabolic syndrome among adults in the United States. Diabetes & Metabolic Syndrome: Clinical Research & Reviews (2016).
Wang, C.-J. et al. Development and evaluation of a simple and effective prediction approach for identifying those at high risk of dyslipidemia in rural adult residents. PloS one 7, e43834 (2012).
He, D. et al. Association between leisure time physical activity and metabolic syndrome: a meta-analysis of prospective cohort studies. Endocrine 46, 231–240 (2014).
Ryu, S. et al. Incidence and risk factors for metabolic syndrome in Korean male workers, ages 30 to 39. Annals of epidemiology 17, 245–252 (2007).
Santos, A. C., Ebrahim, S. & Barros, H. Gender, socio-economic status and metabolic syndrome in middle-aged and old adults. BMC Public Health 8, 62 (2008).
Gharipour, M. et al. Effect of age on the phenotype of metabolic syndrome in developing country. Advanced biomedical research 4 (2015).
Kraja, A. T. et al. Longitudinal and age trends of metabolic syndrome and its risk factors: the Family Heart Study. Nutrition & metabolism 3, 1 (2006).
Abbasi-Ghahramanloo, A., Soltani, S., Gholami, A., Erfani, M. & Yosaee, S. Clustering and combining pattern of metabolic syndrome components among Iranian population with latent class analysis. Medical journal of the Islamic Republic of Iran 30, 445 (2016).
Riahi, S. M. et al. Patterns of clustering of the metabolic syndrome components and its association with coronary heart disease in the Multi-Ethnic Study of Atherosclerosis (MESA): A latent class analysis. International journal of cardiology (2018).
Azizi, F., Salehi, P., Etemadi, A. & Zahedi-Asl, S. Prevalence of metabolic syndrome in an urban population: Tehran Lipid and Glucose Study. Diabetes research and clinical practice 61, 29–37 (2003).
Delavari, A., Forouzanfar, M. H., Alikhani, S., Sharifian, A. & Kelishadi, R. The First nationwide study of the prevalence of the metabolic syndrome and optimal cut-off points of waist circumference in the middle east: the national survey of risk factors for non-communicable diseases of Iran. Diabetes care (2009).
Azimi-Nezhad, M. et al. High prevalence of metabolic syndrome in Iran in comparison with France: what are the components that explain this? Metabolic syndrome and related disorders 10, 181–188 (2012).
Hadaegh, F., Shafiee, G., Ghasemi, A., Sarbakhsh, P. & Azizi, F. Impact of metabolic syndrome, diabetes and prediabetes on cardiovascular events: Tehran lipid and glucose study. Diabetes research and clinical practice 87, 342–347 (2010).
Schulenberg, J. & Schoon, I. The transition to adulthood across time and space: Overview of special section. Longitudinal and Life Course Studies 3, 164 (2012).
Azizi, F. et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials 10, 5 (2009).
Azizi, F. et al. Appropriate definition of metabolic syndrome among Iranian adults: report of the Iranian National Committee of Obesity. Archives of Iranian Medicine 13, 426 (2010).
Tohidi, M. et al. Age-and sex-specific reference values for fasting serum insulin levels and insulin resistance/sensitivity indices in healthy Iranian adults: Tehran Lipid and Glucose Study. Clinical biochemistry 47, 432–438 (2014).
Cheţa, D. M. The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes: response to Kahn et al. Diabetes care 29, 176–177 (2006).
Kahn, R., Buse, J., Ferrannini, E. & Stern, M. The metabolic syndrome: time for a critical appraisal. Diabetologia 48, 1684–1699 (2005).
Collins, L. M. & Lanza, S. T. Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. Vol. 718 (John Wiley & Sons, 2013).
Wang, J. & Wang, X. Structural equation modeling: Applications using Mplus. (John Wiley & Sons, 2012).
Acknowledgements
This work was derived from Noushin Sadat Ahanchi’s MSc thesis in Department of Epidemiology, School of Public Health, Shahid Beheshti University of Medical Sciences and was supported by Prevention of Metabolic Disorders Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences. The authors appreciate the contribution by investigators, staff, and participants of the TLGS. The authors also wish to acknowledge Ms Niloofar Shiva for critical editing of English grammar and syntax of the manuscript. No funding received.
Author information
Authors and Affiliations
Contributions
Design: Noushin Sadat Ahanchi, Davood Khalili, Fereidoun Azizi, Arash Ghanbarianh. Conceptualization: Noushin Sadat Ahanchi, Davood Khalili, Abbas Alipour, Farzad Hadaegh. Data cleaning: Noushin Sadat Ahanchi. Data management: Davood Khalili, Arash Ghanbarian. Statistical analysis: Noushin Sadat Ahanchi. Statistical inference: Noushin Sadat Ahanchi, Davood Khalili, Farzad Hadaegh. Project administration: Davood Khalili, Fereidoun Azizi. Supervision: Fereidoun Azizi, Farzad Hadaeg. Writing ± original draf: Noushin Sadat Ahanchi, Davood Khalili, Farzad Hadaegh. Writing ± review & editing: Noushin Sadat Ahanchi, Davood Khalili, Abbas Alipour, Farzad Hadaegh, Arash Ghanbaria, Fereidoun Azizi. All authors participated in revision of draft manuscript and agreed to the final content.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahanchi, N.S., Hadaegh, F., Alipour, A. et al. Application of Latent Class Analysis to Identify Metabolic Syndrome Components Patterns in adults: Tehran Lipid and Glucose study. Sci Rep 9, 1572 (2019). https://doi.org/10.1038/s41598-018-38095-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-38095-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.