Abstract
Patients with papillary thyroid carcinoma (PTC) would benefit from risk stratification tools that can aid in planning personalized treatment and follow-up. The aim of this study was to develop a conventional ultrasound (US)-based radiomics signature to estimate disease-free survival (DFS) in patients with conventional PTC. Imaging features were extracted from the pretreatment US images of 768 patients with conventional PTC who were treated between January 2004 and February 2006. The median follow-up period was 117.3 months, with 85 (11.1%) events. A radiomics signature (Rad-score) was generated by using the least absolute shrinkage and selection operator (LASSO) method in Cox regression. The Rad-score was significantly associated with DFS (hazard ratio [HR], 3.087; P < 0.001), independent of clinicopathologic risk factors. A radiomics model which incorporated the Rad-score demonstrated better performance in the estimation of DFS (C-index: 0.777; 95% confidence interval [CI]: 0.735, 0.829) than the clinicopathologic model (C-index: 0.721; 95% CI: 0.675, 0.780). In conclusion, radiomics features from pretreatment US may be potential imaging biomarkers for risk stratification in patients with conventional PTC.
Similar content being viewed by others
Introduction
Papillary thyroid carcinoma (PTC) is the most common histologic type of thyroid cancer, and accounts for the majority of increased incidence in thyroid cancer during the last several decades1,2. Because of its treatability and relatively favorable survival rate, the perception of thyroid cancer as a “good cancer” has spread among patients and healthcare providers3,4. Along with recent guidelines recommending active surveillance rather than treatment in selected patients, some researchers have also suggested expanding this management approach to a larger size range of PTCs5. However, a small subset of PTCs shows aggressive clinical behavior, with approximately 9.1–13.3% of patients experiencing recurrence and 1.4–5.2% dying from thyroid cancer6,7. Incidence-based mortality for PTC has also increased — increasing 1.1% per year overall and 2.9% per year for distant stage PTC in the United States2. Therefore, patients with PTC would largely benefit from preoperative risk stratification tools that can aid in planning appropriate treatment and follow-up.
The field of medical image analysis has grown exponentially in the past decade, fueled by the routine use of digital medical images and developments in methods for quantitative image analysis. Radiomics, a promising field in cancer imaging research, is based on the concept that medical images contain crucial information reflecting underlying pathophysiology, which can be used to support evidence-based clinical decisions8. Biomarkers based on quantitative radiomics features have been associated with clinical prognosis and genomic phenotypes across a wide range of cancer types9,10,11,12,13. Recently, this approach has also been applied to the analysis of thyroid nodules. Previous studies have reported that sonographic histogram and texture analyses are useful for differentiating benign and malignant thyroid nodules14,15,16,17,18. However, to our knowledge, there are no published studies that have investigated whether a radiomics approach can be used to estimate the prognosis of PTC.
Therefore, the aim of this study was to develop a radiomics signature based on thyroid ultrasound (US) images to estimate disease-free survival (DFS) in patients with conventional PTC, and to assess its incremental value to clinical-pathologic risk factors.
Results
Clinical Characteristics and Patient Outcomes
Among the 768 patients, 747 (97.3%) underwent total or near-total thyroidectomy, 13 (1.7%) underwent hemithyroidectomy, and 8 (1.0%) underwent hemithyroidectomy with contralateral subtotal thyroidectomy. Table 1 shows the clinicopathologic features of the 768 patients. The median follow-up period was 117.3 months (range, 36.3–154.23 months). At the last follow-up, 85 patients (11.1%) experienced recurrent or persistent disease, with 56 (7.3%) experiencing recurrence and 29 (3.8%) experiencing persistent disease.
Construction of the Radiomics Signature
Of the 730 texture features, the top 40 features were selected in the LASSO Cox regression model based on repeated 10-fold cross-validation. These features were used to build the radiomics signature. The Rad-score calculation formula is presented in the Supplementary Information, where the selected features are presented.
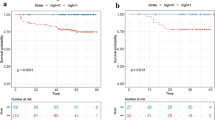
Association of the Radiomics Signature with Disease-free Survival
At univariate analysis, the radiomics signature was associated with disease-free survival (HR = 4.531, 95% CI: 2.909, 7.056 [P < 0.001]) (Table 2). Among clinicopathologic variables, a larger pathological tumor size (HR = 1.042, 95% CI: 1.022, 1.063 [P < 0.001]), presence of cervical lymph node metastasis (HR = 4.919, 95% CI: 2.611, 9.267 [P < 0.001]), distant metastasis (HR = 8.132, 95% CI: 3.286, 20.120 [P < 0.001]), gross extrathyroidal extension (HR = 2.253, 95% CI: 1.040, 4.884 [P = 0.040]), and a higher dose of radioactive ablation (RAI) (HR = 1.010, 95% CI: 1.006, 1.013 [P < 0.001]) was associated with worse disease-free survival.
