Abstract
The law of least mental effort states that, everything else being equal, the brain tries to minimize mental effort expenditure during task performance by avoiding decisions that require greater cognitive demands. Prior studies have shown associations between disruptions in effort expenditure and specific psychiatric illnesses (e.g., schizophrenia and depression) or clinically-related symptoms and traits (e.g., anhedonia and apathy), yet no research has explored this issue transdiagnostically. Specifically, this research has largely focused on a single diagnostic category, symptom, or trait. However, abnormalities in effort expression could be related to several different psychiatrically-relevant constructs that cut across diagnostic boundaries. Therefore, we examined the relationship between avoidance of mental effort and a diverse set of clinically-related symptoms and traits, and transdiagnostic latent factors in a large sample (n = 811). Only lack of perseverance, a dimension of impulsiveness, was associated with increased avoidance of mental effort. In contrast, several constructs were associated with less mental effort avoidance, including positive urgency, distress intolerance, obsessive-compulsive symptoms, disordered eating, and a factor consisting of compulsive behavior and intrusive thoughts. These findings demonstrate that deviations from normative effort expenditure are associated with a number of constructs that are common to several forms of psychiatric illness.
Similar content being viewed by others
Introduction
Each day we are faced with tasks that require mental effort. The level of effort depends on the difficulty of achieving the desired goal. Given that mental effort is a critical part of daily life, understanding the role of mental effort in psychopathology may provide key insights into psychiatric conditions that show deviations from exerting effort towards adaptive behavior. For example, drug seeking or compulsivity can be thought of as exercising effort towards the wrong goal. For individuals who become addicted to drugs, effort manifests as motivated planning to offset cravings; and similarly, counting in OCD is aimed at immediately reducing feelings of distress. Meanwhile, symptoms such as anhedonia and avolition can be thought of as a failure of effort exertion. Elevations in apathy are associated with a lack of interest, and likewise, avolition is a deficit in the initiation of self-directed and purposeful activities.
A number of studies have demonstrated that decision making that requires mental effort is disrupted in clinical populations with diagnoses of schizophrenia and depression (for a review, see Culbreth, Moran, & Barch, 2017) and in symptoms or personality traits such as anhedonia1,2 and apathy (for a recent review, see Le Heron, Apps, & Husain3). It has been argued these disruptions are due to abnormalities in the processes underlying the expenditure of effort4,5 (e.g., cognitive control, cost-benefit evaluations, and/or reward responsivity). Moreover, irregularities in these processes are putatively associated with a range of clinical diagnoses. However, these prior studies have focused on examining associations between effort-based decision making and specific clinically-related constructs or diagnoses, tying disrupted effort onto a single measure or diagnostic group. The limitation of this approach is that effort disruptions are not localized to a single diagnosis or construct, but are often associated with several symptoms and traits that cut across diagnostic boundaries.
We overcome the limitations of examining effort expenditure in a single psychological construct or diagnostic group by taking a dimensional approach to psychopathology in a large sample6,7,8. We measure several symptoms and traits, and obtain transdiagnostic latent factors to investigate associations between a well-defined measure of mental effort9, and several psychiatric constructs that transverse psychopathology.
Among the multiple ways to examine mental effort, one approach is to focus on people’s tendency to minimize effort expenditure (law of least mental effort). This idea is borrowed from a fundamental principle underlying most theories of physical effort, that people seek to minimize physical demands10. Preliminary evidence for the law of least mental effort comes from Tversky & Kahneman’s research11, which suggests that people use heuristics and other strategies to minimize cognitive demands. Recently, Kool and colleagues9 provided the first direct evidence for the principle of mental effort minimization in a novel paradigm called the demand selection task (DST). In this task, participants freely choose between two options that demand differing levels of mental effort. The high-demand option requires increased mental effort in the form of frequent task switching12, whereas the low-demand option necessitates less frequent task switching. Across many replications of this task, participants tend to prefer the less demanding course of action9,13,14. This avoidance of cognitive demand is consistent with the law of least mental effort9,15.
The DST differs from other effort paradigms in several key ways. First, in both the EEfRT1 (Effort Expenditure for Rewards Task) and COGED16 (Cognitive Effort Discounting) tasks the level of effort required for each choice is explicitly stated. In contrast, the DST requires participants to learn the difference in effort required between the low- and high-demand options, and therefore individual variability in effort expression may reflect variability in the learning process. Second, a number of effort paradigms1,16,17,18,19 provide rewards for greater effort exertion, whereas the DST does not provide rewards. Therefore, the DST may represent an individual’s preferred level of effort independent of a reward structure. Finally, the DST is specific to mental effort, whereas other paradigms measure physical effort with repeated finger presses1,18 or grip strength19. The differences between the DST and other effort tasks, and the lack of transdiagnostic studies, provides a unique opportunity to take a transdiagnostic approach to the avoidance of mental effort.
