Abstract
We aimed to evaluate and determine the effect of diabetes mellitus (DM) on overall survival (OS) and cancer-specific survival (CSS) in early stage cervical cancer (CC) patients. Patients with primary cervical cancer and newly diagnosed were selected from ten different cancer specialist hospitals of Malaysia. Patients’ demographic and clinical data were obtained for the prognostic analysis. Kaplan-Meier method was used to estimate patients’ survival time (CSS and OS) with DM status and values were compared using the log-rank test. A total of 19,785 newly diagnosed CC patients were registered during 2010–2016, among them only 16,946 (85.6%) with primary CC tumor. There was no difference in treatment modality between DM and non-DM patients. However intergroup assessment showed that type 2DM have significantly higher rate of mortality in both overall mortality (28.3%) and CC-specific (11.7%) as compared to Type 1DM (17.3%; 5.5%) and non DM patients (12.7%; 9.1%) (p < 0.001). Within group assessments showed that Type 2DM patients have better quality of life (mean 7.13 ± 3.67) (p < 0.001) and less distress levels (mean 2.41 ± 0.63) (p < 0.011) as compared to type1 DM (meant 10.54 ± 2.11; 3.19 ± 1.07). This study concluded that T2DM prognostic effect still remained after adjusting demographic and clinical parameters. Type 1 diabetes mellitus showed better OS and CSS then type2 DM.
Similar content being viewed by others
Introduction
Human papillomavirus (HPV -16 & 18) had a persistent link with cervical cancer among women1. World Health Organization (WHO) and Global Cancer incidence (GLOBOCAN) estimated that cervical cancer (CC) is ranked 2nd for most common cancer worldwide among women with annual incidence of 5.28 million and mortality 2.66 million each year1. About 87% deaths of these cases occurs among women living in developing countries1. Women with HIV are at high risk of developing CC2, early diagnosis of CC proven to have good prognosis and low rates of mortality3. With the help of cytological and molecular screening, early stage diagnosis is possible. In this regard WHO advocates a comprehensive approach to CC prevention & control strategies to identify and deliver effective care4.
Malaysia had estimated 4,696 reported cases of CC annually1, ministry of health Malaysia stated an average of 2000–3000 hospital admissions of CC annually in the country; and majority of them presenting with late stages of the disease5. According to latest Malaysian consensus approximately 2,145 new CC cases are diagnosed annually, it is the 2nd most common cancer among women aged 15–44 years in Malaysia6. This report also stated that about 621 CC-specific deaths occur annually in Malaysia. The CC-specific mortality rate in Malaysia is two times higher than Netherlands, United Kingdom and Finland7.
The economic burden due to CC is enormous in Malaysia, although surgery and radiotherapy proved to have high cure rates in early stage diagnosis but still several patients die with disease relapse. Several prognostic factors influence the outcome of CC including; lymph node, tumor size, stomach invasion, metastasis4,6,8. In recent years, several cohort studies and meta-analysis reported significant influence of diabetes mellitus (DM) on increased risk of cancers with different pathological pathways9,10,11. The underlying mechanism based on hypothesis-involved insulin like growth factor 1 (IGF-1). Hyperglycemia or hyperinsulinemia tends to modulate the over-secretion of free IGF-1, that leads to IGF-1Rs activation and resulting increased proliferation, invasive binding and cellular metastasis12.
Identification of IGF-1 at early stage CC reported at preclinical and clinical level but yet studies have not firmly discussed the correlation patterns of CC incidence and DM13,14,15. The pathological and clinical parameters influence on DM, however the effect of diabetes on overall survival (OS) and cervical cancer (CC)-specific (cancer-specific survival – CSS) mortality among early stage CC has not been evaluated so far. Also the concern is focused on the interrelation of diabetes related psychosocial correlates and variability in glycemic index to disease outcome as well as treatment modalities. This hospital-based survival analysis study is the first of its kind; to determine the effect of DM on survival parameters like; OS and CSS among early stage CC patients and also determine the effect to subclasses of DM., type 1 and 2 on the overall mortality and outcome. The psychosocial parameters like, quality of life tool and diabetes distress scale (DDS) were also used to determine the impact on OS and CSS among patients with early stage CC and DM.