At multivariate analysis, the radiomics signature was independently associated with disease-free survival (HR = 3.087, 95% CI: 1.931, 4.935 [P < 0.001]). Among clinicopathologic variables, the presence of cervical lymph node metastasis (HR = 3.585, 95% CI: 1.849, 6.952 [P < 0.001]), distant metastasis (HR = 3.449, 95% CI: 1.329, 8.950 [P = 0.011]), and a higher dose of RAI ablation (HR = 1.005, 95% CI: 1.001, 1.009 [P = 0.009]) was associated with worse disease-free survival.
Assessment of the Incremental Value of the Radiomics Signature in DFS prediction
The clinicopathologic model for predicting disease-free survival yielded a C-index of 0.721 (95% CI: 0.675, 0.780). We created a radiomics model that integrated the radiomics signature with all clinicopathologic data, and found that adding the radiomics signature to the clinicopathologic model yielded an improvement of 0.056 (95% CI: 0.023, 0.096) in the C-index, showing improved classification accuracy for disease-free survival (Table 3).
Discussion
In the current study, we evaluated the ability of multi-feature-based radiomics to help estimate disease-free survival in patients with conventional PTC. To our knowledge, this is the first study to apply radiomics in the estimation of prognosis in patients with PTC. The radiomics signature was identified as an independent prognostic factor, and added incremental value to other clinico-pathologic risk factors when estimating individualized disease-free survival. Our study demonstrates the potential of applying a radiomics approach to conventional PTC.
As PTC is generally associated with an excellent long-term mortality, setting disease-free survival from recurrence or persistent disease as the focus endpoint for risk stratification, rather than mortality, would benefit more patients by potentially aiding in individualized treatment and management. In efforts to achieve such risk-stratification, previous researchers have focused on identifying clinico-pathologic risk factors associated with recurrent or persistent disease19,20,21,22. Yet, these studies generally included various histologic subtypes and used conventional risk factors which are only obtainable after treatment is completed. In our study, we found that the radiomics signature, which is obtained from preoperative images, was independently associated with disease-free survival (HR = 3.087) and could provide more prognostic information prior to the initiation of treatment.
Although radiomics has shown potential in other cancers, research in thyroid cancer has been relatively limited. Previous studies on radiomics in thyroid disease have mostly focused on differentiating benign and malignant nodules or detecting lymph node metastasis by using relatively simple histogram and texture analysis techniques14,15,16,18,23. In our study, for the construction of the radiomics signature, 730 candidate radomics features were reduced to 40 potential predictors through the LASSO cox regression model, which is known as a useful method for feature selection in high-dimensional data13,24. Whereas previous staging systems and nomograms, including the American Joint Committee on Cancer (AJC) tumor node metastasis (TNM) staging system, have shown excellent discriminatory ability for mortality prediction with AUC values of 0.89–0.98, the AUC values of nomograms for recurrence prediction in thyroid cancer have been slightly lower, ranging from 0.72–0.7619,25,26,27,28,29. In our study, the radiomics signature that combined multiple individual imaging features significantly improved the predictive accuracy of the clinicopathologic model, yielding a C-index of 0.777 (95% CI: 0.735, 0.829). Our study suggests that combining radomics data with other clinicopathologic risk factors may increase the power of decision support models, and aid in achieving personalized estimation of disease-free survival in PTC.
There are some limitations to this study, such as the retrospective nature of its data collection and the relatively small sample size. Another limitation is the lack of external validation and a separate validation data set. Therefore, further studies are needed to overcome these limitations and to validate our results for better generalization. Although the prospective cohort study design would be the preferred study design of such research, the long wait required to analyze survival outcome in PTC, due to its generally excellent prognosis, makes such research daunting to perform. In addition, the small number of events makes it difficult to yield reliable results with smaller data sets. Although we were unable to perform such an independent validation, to our knowledge, this is the first study to apply multi-feature-based radiomics in the estimation of prognosis in patients with PTC. Our results indicate that radiomics has the potential to be a tool for risk stratification, but further validation is needed.