In the current study, we examine the expression of mental effort across the psychopathology spectrum. In addition to measuring a broad range of symptoms and traits, we produce three transdiagnostic factors (anxious depression, compulsive behavior and intrusive thought, and social withdrawal) that have been previously shown to be relevant to psychopathology and goal-directed behaviors20,21. Combining the DST with these psychiatric factors and several psychiatrically-relevant constructs will allow us to investigate the law of least mental effort transdiagnostically. We hypothesize that several constructs will be associated with greater avoidance of mental effort because theoretical models suggest common sources of dysfunction underlying the expression of effort in psychiatric illness22,23. If we find the expression of mental effort is associated with transdiagnostic constructs, it would suggest a common source of dysfunction in the processes underlying effort expression across several clinical diagnoses.
Methods
Participants
A total of 905 participants were recruited using Amazon Mechanical Turk. The participants provided informed consent, and the study and experimental protocols followed ethical guidelines and were approved by the Committee on the Use of Human Subjects (CUHS), the Institutional Review Board (IRB) for Harvard University. Participants were required to have U.S. residency, 90% approval rating, and 100 completed Mechanical Turk Human Intelligence Tasks. The study was completed over two sessions, and included the DST9, an adaptive IQ test20,24, nineteen self-report measures, and a sequential decision making task21,25. Participants were compensated $20. Exclusions included current drug and/or alcohol intoxication (n = 3) and demonstrated non-adherence on the IQ test (n = 72) and/or DST (n = 19). The IQ test questions became increasingly easier with incorrect responses, therefore participants with decreasing IQ scores indicated non-adherence or random responding. Participants endorsing mental health diagnoses were not excluded at a higher rate than those without (see Supplemental). The final sample included 811 participants that were 47.9% female and 52.1% male, ranged in age from 18–73 years old (M = 34.9, SD = 10.2) and had an average IQ of 99.1 (SD = 9.7). Participants were 78.4% Caucasian, 8.8% Black/African American, 6.2% Hispanic/Latino, 6.0% Asian/Asian American, and 0.5% Native American/Other. Table 1 contains self-reported clinical diagnostic and treatment information.
Self-report measures
Table 2 provides definitions and sources for nineteen psychiatric constructs from self-report measures completed by the participants. In a separate but related project on sequential decision making and psychopathology21, we replicated and extended the findings of Gillan and colleagues20 using overlapping self-report measures. Like these former studies, nine of the self-report measures in the current study can be summarized with three latent factors (anxious depression, compulsive behavior and intrusive thought, and social withdrawal). We generated the scores for these factors using the factor loadings from Gillan and colleagues20. The measures included in these factors are: Apathy Evaluation Scale26, trait portion of the State-Trait Anxiety Inventory27, Alcohol Use Disorders Identification Test28, Barratt Impulsiveness Scale-1129, Zung Depression Scale30, Eating Attitudes Test31, Obsessive-Compulsive Inventory-Revised32, Short Schizotypy Scale33, and Social Anxiety Scale34.
We measured ten additional constructs because they encompass personality traits (i.e., intolerance of uncertainty, rumination, emotion dysregulation, distress intolerance, impulsivity) that underlie prominent theories of psychiatric illness. These measures were, the Intolerance of Uncertainty Scale35, Anxiety Sensitivity Index-336, Ruminative Response Scale37, Difficulties with Emotion Regulation Scale38, Distress Tolerance Scale39, and the UPPS-P Impulsivity Scale40,41,42 (the UPPS-P is comprised of positive & negative urgency, sensation seeking, lack of premeditation, and lack of perseverance). We did not conduct a factor analysis with these measures because the sample size is underpowered and we sought to stay consistent with Patzelt and colleagues21.
Demand selection task
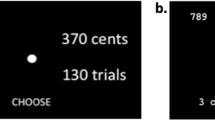
The study used an abridged version of the DST first reported in Experiment 3 of Kool and colleagues9 and also used in Experiment 1 of Gold and colleagues (2014), and it was adopted for use on Mechanical Turk (https://github.com/wkool/demandavoidance). In this paradigm, the participant is presented with two abstract color patches representing the cues (Fig. 1). The participant chooses a cue, and a probe appears as a blue or yellow number between 1 and 9. Participants were instructed to make a parity judgment on yellow numbers (i.e., odd or even) or a magnitude judgement on blue numbers (i.e., >5 or <5).
Demand selection task. The participant is presented with the choice between two abstract patches representing the cues. A probe appears as a colored number following cue selection, and the participant responds with a parity judgement on yellow numbers (e.g., odd or even), or magnitude judgement on blue numbers (e.g., <5 or >5). Note, the magnitude and parity rules are displayed above, but not visible to the participant during the task. The top cue is the high demand option and requires frequent task switching between parity and magnitude judgements (i.e., 90% of the time; high mental effort). The bottom cue is the low demand option and requires infrequent task switching between parity and magnitude judgements (i.e., 10% of the time; low mental effort). Participants completed 300 trials across 4 blocks and 4 different cue pairs.
One cue represented the high-demand option, whereas the other represented the low-demand option. When choosing the high-demand option over several trials, the participant would be required to switch tasks between parity and magnitude judgments 90% of the time. Alternatively, when choosing the low-demand option consistently over several trials, the participant would be required to switch tasks between parity and magnitude judgements 10% of the time. Thus, the high-demand option required more task switching relative to the low-demand option, and therefore greater cognitive effort9,12,43.