Results
Patient Characteristics
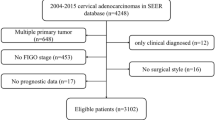
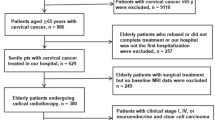
A total of 19,785 newly diagnosed CC patients were registered during 2010–2016, among them only 16,946 (85.6%) with primary CC tumor. After screening for exclusion criteria 3,797 (19.2% out of total registrations) were enrolled in the study (Fig. 1). Subgroups were DM type 1 (n = 564), DM type 2 (n = 1101) and non DM (n = 2,132). Mean age of CC diagnosis among DM type 2 patients was significantly (p < 0.001) higher than non-DM patients (Table 1). Also DM type 2 patients (Mean ± SD: 58.0 ± 19.6) have significantly (p < 0.001) less follow-up time as compared to type 1 (61.4 ± 22.3) and non-DM patients (75.4 ± 2.9) (Table 1). It was also found that patients with DM (type 1or 2) were significantly probable to develop squamous cell carcinoma (SCC) (p < 0.048), high incidences of liver and cardiopulmonary comorbidities (p < 0.001), Stage IA/IB (p < 0.002) and nodule size ≤6 cm (p < 0.021) (Table 1). There was a significant difference (p < 0.001) in treatment modality among DM and non-DM patients. Also, intergroup assessment showed that type 2DM have significantly higher rate of mortality in both overall mortality (28.3%) and CC-specific (11.7%) as compared to Type 1DM (17.3%; 5.5%) and non DM patients (12.7%; 9.1%) (p < 0.001). Within group assessments showed that Type 2DM patients have better quality of life (mean ± SD: 7.13 ± 3.67) (p < 0.001) and less distress levels (mean ± SD: 2.41 ± 0.63) (p < 0.011) as compared to type1 DM (mean ± SD: 10.54 ± 2.11; 3.19 ± 1.07).
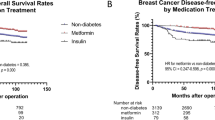
Mortality and Survival Analysis
During study duration, a total of 681 (17.9%) patients died among them 410 patients were DM (both Type 1 & 2) and rest 271 were non DM group patients. A significant (p < 0.0001) difference was reported with shorter OS time among type 2DM as compared to non DM group. Type 1 DM also showed shorter OS time compared to non DM ((p < 0.001) but slightly longer than type 2DM (Fig. 2A). Intergroup analysis showed that OS rates of 2 years were 89.1% (DM): 97.3% (non-DM); 79.6% (DM): 90.8% (non-DM) at 5 years and 75.4% (DM): 87.3% (non-DM) at 7 years respectively. Within group analysis showed that type1 DM patients OS rates were significantly higher than type2 DM patients during study follow up time 82.6% versus 71.7% (p < 0.001). Similar pattern was found with CC-specific survival analysis (Fig. 2B). However, within group assessment for type1 & 2 DM patients showed no significant difference on CCS rates during study duration.
Modeling for Probability assessment
Several variables were tested for the probability testing, and many of them showed effect on lower OS and CC-specific survival probability. Therefore, after adjusting age, stage of CC, tumor size, lymph node, comorbidities, histology and treatment modality – DM persisted as potential prognosticator of a lower OS and CSS likelihood (p < 0.001) (Fig. 2A,B). Within group assessment showed that type 2 DM patients had lower OS prospect (Adjusted HR: 1.61; 95% CI 1.45–2.59; p < 0.001) and CSS likelihood (Adjusted HR: 1.56; 95% CI 1.03–2.78; p < 0.001) as compared to non DM. Type1 DM patients also reported lower OS value (Adjusted HR: 1.23; 95% CI 1.02–1.81, p < 0.001) but CSS probability (Adjusted HR: 1.07; 95% Cl 0.47–1.96, p < 0.221) was not different from non DM group patients (Table 2).
Heterogeneity and Prognostic influence of Variables on DM
Intergroup analysis showed vital predictive effect of DM on the other variables as; age, stage, tumor size, lymph node, histology and treatment options/modality (Table 3). No significant and strong heterogeneity was found between HR of the subgroups. The ranges for adjusted HR among groups for Overall mortality were 1.023–3.12 and 0.79–3.04 for CC-specific mortality (Table 3).