In conclusion, our preliminary study shows that the identified radiomics signature has the potential to be used as a biomarker for risk stratification in patients with conventional PTC. The radiomics model, which incorporated the radiomics signature with clinicopathologic data, showed a significant improvement in discrimination performance for evaluating disease-free survival. Although promising, these are preliminary results and further validation is required on a larger and independent data set before clinical application. After validation, the radiomics signature may serve as a potential tool to guide individualized management for patients with PTC, of whom the majority will have excellent prognosis.
Methods
Patients
The institutional review board of Severance hospital approved this retrospective study and the requirement for informed consent was waived. Our institutional database was reviewed to identify patients with histologically confirmed conventional papillary thyroid carcinoma who underwent preoperative US and thyroid surgery from January 2004 to February 2006. In total, 768 patients were identified (648 women and 120 men; median age, 45 years [range, 17–80 years]; tumor size, 16 mm [range, 2–65 mm]) and comprised our study population. Among the study patients, 299 patients were included in a prior study which compared the diagnostic accuracy of preoperative staging using US imaging and CT30, and 469 patients were included in a prior study which investigated whether conventional US features were associated with tumor recurrence in PTC31.
Surgery and Follow-up
Total or near-total thyroidectomy was performed in patients who had multiple tumors, extrathyroidal invasion or lymph node metastasis (LNM) on either preoperative or intraoperative findings. Central compartment neck dissection including the paratracheal, pretracheal, and prelaryngeal lymph nodes is routinely performed at our institution. Bilateral central compartment neck dissection was performed in patients who underwent total or near-total thyroidectomy and ipsilateral central compartment neck dissection was performed in patients who underwent hemithyroidectomy. Lateral compartment neck dissection was performed in selected patients with lateral LNM diagnosed by preoperative US-guided fine-needle aspiration. If suspicious LNs were found during surgery, intraoperative frozen biopsy was performed. In patients confirmed to have lateral LNM, lateral neck compartments including levels 2, 3, 4 and anterior level 5 were dissected.
For postoperative follow-up, clinical examination, neck US, chest radiographs, and measurements of serum thyroid-stimulating hormone (TSH), free T4, thyroglobulin (Tg), and anti-Tg antibody were recommended annually. For patients with suspected recurrence chest computed tomography (CT), magnetic resonance imaging (MRI), whole body bone scan or fluorodeoxyglucose positron emission tomography (PET) was performed at the discretion of the physician.
Clinicopathologic data including age, gender, pathological tumor size, cervical lymph node metastasis (LNM), gross extrathyroidal extension, surgery method (total or near-total thyroidectomy, hemithyroidectomy, and hemithyroidectomy with contralateral subtotal thyroidectomy), and radioiodine ablation dose were collected from medical records. Medical records and imaging studies during postoperative surveillance were reviewed for patient outcome.
No evidence of disease was defined as no biochemical (suppressed thyroglobulin (Tg) < 1 ng/mL, stimulated Tg < 2 ng/mL, with negative anti-Tg antibodies) or structural recurrences (no evidence of disease on US, cross-sectional and/or nuclear imaging) during follow-up32. Distant metastasis was defined as the development of thyroid cancer foci at distant organs located in areas other than the neck, which was either confirmed with biopsy or clinically suspected based on various imaging studies. Recurrence/persistence of disease was defined by biochemical, structural or functional evidence of disease that was detected with/without a period of any evidence of disease since initial surgery32. Disease-free survival was defined as the time of interval (in months) between initial surgery and occurrence of recurrence/persistence or the date of last clinical follow-up.
US Examinations
All patients underwent preoperative US including both thyroid glands and cervical regions, performed by using a 7–12-MHz (HDI 3000 or 5000; Philips Medical Systems, Bothell,Wash), 5–13-MHz (SONOLINE Antares; Siemens Medical Solutions, Erlangen,Germany/Acuson Sequoia 512; Acuson, Mountain View, CA), or a 5–12-MHz linear array transducer (iU22; Philips Medical Systems, Bothell,Wash).
Radiomics Feature Analysis
For image feature extraction, a representative US image was selected for each tumor from images that were previously captured by the radiologist at the time of the US examination, and which were retrieved from the picture archiving and communication system. Manual segmentation of the thyroid tumors was performed by a radiologist (V. Y. P) who had 7 years of experience in thyroid US imaging. A region of interest (ROI) was delineated around the boundary of the index tumor on a representative US image, which was validated by a senior radiologist (K.J.Y) who had 16 years of experience in thyroid US imaging.