There were three rounds of training where participants first practiced 10 trials making parity or magnitude judgements with accuracy feedback on every trial. Next, participants completed 10 trials with feedback at the end, to ensure the correct response mappings. Finally, participants practiced 20 trials of the full task by choosing a cue and responding with a parity or magnitude judgment depending on the color of the displayed number. The participants completed 300 trials of the DST with 75 trials across 4 blocks and 4 cue pairs. The location and appearance of the cues remained fixed within block while varying across block.
Analyses
Measuring mental effort
Following prior work9, we measured the degree of demand avoidance as the proportion of trials on which participants chose the low demand cue. Accuracy was calculated separately for low demand and high demand trials. Participants were excluded (N = 19) if their overall task performance reflected random responding, which was calculated using a binomial distribution to determine the minimum number of correct responses (i.e., 165/300 trials) needed to surpass the 50% chance accuracy threshold.
Demand avoidance bias and psychiatric constructs (Bayesian regression)
Bayesian regression was used to estimate the relationship between the psychiatric constructs and demand avoidance44. This differs from frequentist approaches to linear analysis in several ways. Frequentist linear regression produces a point estimate of the regression coefficients. This is often reported in addition to 95% confidence intervals, which indicate that over many repetitions of the study, 95% of intervals will contain the population value. As noted by Baldwin & Larson45, confidence intervals are often misinterpreted as the interval that contains probable values of the beta coefficient. However, in frequentist theory, the confidence interval indicates confidence in the method (i.e., the study design) that produced the beta estimate. This point estimate is subjected to significance testing for rejection of the null hypothesis. The frequentist interpretation is binary: either there is a lack of a relationship between the predictor and the dependent variable (i.e., the null hypothesis is true), or the null hypothesis is rejected.
In contrast, Bayesian linear regression incorporates probability into the estimate of beta values for the regression coefficient. A posterior probability distribution over possible beta values is produced that can be summarized using credible intervals, indicating the concentration of betas around the mean or median. This allows us to quantify the magnitude of the effect between the psychiatric constructs and demand avoidance because we can estimate the probability that a positive or negative relationship exists (rather than accepting or rejecting the null). We report the 95% highest posterior density (HPD) interval. This indicates the range of coefficient values around the posterior mean (βmean) that contains 95% of the posterior probability density. The percentage of the posterior density that exceeds or falls below 0 indicates the probability of a positive relationship (i.e., construct is associated with more demand avoidance), or negative relationship (i.e., construct is associated with less demand avoidance). We used the brms package46 with the default prior σ ~ student-t(3,0,10) and separately regressed each self-report measure onto the proportion of low demand choices (i.e., demand avoidance) while controlling for age, IQ, and gender.
We also accounted for collinearity (correlations reported in supplemental information, Fig. S3) by entering all the self-report measures into a single regression with elastic net regularization using the caret47 and glmnet48 packages in R. The analysis used 20-fold cross-validation with 10 repeats to establish the best alpha and lambda parameters for the elastic net.
Transdiagnostic factors
We derived psychiatric factors by regressing the published factor loadings from Gillan et al.20 onto the item level scores for nine self-report measures that overlapped with their study (see Table 2). This generated individual factor scores for the participants in our study corresponding to the three psychiatric factors: anxious depression, compulsive behavior and intrusive thought, and social withdrawal. We regressed all three measures concurrently onto the proportion of low demand choices, again controlling for age, IQ, and gender.
To confirm the factor structure produced by Gillan and colleagues we performed a confirmatory factor analysis (CFA) with the lavaan package49. The latent variable definitions (e.g., anxious-depression) in the specified model describe how the factors manifest from the observed self-report items. We specified the factor structure according to the latent factor model provided by Gillan and colleagues and the fit was measured by two metrics that account for model complexity, the RMSEA and SRMR50. We then regressed the CFA loadings onto the proportion of low demand choices to establish if loadings generated solely from our data would produce similar results to the Gillan et al.20 loadings.
Results
Demand selection task
On average, participants selected the low-demand option 65% of the time (SD = 0.18; Fig. 2). A one-sample t-test showed participants significantly preferred the low-demand option over the high demand option (t(810) = 23.59, p < 0.001). Mean accuracy for the low-demand option was 0.95 (SD = 0.063) and for the high-demand option was 0.93 (SD = 0.073), and these differed significantly from each other (t(1587.3) = 5.51, p < 0.001). IQ was significantly positively correlated with demand avoidance (r(792) = 0.21, p < 0.001), indicating increasing IQ was associated with a bias towards greater demand avoidance (i.e., less mental effort). Age was uncorrelated with demand avoidance (r(792) = −0.01, p = 0.71).