Diabetes Subclass Heterogeneity Assessment
Within group assessment showed that type2 DM had prognostic influence than type 1DM, on following variables; age, tumor size, low age of diabetes diagnosis, high mean score of QOL, and glycemic index. No strong heterogeneity was reported in the findings; adjusted HR 95% CI range value for CC-specific mortality (0.85–3.34) and overall mortality (OM) (1.33–3.54) were found in the subgroups analysis (Table 4).
Discussion
In this hospital-based case-control study, findings showed that DM patients’ were exhibited adverse prognostic factors for patients with newly and early diagnosis of CC. This finding suggested that type2 DM patients had more mortality rates as compared to type 1, and also the impact on OS probability. According to multivariate analysis; type2 DM showed consistent negative prognostic effect among age (groups), different tumor size, lymph node, histology, age of diabetes diagnosis, glycemic index and treatment modalities. Therefore, type2 DM significantly lower CSS & OS rates and also remained independent predictor for lowering CSS and OS probability.
Literature have reported adverse effect of DM on early stage liver and breast cancers, thus lead to poor prognosis12,13,16 and showed increased rates of cancer-specific mortality. This study also reported similar findings with early and newly diagnosed CC patients. In addition to these findings, our study also managed to differentiate the prognostic impact in terms of DM subclasses and related social variables. Past studies reported that CC, breast and livers cancers exhibits high level of IGF-1R overexpression17,18. Also IGF-1 levels showed positive association with CC risk has been identified in scientific literature19, thus in clinical practice IGF-1R paly vital role to predict the clinical relevance of mortality & disease occurrence at early stages19,20.
Patients with either hyperglycemia or hyperinsulinemia might decrease the production of hepatic proteins and binding capacity subsequently increased the concentration of free IGF-1 value in the body11,12,14,20,21. Thus concurrent increased IGF-1 levels and activation of IGF axis due to excessive IGF-1R in CC cells may resulted in poor diagnosis22. This study also found that more duration of diabetes history significantly and independently lowers both CSS and OS probability (Fig. 2A,B).
The inter-group analysis showed negative impact of DM on OS and CSS, the influence was more significantly prominent among squamous cell carcinoma than adenocarcinoma (Table 3). To the current scientific understanding nearly all types of cancers with positive association to DM were adenocarcinoma histologically23. Within group assessment revealed type2 DM more oriented to such effects then type1 DM (Table 1). However, it is still unknown or unclear the effect of different DM subclasses on squamous and adenocarcinoma cells at cellular mechanism of IGF-1 levels and overexpression of IGF-1R axis. More clinical trials are required to determine the systemic pathological pathway of metastasis in adenocarcinoma with hyperglycemia and/or hyperinsulinemia.
Treatment modalities among DM patients were favorable to surgery and radiotherapy alone, other adjuvant therapies showed low OS and CSS (Tables 1 and 3). However, patients with contraindication to surgery exhibit unfavorable risk factors (e.g., inadequate glycemic control), with implied to poor prognosis. A retrospective study reported poor OS rates among obese patients with cervical cancer, and recommended radiotherapy as a primary curative therapy then surgery17,18,19,20,21,22,23,24. Also reported that obesity is an independent factor for poor prognosis among cervical cancer patients. Type2 DM patients usually present with overweight /obesity, this could impair the disease outcomes via inadequate treatment dose and/or uncontrolled glycemic index. Sub-therapeutic radiation dose (esp. lateral or oblique treatment)25 and others26 were contributing barriers in delivering optimum radiation to patients with obesity. Similarly, patients with metastatic lymph nodes and contraindicated to surgery, survival probability is influenced with sub therapeutic levels of either radiotherapy or chemotherapy. This study is limited with body mass index (BMI) values among patients due to missing data in medication profiles, but still morbid obesity is less likely reported in Asian population27 so this may slightly influence the study findings. In contrast, patients with unfavorable pathological factors received adjuvant therapy that possibility lead to high risk of disease occurrence and mortality rates.
Limitations of the study
Several above mentioned clinical variables with potential prognostic characteristics were not analyzed even it might affect the selection of treatment modalities among early and newly diagnosed CC patients with DM.
Conclusion
This study concluded that diabetes is the potential independent variable for lowering OS and CSS probability among newly diagnosed Cervical cancer patients. Diabetes type 2 mellitus prognostic effect still remained after adjusting demographic and clinical parameters. Type 1 diabetes mellitus showed better OS and CSS than type2 DM. Patient age and duration of diabetes reduced OS and CSS probability in patients with type2 DM then non-diabetes. Hyperglycemic index and poor QOL in patients with DM reported high rates of OS and CSS then non-diabetic patients.