The radiomics feature extraction methodology is described in Appendix E1 (online). Texture feature extraction was performed by in-house texture analysis algorithms implemented in MATLAB 2016b (The MathWorks, Inc., Natick, Massachusetts, United States). After saving the ROI-segmented US images as JPG images, the images were then converted into grayscale intensity images by eliminating the hue and saturation information while retaining luminance. A total of 730 candidate radomics features, using GLCM and GLRLM texture matrices, single-level discrete 2D wavelet transform and so forth, were generated from a single US image (Fig. 1). Each image was normalized for direct comparison between patients.
Example of the radiomics feature extraction. (a) Each tumor was first manually segmented on a representative US image (left) and subsequently, the position information of the ROI (middle) was collected and applied to the US image without marking the ROI itself, allowing the ROI to be extracted from the original US image (right). (b) Intensity histogram of the ROI image is shown. First and second order statistics values were calculated for each image. (c) For further feature extraction, the wavelet transform was used. For clearer presentation, the wavelet coefficients were scaled into a range from 0 to 255. From left to right: wavelet decompositions of the original image using LL, LH, HL, and HH, where L and H are low- and high-pass filters in the x- and y-directions, respectively.
Statistical Analysis
To select radiomics features, we used the least absolute shrinkage and selection operator (LASSO) method in Cox regression to select the most useful prognostic imaging features for disease-free survival. The LASSO method is a penalized technique for variable selection that is suitable for the regression of high-dimensional data33.
In the LASSO Cox regression analysis, 10-fold cross-validation was used to avoid overfitting and to estimate errors of partial likelihood deviance, which is a goodness-of-fit statistic in Cox regression. Additionally, the whole process of partitioning and estimating through cross-validation was repeated 100 times. In each validation step, features were selected by using minimum criteria—i.e., optimal tuning parameter of the LASSO that minimized the partial likelihood deviance was selected and we took the average as the final coefficients for each feature34. A larger average coefficient indicates a more relevant feature. Repeated cross-validation can reduce variation caused by the randomness of partitioning the sample into 10-folds as well as estimates of prediction error.
A radiomics score (Rad score) was calculated for each patient as a linear combination of selected features that were weighted by their respective coefficients. The number of features chosen to calculate the radiomics score was determined by the mean number of features selected through 100 repeated cross-validation.
To estimate the association between disease-free survival and radiomics features with clinicopathologic factors, univariable and multivariable Cox proportional hazard regressions were performed. Hazard ratios with 95% confidence interval (CI) for each variable were estimated. To evaluate the incremental prognostic value of the radiomics score when added to clinicopathologic factors, Harrell’s C-index was calculated and compared using the bootstrap method with 1,000 resampling. The significance of the incremental values of the radiomics score was determined using 95% CI for the difference in C-index.
The statistical analysis was performed using R software, version 3.3.3 (http://www.R-project.org). The LASSO method and Cox regression was performed using the “glmnet” and “survival” R packages, respectively. Bootstrapping was implemented using the “boot” R package. P values < 0.05 indicated statistical significance.
References
Ahn, H. S. et al. Thyroid Cancer Screening in South Korea Increases Detection of Papillary Cancers with No Impact on Other Subtypes or Thyroid Cancer Mortality. Thyroid 26, 1535–1540, https://doi.org/10.1089/thy.2016.0075 (2016).
Lim, H., Devesa, S. S., Sosa, J. A., Check, D. & Kitahara, C. M. Trends in Thyroid Cancer Incidence and Mortality in the United States, 1974-2013. Jama 317, 1338–1348, https://doi.org/10.1001/jama.2017.2719 (2017).
Randle, R. W. et al. Papillary Thyroid Cancer: The Good and Bad of the “Good Cancer”. Thyroid, https://doi.org/10.1089/thy.2016.0632 (2017).
Vaccarella, S. et al. Worldwide Thyroid-Cancer Epidemic? The Increasing Impact of Overdiagnosis. N Engl J Med 375, 614–617, https://doi.org/10.1056/NEJMp1604412 (2016).
Griffin, A., Brito, J. P., Bahl, M. & Hoang, J. K. Applying Criteria of Active Surveillance to Low-Risk Papillary Thyroid Cancer Over a Decade: How Many Surgeries and Complications Can Be Avoided? Thyroid 27, 518–523, https://doi.org/10.1089/thy.2016.0568 (2017).
Cho, B. Y. et al. Changes in the clinicopathological characteristics and outcomes of thyroid cancer in Korea over the past four decades. Thyroid 23, 797–804, https://doi.org/10.1089/thy.2012.0329 (2013).