Demand avoidance and self-report measures
Figure 3 shows the results of separate regressions for each self-report measure. The distance from zero of the mean beta coefficients and credible intervals indicate the magnitude of the relationship between demand avoidance and the self-report measures. Table 3 reports the posterior probability of beta less than or greater than zero. Almost the entire posterior distribution of possible betas for lack of perseverance was placed on values greater than zero (96.0% positive), indicating that the self-report measure was associated with a greater demand avoidance bias (i.e., less mental effort). Alternatively, positive urgency (1.9% positive) and distress intolerance (2.1% positive) had posterior data distributions where at least 95% of the beta estimates were negative. The obsessive-compulsive symptoms (6.2% positive), and disordered eating (8.5% positive) had posterior beta distributions where at least 90% of the beta estimates were negative, which is below the 95% HPD, yet still indicates high certainty about the association between these measures and mental effort. Thus, increases in these constructs were associated with less demand avoidance bias, meaning people high in these constructs exerted relatively more mental effort than individuals with low scores on these scales. Additionally, several self-report measures were associated with a lesser demand avoidance bias but there was high uncertainty in these relationships (i.e., less than 90% but more than 50% of the posterior was negative). The regression using elastic net largely replicated the same pattern of results with parameter values of alpha = 0.55 and lambda = 0.008 (Supplemental Fig. S4). There was no difference in demand avoidance as a function of the presence of a diagnosis as shown in the Supplemental Information.
Coefficient plot where the beta indicates the estimated slope of the line relating severity of the self-report measures and proportion of low demand choices while controlling for age, IQ, and gender. Credible intervals are displayed containing 95% of the posterior probability density around the mean, organized according to ascending coefficient mean. Negative beta intervals are evidence for less demand avoidance (more mental effort) and positive beta intervals are evidence for more demand avoidance (less mental effort).
Demand avoidance and psychiatric factors
Figure 4 shows the mean beta coefficients and credible intervals when regressing the three psychiatric factors onto demand avoidance concurrently, and Table 4 reports the corresponding posterior density of the possible beta values around 0. The compulsive behavior and intrusive thought factor was strongly associated with a reduced demand avoidance bias (0.9% positive) with most of the posterior distribution less than zero. In contrast, the anxious-depression and social withdrawal factors were associated with a greater demand avoidance bias, but there was greater uncertainty in these associations (anxious depression = 76.0% >0, social withdrawal = 82.2% >0).
Coefficient plot where the beta indicates the estimated slope of the line relating severity of the transdiagnostic psychiatric factors and proportion of low demand choices while controlling for age, IQ, and gender. Credible intervals are displayed containing 95% of the posterior probability density around the mean. Negative beta intervals are evidence for less demand avoidance (more mental effort) and positive beta intervals are evidence for more demand avoidance (less mental effort). Factors derived from nine of the self-report measures indicated in Table 1.
We confirmed the factor structure reported by Gillan and colleagues using a CFA with two indices indicating good (RMSEA: 0.059), and acceptable (SRMR: 0.075) fits50. In addition, when the CFA loadings were regressed onto proportion low-demand choices the results were consistent with our results using the Gillan et al.20 loadings, demonstrating that the compulsive behavior and intrusive thought factor was associated with less effort avoidance (Supplemental Information Fig. S5).
Discussion
The law of least mental effort states that, everything else being equal, we seek to minimize cognitive demands9,15. In this study, we investigated the relationship between mental effort and transdiagnostic measures of psychopathology in a large online sample. Former research has largely focused on a single diagnostic category or trait. In contrast, our study measured a broad range of symptoms, traits, and factors that cut across diagnostic boundaries. While increasing scores on lack of perseverance (a facet of impulsiveness), were associated with a greater avoidance of cognitive effort, increasing scores on several constructs were associated with less avoidance of cognitive effort. We found that (1) increasing lack of perseverance was associated with greater avoidance of cognitive effort; (2) increasing positive urgency, distress intolerance, obsessive-compulsive symptoms, and disordered eating were associated with less avoidance of cognitive effort (i.e., all had >90% of the posterior density distributions indicating avoidance decreases); and (3) increasing scores on a transdiagnostic psychiatric factor encompassing compulsive behavior and intrusive thought were also associated with less avoidance of cognitive effort. In addition, increasing scores on several of the self-report measures had more uncertain associations, but indicated less avoidance of cognitive effort (Fig. 3, Table 3).
Prior research on effort-based decision making has largely focused on a single phenomenon (e.g., anhedonia) or diagnostic category (e.g., schizophrenia). We used several transdiagnostic symptoms, traits, and factors to show specific associations between mental effort and various aspects of psychopathology. Lack of perseverance is defined as difficulty completing challenging or boring tasks42. Since this is a self-report measure of effort, this finding provides convergent validity with the DST’s behavioral index of effort avoidance. This is interesting because lack of perseverance has also been associated with several domains of psychopathology including depression, borderline personality traits, disordered eating, alcohol and substance use51. While lack of perseverance has been associated with an increased vulnerability for the development of schizophrenia52, other research indicates no association between lack of perseverance and a diagnosis of schizophrenia53. The current study does not provide evidence as to the relationship between lack of perseverance and DSM diagnoses such as major depressive disorder or schizophrenia. However, increased lack of perseverance may represent a transdiagnostic personality vulnerability within some forms of psychopathology. Further research is needed to establish the association between lack of perseverance and behavioral effort disruption commonly seen in clinical diagnoses.
With the exception of lack of perseverance, several scales were associated with less avoidance of cognitive effort, demonstrating individuals with higher scores on these constructs chose the high-effort option more frequently than those with lower scores. There are several possibilities to contextualize these findings.