Practice Implications
This study predicts the prognostic implication of DM for the newly diagnosed early stage CC patient. Findings reported that type 2 DM may increase the risk of cancer relapse and decrease OS even after initiating treatment modalities. Hyperglycemic index and poor QOL in patients with DM reported high rates of OS and CSS then non-diabetic patients. Thus incorporating DM care model in the treatment plan would improve the continuum of care.
Methodology
Ethics Approval
The study was performed in compliance with the WMA [World Medical Association] Declaration of Helsinki: Ethical principles for medical research involving human subjects amended by 59th WMA (number PHRC/HC/11/13), 2013 Seoul, Korea. Study was approved by Clinical Research Committee (CRC), Ministry of Health (MOH) (id: NMRR-10-776-6941), Malaysia. This study protocol followed the Good Clinical Practice (GCP) guidelines, MOH, Malaysia.
Data Collection
Patients with primary cervical cancer and newly diagnosed between Jan-2010 till Dec-2016 were selected from ten different cancer specialist hospitals of Malaysia. These hospitals located in all the major cities of Malaysia thus covers >90% of total cervical cancer (CC) patients except eastern states i.e., Sabah and Sarawak. Bi-annual follow-up with all the enrolled patients were scheduled throughout the study duration to collect data on clinical and relative parameters. All the patients were required to sign a mandatory written consent form. Principle investigator ensured the anonymity and privacy of each patient. Patients’ identities were encrypted and all the data was analyzed anonymously. Informed consent form was also obtained from all the participants at the time of enrollment.
Patient demographic, clinical and pathological status, treatment plans, glycemic index, quality of life relative to diabetes management and comorbidities were obtained for the prognostic analysis. Information and medical records were linked-up with Malaysian death registry to identify and validate the mortalities between 2010 (Jan) and 2017 (May).
Patients Characteristics and Recruitment
Newly diagnosed primary cervical cancer patients were recruited with inclusion criteria; age >40 years; cervical cancer as primary tumor; stage I-IIA (American Joint Cancer committee –Cancer system (6th edition)28 and received curative treatment. Patients were excluded on: cancer history, multiple primary cancers, pathological findings reported other than squamous cell carcinoma or adenocarcinoma, patients with neoadjuvant therapy or unknown treatment modality and either positive or unknown surgical margin.
Primary and Secondary Endpoints and Definitions
International Classification of Diseases, 9th edition for clinical modifications (ICD-9-CM) codes was used to screen Diabetes mellitus (DM) and other comorbidities in the study population. The diagnosis codes for in-patient and outpatient clinics were included and also Deyo-Charlson comorbidity index were examined29. The DM diagnosis either type 1 or type 2 was established if it was reported at least two times in out-patient clinics at different months or at least once in in-patient hospital stay within 1 year. General physician calculated the duration of DM on the basis of first confirmed diagnosis and then counter validated either by patient or caregiver and/or family members. Secondary sources also included ministry of health online repository. Comorbidities were coded and analyzed as dichotomized variable (YES/NO). Followings are the ICD-9-CM codes for comorbidities;
-
a.
Type 1 DM (ICD-9-CM code 250.01)
-
b.
Type 2 DM (ICD-9-CM code 250.x)
-
c.
Mild liver disease (ICD-9-CM codes 571.2,571.4–571.6)
-
d.
Chronic Pulmonary Disease (ICD-9-CM codes 416.8, 416.9, 490.x–505.x, 506.4, 508.1, 508.8)
-
e.
Congestive heart failure (ICD-9-CM codes 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 425.4–425.9, 428.x)
-
f.
Renal disease (ICD-9-CM codes 403.01, 403.11, 403.91, 404.02, 404.03, 404.12, 404.13, 404.92, 404.93, 582.x, 583.0–583.7, 585.x, 586.x, 588.0, V42.0, V45.1, V45.x)
-
g.
Cerebrovascular disease (ICD-9-CM codes 362.34, 430.x–438.x)
-
h.