Londero, S. C. et al. Papillary thyroid carcinoma in Denmark, 1996-2008: outcome and evaluation of established prognostic scoring systems in a prospective national cohort. Thyroid 25, 78–84, https://doi.org/10.1089/thy.2014.0294 (2015).
Gillies, R. J., Kinahan, P. E. & Hricak, H. Radiomics: Images Are More than Pictures, They Are Data. Radiology, 151169, https://doi.org/10.1148/radiol.2015151169 (2015).
Aerts, H. J. et al. Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun 5, 4006, https://doi.org/10.1038/ncomms5006 (2014).
Grove, O. et al. Quantitative computed tomographic descriptors associate tumor shape complexity and intratumor heterogeneity with prognosis in lung adenocarcinoma. PLoS One 10, e0118261, https://doi.org/10.1371/journal.pone.0118261 (2015).
Huang, Y. Q. et al. Development and Validation of a Radiomics Nomogram for Preoperative Prediction of Lymph Node Metastasis in Colorectal Cancer. J Clin Oncol 34, 2157–2164, https://doi.org/10.1200/jco.2015.65.9128 (2016).
Li, H. et al. MR Imaging Radiomics Signatures for Predicting the Risk of Breast Cancer Recurrence as Given by Research Versions of MammaPrint, Oncotype DX, and PAM50 Gene Assays. Radiology, 152110, https://doi.org/10.1148/radiol.2016152110 (2016).
Zhang, B. et al. Radiomics Features of Multiparametric MRI as Novel Prognostic Factors in Advanced Nasopharyngeal Carcinoma. Clin Cancer Res, https://doi.org/10.1158/1078-0432.ccr-16-2910 (2017).
Chen, S. J. et al. Classification of the thyroid nodules based on characteristic sonographic textural feature and correlated histopathology using hierarchical support vector machines. Ultrasound Med Biol 36, 2018–2026, https://doi.org/10.1016/j.ultrasmedbio.2010.08.019 (2010).
Grani, G. et al. Grey-Scale Analysis Improves the Ultrasonographic Evaluation of Thyroid Nodules. Medicine (Baltimore) 94, e1129, https://doi.org/10.1097/md.0000000000001129 (2015).
Song, G., Xue, F. & Zhang, C. A Model Using Texture Features to Differentiate the Nature of Thyroid Nodules on Sonography. J Ultrasound Med 34, 1753–1760, https://doi.org/10.7863/ultra.15.14.10045 (2015).
Bhatia, K. S., Lam, A. C., Pang, S. W., Wang, D. & Ahuja, A. T. Feasibility Study of Texture Analysis Using Ultrasound Shear Wave Elastography to Predict Malignancy in Thyroid Nodules. Ultrasound Med Biol 42, 1671–1680, https://doi.org/10.1016/j.ultrasmedbio.2016.01.013 (2016).
Nam, S. J. et al. Quantitative Evaluation for Differentiating Malignant and Benign Thyroid Nodules Using Histogram Analysis of Grayscale Sonograms. J Ultrasound Med 35, 775–782, https://doi.org/10.7863/ultra.15.05055 (2016).
Ge, M. H. et al. Nomograms predicting disease-specific regional recurrence and distant recurrence of papillary thyroid carcinoma following partial or total thyroidectomy. Medicine (Baltimore) 96, e7575, https://doi.org/10.1097/md.0000000000007575 (2017).
Piccardo, A. et al. Focus on high-risk DTC patients: high postoperative serum thyroglobulin level is a strong predictor of disease persistence and is associated to progression-free survival and overall survival. Clin Nucl Med 38, 18–24, https://doi.org/10.1097/RLU.0b013e318266d4d8 (2013).
Radowsky, J. S., Howard, R. S., Burch, H. B. & Stojadinovic, A. Impact of degree of extrathyroidal extension of disease on papillary thyroid cancer outcome. Thyroid 24, 241–244, https://doi.org/10.1089/thy.2012.0567 (2014).
Wang, F. et al. The Prognostic Value of Tumor Multifocality in Clinical Outcomes of Papillary Thyroid Cancer. J Clin Endocrinol Metab 102, 3241–3250, https://doi.org/10.1210/jc.2017-00277 (2017).
Kim, S. Y. et al. Ultrasound texture analysis: Association with lymph node metastasis of papillary thyroid microcarcinoma. PLoS One 12, e0176103, https://doi.org/10.1371/journal.pone.0176103 (2017).