First, our findings that increased psychopathology on several scales was associated with increased mental effort somewhat parallel one experiment in Gold and colleagues (2014); one of their experiments showed that patients with a diagnosis of schizophrenia chose the high effort option slightly more frequently. A forced choice condition in a control experiment (e.g., instructions to select the higher, or lower, effort cue) suggests that greater effort expenditure in the patient group may have arisen due to a deficit in adequately estimating the effort costs of the two response options. This is consistent with a cost-benefit account of mental effort5,54,55 and suggests that other forms of psychopathology may be associated with a disruption in the cost-benefit analysis underlying effort expression. However, Gold and colleagues (2014) were unable to demonstrate the main effect of demand avoidance, so it is difficult to determine the nature of the observed deficits in the schizophrenia group. In contrast, we were able to demonstrate the main effect of demand avoidance, so conclusions driven by comparison of the two studies are limited.
Second, Shenhav and colleagues5 propose that effort is comprised of a set of individual characteristics (e.g., information-processing capacity) and cognitive processes (e.g., performance monitoring) that mediate between task demands and task performance. These processes are disrupted in a range of psychiatric illnesses, and therefore another possibility is that the constructs associated with greater effort reflect a deficit in attention, performance monitoring, or other cognitive control abilities56,57. These individuals are not choosing the high effort option more because they prefer it, but because they fail to sustain the representation of the two cues simultaneously during the task. Our data cannot speak to this possibility and future research may benefit from combining effort tasks with other cognitive control paradigms to increase specificity when examining relationships between aspects of cognition and psychopathology.
A third possibility is that, individuals who are elevated on these clinically-related constructs are aware of which option requires lower effort and just prefer the high effort course of action. Evidence for this possibility could manifest as a scenario in which these participants show similar task accuracy as participants low on the clinically-related constructs and just choose to select the high effort option more frequently. Unfortunately, the current data cannot provide strong evidence for this possibility because accuracy and effort are confounded: the high effort option is more difficult, and therefore choosing this option more will decrease accuracy. In an exploratory analysis, we focused on subjects with 90% accuracy or above, and the results remained largely consistent (Supplemental Information). This supports the idea that participants were engaged with the task and deviations of effort were not simply due to random responding. Therefore, three possible mechanisms driving choosing the high effort option more frequently are (1) difficulty estimating the cost of the two response options43, (2) deficits in cognitive processing (e.g., cognitive control) that mediates between task demands and task performance5, and/or (3) a preference for greater mental effort.
Our results also diverge from a large literature indicating that psychopathology is generally associated with reductions of effort (for reviews see Culbreth et al.4; Pessiglione et al.58. However, in addition to the findings of Gold and colleagues indicating greater mental effort, there have been other ambiguities in this research. In a case-control study of major depressive disorder it was found that patients exerted less effort (relative to controls), yet within the patient group higher depressive symptoms were correlated with greater effort59. Using the same task (i.e., EEfRT), McCarthy and colleagues60 found a similar result in patients with a diagnosis of schizophrenia, who exhibited less overall effort, but demonstrated a positive association between effort exertion and negative symptom severity60. Meanwhile, another recent study using the EEfRT task found social anhedonia was associated with greater effort exertion2. These findings suggest that the relationship between the expression of effort and psychopathology may be more nuanced than anticipated by theories4,58 in which psychopathology is associated with effort reductions. Moreover, across studies supporting both reductions and increases in effort, the paradigms have incentivized participants to increase effort. For example, in the EEfRT task1, participants are provided more reward for more presses of the spacebar. As noted above, the DST does not provide greater reward for more effort expenditure. Therefore, the DST may comprise a different set of intervening processes that affect the expression of mental effort, due to the costs associated with action itself (rather than those due to the association between actions and outcomes).
The DST also differs from other effort-based decision-making tasks because participants in the DST are required to learn the effort required by each cue. Moreover, the DST only requires mental effort rather than the physical effort required in the COGED16, EEfRT1, and grip strength task19. It has been suggested that physical effort and mental effort may rely on the same underlying motivation system in the brain61, but behavioral performance may depend upon task-specific systems that differ between mental and physical effort. An open question is whether the effort deviations we observed were localized to this common motivational system, and to what extent the effort disruptions in the DST would generalize to other tasks. The addition of rewards to the DST could shift the observed results; however, it is also possible that we observed a trait-like deficit that would be consistent across other forms of effort-based decision making.
The compulsive behavior and intrusive thought factor demonstrated the same pattern of results as several self-report measures, showing a reduced avoidance of cognitive effort. The results for the anxious-depression and social withdrawal factors demonstrated a more uncertain pattern of results that was associated with greater avoidance of mental effort. These three factors were derived from nine scales that cut across diagnostic categories20. For example, the compulsive behavior and intrusive thought factor contained high loadings from items on the obsessive-compulsive inventory32 and the disordered eating questionnaire31. This suggests that this factor may be associated with cognitive deficits across several domains of psychopathology, perhaps reflecting general difficulties with cognitive control and/or estimating the costs associated with mental effort.