Dementia (ICD-9-CM codes 290.x, 294.1, 331.2)
Patients received chemotherapy (CT) or radiotherapy (RT) or combinations within 90 days of surgery were considered as adjuvant therapy/treatment. Participants were observed and scheduled follow-up from the primary diagnosis (CC) to mortality based on Cancer-specific survival (CSS) and death from any cause overall survival (OA) also based on the last follow-up date in the medication profile or hospitals database (i.e., 31st May, 2017).
Follow-up assessments were also included; HbA1c value, Euro quality of life assessment scale (EuroQOL-5D-3L)30, Diabetes Distress Scale (DDS-17)31. These assessments were made to identify the psychosocial and glycemic variability impact on CC mortality & survival probability. These assessments were collected bi-annually from patients and values were provided in the prognostic analysis.
Statistical analysis
The baseline values of characteristics were evaluated by using either one-way analysis of variance (continuous variables) or Chi-square test (nominal variables). Kaplan-Meier method was used to estimate patients’ survival time (CSS and OS) with DM status (type 1 & type 2) and values were compared using the log-rank test. The effect of DM (including subclasses) and further potential risk factors were evaluated using Cox proportional hazards model with adjusted Hazard ratios and 95% confidence intervals. All the primary and secondary variables were included in the analysis to determine the effect and consistency of DM (both type 1& type 2) on mortality among study population. A p value less than 0.05 (two-sided) was considered statistically significant. Statistical Package for Social Sciences (SPSS ® 22 version) was used to perform analysis.
Data Availability
Data is available with reasonable request to principle investigator Dr. Syed Wasif Gillani.
References
Globocan. Cervical Cancer: Estimated Incidence, Mortality and Prevalence Worldwide in 2012 [Internet]. International Agency for Research on Cancer (IARC); 2012. Preprint at, http://globocan.iarc.fr/old/FactSheets/cancers/cervix-new.asp (2015).
Frisch, M. Human Papillomavirus-Associated Cancers in Patients With Human Immunodeficiency Virus Infection and Acquired Immunodeficiency Syndrome. J Natl Cancer Inst. 92(18), 1500–10 (2000).
Hawes, S. E. et al. Incident high-grade squamous intraepithelial lesions in Senegalese women with and without human immunodeficiency virus type 1 (HIV-1) and HIV-2. J Natl Cancer Inst. 98(2), 100–9 (2006).
World Health Organization (WHO). Comprehensive cervical cancer prevention and control: a healthier future for girls and women [Internet]. 2013. Preprint at, http://apps.who.int/iris/bitstream/10665/78128/3/9789241505147_eng.pdf?ua=1 (2015).
Devi, B. C. R., Tang, T. S. & Gerard, L. C. Preliminary results from the pilot study on the National Cancer Patient Registry–Cervical Cancer. Med J Malaysia. 63(Suppl C), 63–65 (2008).
Bruni, L. et al. ICO Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Malaysia. Summary Report 27 July 2017. Preprint at, http://www.hpvcentre.net/statistics/reports/XWX.pdf (2017).
Zaridah, S. A Review of Cervical Cancer Research in Malaysia. Med J Malaysia. 69(Supplement A), 33–41 (2014).
Rotman, M. et al. A phase III randomized trial of postoperative pelvic irradiation in stage IB cervical carcinoma with poor prognostic features: Follow-up of a gynecologic oncology group study. Int J Radiat Oncol Biol Phys. 65, 169–176 (2006).
Vigneri, P. et al. Diabetes and cancer. Endocr Relat Cancer. 16, 1103–1123 (2009).
Yood, M. U. et al. Incidence of cancer in a population-based cohort of patients with type 2 diabetes. Diab Met Syndr Clin Res Rev. 3, 12–16 (2009).
Atchison, E. A. et al. Risk of cancer in a large cohort of U.S. veterans with diabetes. Int J Cancer. 128, 635–643 (2011).
Law, J. H. et al. Phosphorylated insulin-like growth factor-i/insulin receptor is present in all breast cancer subtypes and is related to poor survival. Cancer Res. 68, 10238–10246 (2008).
Shen, M. R. et al. Insulin-like growth factor 1 is a potent stimulator of cervical cancer cell invasiveness and proliferation that is modulated by alphavbeta3 integrin signaling. Carcinogenesis. 27, 962–971 (2006).
Huang, Y. F. et al. Clinical implications of insulin-like growth factor 1 system in early-stage cervical cancer. Br J Cancer. 99, 1096–1102 (2008).