Huang, Y. et al. Radiomics Signature: A Potential Biomarker for the Prediction of Disease-Free Survival in Early-Stage (I or II) Non-Small Cell Lung Cancer. Radiology, 152234, https://doi.org/10.1148/radiol.2016152234 (2016).
Nixon, I. J. et al. Defining a Valid Age Cutoff in Staging of Well-Differentiated Thyroid Cancer. Ann Surg Oncol 23, 410–415, https://doi.org/10.1245/s10434-015-4762-2 (2016).
Yang, L., Shen, W. & Sakamoto, N. Population-based study evaluating and predicting the probability of death resulting from thyroid cancer and other causes among patients with thyroid cancer. J Clin Oncol 31, 468–474, https://doi.org/10.1200/jco.2012.42.4457 (2013).
Lang, B. H., Wong, C. K., Yu, H. W. & Lee, K. E. Postoperative nomogram for predicting disease-specific death and recurrence in papillary thyroid carcinoma. Head Neck 38(Suppl 1), E1256–1263, https://doi.org/10.1002/hed.24201 (2016).
Pathak, K. A., Mazurat, A., Lambert, P., Klonisch, T. & Nason, R. W. Prognostic nomograms to predict oncological outcome of thyroid cancers. J Clin Endocrinol Metab 98, 4768–4775, https://doi.org/10.1210/jc.2013-2318 (2013).
Lang, B. H. & Wong, C. K. Validation and Comparison of Nomograms in Predicting Disease-Specific Survival for Papillary Thyroid Carcinoma. World J Surg 39, 1951–1958, https://doi.org/10.1007/s00268-015-3044-2 (2015).
Choi, J. S. et al. Preoperative staging of papillary thyroid carcinoma: comparison of ultrasound imaging and CT. AJR Am J Roentgenol 193, 871–878, https://doi.org/10.2214/ajr.09.2386 (2009).
Kim, S. Y., Kwak, J. Y., Kim, E. K., Yoon, J. H. & Moon, H. J. Association of Preoperative US Features and Recurrence in Patients with Classic Papillary Thyroid Carcinoma. Radiology 277, 574–583, https://doi.org/10.1148/radiol.2015142470 (2015).
Tuttle, R. M. et al. Estimating risk of recurrence in differentiated thyroid cancer after total thyroidectomy and radioactive iodine remnant ablation: using response to therapy variables to modify the initial risk estimates predicted by the new American Thyroid Association staging system. Thyroid 20, 1341–1349, https://doi.org/10.1089/thy.2010.0178 (2010).
Tibshirani, R. The lasso method for variable selection in the Cox model. Stat Med 16, 385–395 (1997).
Kim, J. H. Estimating classification error rate: Repeated cross-validation, repeated hold-out and bootstrap. Computational Statistics & Data Analysis 53, 3735–3745, https://doi.org/10.1016/j.csda.2009.04.009 (2009).
Acknowledgements
This study was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) by the Ministry of Education (2016R1D1A1B03930375). This study was also supported by a CMB-Yuhan research grant of Yonsei University College of Medicine (6-2017-0170). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
J.Y.K. – conceived, coordinated, and directed all study activities, K.H. – statistical analysis, E.L. – image post-processing, curation of the radiomics-based image features, V.Y., P. –data collection, image segmentation, manuscript writing, E.K., H.J.M., J.H.Y. – acquisition of imaging data and manuscript review. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, V.Y., Han, K., Lee, E. et al. Association Between Radiomics Signature and Disease-Free Survival in Conventional Papillary Thyroid Carcinoma. Sci Rep 9, 4501 (2019). https://doi.org/10.1038/s41598-018-37748-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-37748-4
This article is cited by
-
Combined clinical variable and radiomics of post-treatment total body scan for prediction of successful I-131 ablation in low-risk papillary thyroid carcinoma patients
Scientific Reports (2024)
-
Analysis of preoperative computed tomography radiomics and clinical factors for predicting postsurgical recurrence of papillary thyroid carcinoma
Cancer Imaging (2023)
-
Ultrasound-based radiomics analysis for preoperative prediction of central and lateral cervical lymph node metastasis in papillary thyroid carcinoma: a multi-institutional study
BMC Medical Imaging (2022)
-
Relation of Carotid Plaque Features Detected with Ultrasonography-Based Radiomics to Clinical Symptoms
Translational Stroke Research (2022)
-
Implications of US radiomics signature for predicting malignancy in thyroid nodules with indeterminate cytology
European Radiology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.