The main limitation of the current investigation was our inability to disentangle the association between psychiatric constructs and various processes underlying the expenditure of mental effort. As noted by others5, this limitation arises because the expenditure of effort is affected by multiple cognitive processes of the individual, and their relationship to psychopathology requires more systematic approaches (e.g., computational modeling) to concurrently examine, and formalize, the processes driving effort expression. Debriefing questions or forced choice trials may have aided in discriminating among the various underlying mechanisms driving effort disruptions such as preference for greater effort, difficulty estimating the effort cost of the two options, and/or cognitive processing deficits. Relatedly, learning the effort costs associated with each cue likely requires working memory processes that are disrupted in schizophrenia62, and we were unable to test for this possibility. In addition, we were unable to formally diagnose our sample with trained clinicians. The MTurk sample may not faithfully represent the general population, and specific disorders may have different relationships with mental effort. However, the relationships we report are based on widely used self-report measures that reflect common constructs in the study of psychopathology.
Another limitation is that the self-report measures are heterogenous in themselves, comprised of many different questions that may measure many different aspects of the proposed construct, further occluding the specificity the construct and its relationship with effort. Using the transdiagnostic factor approach we were able to partially overcome this challenge. However, we were unable to conduct an exploratory factor analysis on all the measure items concurrently due to the large number of items (385) and low subject-to-variable ratio (~2:1). Future research with a larger sample could identify additional factors and provide a more compact analysis by reducing the self-report measures into fewer dimensions. In addition, network63 and computational approaches to the structure of psychopathology64 will be needed to further parse dissociable aspects of psychiatric illness and look at relationships with cognition.
The current study demonstrated that various aspects of psychopathology are associated with deviations from the law of least mental effort. Our findings demonstrate the specificity that can be achieved with transdiagnostic approaches to the study of cognition. Choosing the low effort option more frequently is associated with a personality trait characterized by lack of perseverance. We report that choosing the high effort option more frequently is associated with elevations on several psychiatrically-relevant constructs, including positive urgency, distress intolerance, obsessive-compulsive symptoms, disordered eating, and a transdiagnostic psychiatric factor encompassing compulsive behavior and intrusive thought. This suggests that some psychopathological disruptions may be associated with increased effort expression, rather than reduced effort expression as suggested by common theoretical models of effort-based decision-making4,58. The current study has significant clinical implications, showing that symptoms, traits, and transdiagnostic dimensions that cut across diagnostic boundaries are associated with deviations in the expression of mental effort. Furthermore, these transdiagnostic abnormalities in effort exertion may correspond to challenges exerting the appropriate level of mental effort for the tasks of daily life.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon request consistent with the IRB data sharing protocol.
References
Treadway, M. T., Buckholtz, J. W., Schwartzman, A. N., Lambert, W. E. & Zald, D. H. Worth the ‘EEfRT’? The effort expenditure for rewards task as an objective measure of motivation and anhedonia. PLoS One 4, 1–9 (2009).
McCarthy, J. M., Treadway, M. T. & Blanchard, J. J. Motivation and effort in individuals with social anhedonia. Schizophr. Res. 165, 70–75 (2015).
Le Heron, C., Apps, M. A. J. & Husain, M. The anatomy of apathy: A neurocognitive framework for amotivated behaviour. Neuropsychologia 0–1, https://doi.org/10.1016/j.neuropsychologia.2017.07.003 (2017).
Culbreth, A. J., Moran, E. K. & Barch, D. M. Effort-cost decision-making in psychosis and depression: could a similar behavioral deficit arise from disparate psychological and neural mechanisms? Psychol. Med. 48, 889–904 (2018).
Shenhav, A. et al. Toward a Rational and Mechanistic Account of Mental Effort. Annu. Rev. Neurosci. 40, 99–124 (2017).
Clark, L. A., Cuthbert, B., Lewis-Fernández, R., Narrow, W. E. & Reed, G. M. Three Approaches to Understanding and Classifying Mental Disorder: ICD-11, DSM-5, and the National Institute of Mental Health’s Research Domain Criteria (RDoC). Psychol. Sci. Public Interes. 18, 72–145 (2017).
Insel, T. et al. Research domain criteria (RDoC): Toward a new classification framework for research on mental disorders. Am. J. Psychiatry 167, 748–751 (2010).
Cuthbert, B. N. & Insel, T. R. Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Med. 11, 126 (2013).
Kool, W., McGuire, J. T., Rosen, Z. B. & Botvinick, M. M. Decision Making and the Avoidance of Cognitive Demand. J. Exp. Psychol. Gen. 139, 665–682 (2010).
Hull, C. L. Principles of Behavior. (Appleton-Century-Crofts 1943).
Tversky, A. & Kahneman, D. Judgment under Uncertainty: Heuristics and Biases. Science (80-.). 185, 1124–1131 (1974).
Monsell, S. Task switching. Trends Cogn. Sci. 7, 134–140 (2003).
McGuire, J. T. & Botvinick, M. M. Prefrontal cortex, cognitive control, and the registration of decision costs. Proc. Natl. Acad. Sci. 107, 7922–7926 (2010).
Kool, W., Mcguire, J. T., Wang, G. J. & Botvinick, M. M. Neural and Behavioral Evidence for an Intrinsic Cost of Self-Control. PLoS One 8 (2013).