Wideroff, L. et al. Cancer incidence in a population-based cohort of patients hospitalized with diabetes mellitus in Denmark. J Natl Cancer Inst. 89, 1360–1365 (1997).
Shau, W. Y. et al. Diabetes mellitus is associated with increased mortality in patients receiving curative therapy for hepatocellular carcinoma. The Oncologist. 17, 856–862 (2012).
Desbois-Mouthon, C. et al. Insulin-like growth factor-1 receptor inhibition induces a resistance mechanism via the epidermal growth factor receptor/HER3/AKT signaling pathway: Rational basis for cotargeting insulin-like growth factor-1 receptor and epidermal growth factor receptor in hepatocellular carcinoma. Clin Cancer Res. 15, 5445–5456 (2009).
Shimizu, C. et al. Expression of insulin-like growth factor 1 receptor in primary breast cancer: Immunohistochemical analysis. Hum Pathol. 35, 1537–1542 (2004).
Lee, S. W. et al. Plasma levels of insulin-like growth factor-1 and insulin-like growth factor binding protein-3 in women with cervical neoplasia. J Gynecol Oncol. 21, 174–180 (2010).
Steller, M. A. et al. Overexpression of the insulin-like growth factor-1 receptor and autocrine stimulation in human cervical cancer cells. Cancer Res. 56, 1761–1765 (1996).
Luo, M. et al. MicroRNA-497 is a potential prognostic marker in human cervical cancer and functions as a tumor suppressor by targeting the insulin-like growth factor 1 receptor. Surgery. 153, 836–847 (2013).
Kuo, H. Y. et al. The prognostic impact of type 2 diabetes mellitus on early cervical cancer in Asia. The Oncologist. 20, 1051–1057 (2015).
Powell, D. R. et al. Insulin inhibits transcription of the human gene for insulin-like growth factor-binding protein-1. J Biol Chem. 266, 18868–18876 (1991).
Ooi, G. T. et al. Insulin rapidly decreases insulin-like growth factor-binding protein-1 gene transcription in streptozotocin-diabetic rats. Mol Endocrinol. 6, 2219–2228 (1992).
Frumovitz, M. et al. Morbid obesity as an independent risk factor for disease-specific mortality in women with cervical cancer. Obstet Gynecol. 124, 1098–1104 (2014).
Wong, J. R. et al. Potential for higher treatment failure in obese patients: Correlation of elevated body mass index and increased daily prostate deviations from the radiation beam isocenters in an analysis of 1,465 computed tomographic images. Int J Radiat Oncol Biol Phys. 75, 49–55 (2009).
Griggs, J. J. et al. Appropriate chemotherapy dosing for obese adult patients with cancer: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 30, 1553–1561 (2012).
Greene, F. L. et al. AJCC Cancer Staging Handbook. 6th ed. New York, NY: 100–165 (Springer, 2002).
Deyo, R. A., Cherkin, D. C. & Ciol, M. A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 45, 613–619 (1992).
EuroQOL. Euro-QOL – a new facility for the measurement of health-related quality of life. Health Policy. 13(3), 199–208 (1990).
Fisher, L., Hessler, D. M., Polonsky, W. H. & Mullan, J. When is diabetes distress clinically meaningful? Establishing cut-points for the Diabetes Distress Scale. Diabetes Care. 35, 259–264 (2012).
Acknowledgements
We would like to acknowledge the efforts of technical and nursing staffs of the hospitals to help us in collecting data. No employment conflict. I (Dr. Syed Wasif) was employed to USM, Malaysia at the time to initiate this research project, however currently I am employed to Taibah University, Saudi Arabia.
Author information
Authors and Affiliations
Contributions
S.W.G. concept and design, principle investigator, writing manuscript. H.A.Z. & I.A.A. provision of study materials and population. M.I.M.A. & S.A.S.S. data collection and assembly of data. M.R.B. content analysis and interpretation. H.A.R. copy editing and final drafting. All the authors have approved the contents of manuscript and allowed to send for peer-review and publication.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gillani, S.W., Zaghloul, H.A., Ansari, I.A. et al. Multivariate Analysis on the Effects of Diabetes and related Clinical Parameters on Cervical Cancer Survival Probability. Sci Rep 9, 1084 (2019). https://doi.org/10.1038/s41598-018-37694-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-37694-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.