Balle, M. La loi du moindre effort mental: [The law of least mental effort]. Sci. Hum. 36–39 (2002).
Westbrook, A., Kester, D. & Braver, T. S. What Is the Subjective Cost of Cognitive Effort? Load, Trait, and Aging Effects Revealed by Economic Preference. PLoS One 8 (2013).
Wolf, D. H. et al. Amotivation in schizophrenia: Integrated assessment with behavioral, clinical, and imaging measures. Schizophr. Bull. 40, 1328–1337 (2014).
Gold, J. M. et al. Negative symptoms of schizophrenia are associated with abnormal effort-cost computations. Biol. Psychiatry 74, 130–136 (2013).
Hartmann, M. N., Hager, O. M., Tobler, P. N. & Kaiser, S. Parabolic discounting of monetary rewards by physical effort. Behav. Processes 100, 192–196 (2013).
Gillan, C. M., Kosinski, M., Whelan, R., Phelps, E. A. & Daw, N. D. Characterizing a psychiatric symptom dimension related to deficits in goal-directed control. eLife 5 (2016).
Patzelt, E. H., Kool, W. J., Millner, A. J. & Gershman, S. J. Incentives Boost Model-based Control Across a Range of Severity on Several Psychiatric Constructs. Biol. Psychiatry, https://doi.org/10.1016/j.biopsych.2018.06.018 (2018).
Salamone, J. D. et al. The pharmacology of effort-related choice behavior: Dopamine, depression, and individual differences. Behav. Processes 127, 3–17 (2016).
Holroyd, C. B. & Umemoto, A. The research domain criteria framework: The case for anterior cingulate cortex. Neurosci. Biobehav. Rev. 71, 418–443 (2016).
Raven, J. The Raven’s Progressive Matrices: Change and Stability over Culture and Time. Cogn. Psychol. 41, 1–48 (2000).
Kool, W., Gershman, S. J. & Cushman, F. A. Cost-benefit arbitration between multiple reinforcement learning systems. Psychol. Sci. 28, 1321–1333 (2017).
Marin, R., Biedrzycki, R. & Firinciogullari, S. Reliability and validity of the apathy evaluation scale. Psychiatry Res. 38, 143–162 (1991).
Spielberger, C. D., Gorsuch, R. L., Lushene, P. R., Vagg, P. R. & Jacobs, A. G. Manual for the State-Trait Anxiety Inventory. (Consulting Psychologists Press 1983).
Saunders, J. B., Aasland, O. G., Babor, T. F., De La Fuente, J. R. & Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption. II. Addiction 88, 791–804 (1993).
Patton, J. H., Stanford, M. S. & Barratt, E. S. Factor structure of the Barratt impulsiveness scale. J. Clin. Psychol. 51, 768–74 (1995).
Zung, W. & Durham, N. A Self-Rating Depression Scale. Arch. Gen. Psychiatry 12, 63–70 (1965).
Garner, D., Olmsted, M. P., Bohr, Y. & Garfinkel, P. The eating attitudes test: psychometric features and clinical correlates. Psychol. Med. 12, 871–878 (1982).
Foa, E. B. et al. The obsessive-compulsive inventory: Development and validation of a short version. Psychol. Assess. 14, 485–496 (2002).
Mason, O., Linney, Y. & Claridge, G. Short scales for measuring schizotypy. Schizophr. Res. 78, 293–296 (2005).
Liebowitz, M. R. Social phobia. Mod. Probl. Pharmacopsychiatry 22, 141–173 (1987).
Carleton, R. N., Norton, M. A. P. J. & Asmundson, J. G. Fearing the unknown: A short version of the Intolerance of Uncertainty Scale. J. Anxiety Disord. 21, 105–117 (2007).
Taylor, S. et al. Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychol. Assess. 19, 176–188 (2007).
Nolen-Hoeksema, S. & Morrow, J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta earthquake. J. Pers. Soc. Psychol. 61, 115–121 (1991).
Gratz, K. L. & Roemer, L. Multidimensional assessment of emotion regulation and dysregulation. J. Psychopathol. Behav. Assess. 26, 41–54 (2004).
Simons, J. S. & Gaher, R. M. The distress tolerance scale: Development and validation of a self-report measure. Motiv. Emot. 29, 83–102 (2005).
Lynam, D. R., Smith, G. T., Cyders, M. A., Fischer, S. & Whiteside, S. P. The UPPS-P questionnaire measure of five dispositions to rash action (unpublished technical report) (2007).
Cyders, M. A. et al. Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychol. Assess. 19, 107–118 (2007).
Whiteside, S. P. & Lynam, D. R. The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Pers. Individ. Dif. 30, 669–689 (2001).
Gold, J. M. et al. Cognitive effort avoidance and detection in people with schizophrenia. Cogn. Affect. Behav. Neurosci. 15, 145–154 (2014).
Gelman, A. et al. Bayesian data analysis. (CRC Press 2013).
Baldwin, S. A. & Larson, M. J. An introduction to using Bayesian linear regression with clinical data. Behav. Res. Ther. 98, 58–75 (2016).
Burkner, P. C. brms: An R Package for Bayesian Multilevel Models using Stan. J. Stat. Softw. 80, 1–28 (2013).
Kuhn, M. Building Predictive Models in R Using the caret Package. J. Stat. Softw. 28, 1–26 (2008).
Friedman, J., Hastie, T. & Tibshirani, R. Regularization Paths for Generalized Linear Models via Coordinate Descent. J. Stat. Softw. 33, 1–22 (2010).
Rosseel, Y. Lavaan: an R package for structural equation modeling and more. J. Stat. Softw. 48, 1–36 (2012).
Cangur, S. & Ercan, I. Comparison of Model Fit Indices Used in Structural Equation Modeling Under Multivariate Normality. J. Mod. Appl. Stat. Methods 14, 152–167 (2015).
Berg, J. M., Latzman, R. D., Bliwise, N. G. & Lilienfeld, S. O. Parsing the heterogeneity of impulsivity: A meta-analytic review of the behavioral implications of the UPPS for psychopathology. Psychol. Assess. 27, 1129–1146 (2015).
Ho, B. C., Barry, A. B. & Koeppel, J. A. Impulsivity in unaffected adolescent biological relatives of schizophrenia patients. J. Psychiatr. Res. 97, 47–53 (2018).
Hoptman, M. J., Antonius, D., Mauro, C. J., Parker, E. M. & Javitt, D. C. Cortical thinning, functional connectivity, and mood-related impulsivity in schizophrenia: Relationship to Aggressive attitudes and behavior. Am. J. Psychiatry 171, 939–948 (2014).
Kurzban, R., Duckworth, A., Kable, J. W. & Myers, J. An opportunity cost model of subjective effort and task performance. Behav. Brain Sci. 36, 661–679 (2013).
Kool, W. & Botvinick, M. Mental labour. Nat. Hum. Behav. https://doi.org/10.1038/s41562-018-0401-9 (2018).
Macdonald, A. W., Cohen, J. D., Stenger, V. A. & Carter, C. S. Dissociating the Role of the Dorsolateral Prefrontal and Anterior Cingulate Cortex in Cognitive Control. Science (80-.). 288, 1835–1838 (2000).
Botvinick, M. M., Braver, T. S., Barch, D. M., Carter, C. S. & Cohen, J. D. Conflict monitoring and cognitive control. Psychological Review 108, 624–652 (2001).
Pessiglione, M., Vinckier, F., Bouret, S., Daunizeau, J. & Le Bouc, R. Why not try harder? Computational approach to motivation deficits in neuro-psychiatric diseases. Brain. https://doi.org/10.1093/brain/awx278 (2017).
Treadway, M. T., Bossaller, N. A., Shelton, R. C. & Zald, D. H. Effort-based decision-making in major depressive disorder: A translational model of motivational anhedonia. J. Abnorm. Psychol. 121, 553–558 (2012).
McCarthy, J. M., Treadway, M. T., Bennett, M. E. & Blanchard, J. J. Inefficient effort allocation and negative symptoms in individuals with schizophrenia. Schizophr. Res. 170, 278–284 (2016).
Schmidt, L., Lebreton, M., Cléry-Melin, M. L., Daunizeau, J. & Pessiglione, M. Neural mechanisms underlying motivation of mental versus physical effort. PLoS Biol. 10, 1001266 (2012).
Collins, A. G. E., Brown, J. K., Gold, J. M., Waltz, J. A. & Frank, M. J. Working Memory Contributions to Reinforcement Learning Impairments in Schizophrenia. J. Neurosci. 34, 13747–13756 (2014).
Borsboom, D. A network theory of mental disorders. World Psychiatry 16, 5–13 (2016).
Patzelt, E. H., Hartley, C. A. & Gershman, S. J. Computational phenotyping: using models to understand individual differences in personality, development, and mental illness. Personal. Neurosci (2018).
Acknowledgements
This project was partially supported by a training grant from the NIH Blueprint for Neuroscience Research (T90DA022759/R90DA023427), and NIH grant CRCNS R01-1207833. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. We would like to thank Michal Kosinksi for use of the IQ test, Drs. Bruce Rosen and Maria Mody for their work with the AMNTP, and the members of the Computational Cognitive Neuroscience Laboratory for their support and feedback.
Author information
Authors and Affiliations
Contributions
E.H.P., W.K., and S.J.G. designed the study. E.H.P. collected and analyzed the data. E.H.P. wrote the initial version of the manuscript, and W.K., A.J.M, and S.J.G. reviewed and provided input for the final version.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Patzelt, E.H., Kool, W., Millner, A.J. et al. The transdiagnostic structure of mental effort avoidance. Sci Rep 9, 1689 (2019). https://doi.org/10.1038/s41598-018-37802-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-37802-1
This article is cited by
-
Investigating links between creativity anxiety, creative performance, and state-level anxiety and effort during creative thinking
Scientific Reports (2023)
-
Learned industriousness as a translational mechanism in anorexia nervosa
Nature Reviews Psychology (2022)
-
Psychiatrically relevant signatures of domain-general decision-making and metacognition in the general population
npj Mental Health Research (2022)
-
Preferences for seeking effort or reward information bias the willingness to work
Scientific Reports (2022)
-
Value-free random exploration is linked to impulsivity
Nature Communications (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.