Abstract
The aim of current study was to assess the effects of Baduanjin exercise on cerebrovascular function, cardiac structure and cardiac function, static pulmonary function, traditional risk factors of CVD and the related psychological outcomes in older community adults at risk for ischaemic stroke. A randomized controlled trial was conducted in three community between November 2013 and October 2015. Older community-dwelling adults (N = 170) were randomly allocated into either a Baduanjin training (5 × 60 min/weekly) or control group who kept their unaltered lifestyle during a 12-week intervention period. Primary (cerebral haemodynamic parameters) and secondary outcomes (cardiac structure, cardiac function, static pulmonary function, traditional risk factors and the related psychological outcomes) were measured at baseline, after a 12-week intervention period and after an additional 12-week follow-up period. After the 12-week intervention period and additional 12-week follow-up period, the Baduanjin exercise group displayed significant changes in most cerebral haemodynamic parameters compared to the control group: lower systolic blood pressure, diastolic blood pressure, plasma total cholesterol levels, waist circumference, hip circumference and waist/hip ratio; and improved mood, self-confidence, self-esteem, quality of life and sleep quality. A supervised 12-week Baduanjin exercise intervention was effective and safe in modulating cerebral haemodynamics, reducing blood pressure and improving anthropometric parameters and related psychological outcomes in older community adults at risk for ischaemic stroke.
Similar content being viewed by others
Introduction
Ischaemic stroke remains the leading cause of long-term disability in adults worldwide1. Although age-standardized mortality of stroke have decreased around the world in the past twenty years, the absolute number of people suffering from stroke is increasing, and its impact is likely to dramatically increase in the future because of the ageing population and health transitions observed in developing countries2,3. Currently, no country in the world has exhibited a substantial reduction in stroke burden in terms of the absolute number of people affected by and/or dying from stroke. This implies that it is important to make efforts to prevent stroke, particularly the establishment of effective primary prevention strategies for older community adults.
Studies have demonstrated that stroke and most other cardiovascular diseases can be prevented4. The most effective means available for stroke prevention involve the control of modifiable risk factors5,6. According to the INTERSTROKE study, ten risk factors, including vascular risk factors, unhealthy diet and physical inactivity, account for 90% of the population-attributable risk of stroke, and most of them are modifiable risk factors7,8. It is well known that more than 50% of strokes could be prevented through the control of modifiable risk factors9. Even so, their preventive mechanisms remain unclear, which may limit the efficacy of primary prevention.
In terms of aetiology, the direct cause of ischaemic stroke is associated with intracranial atherosclerotic stenosis and the disruption of atherosclerotic plaques with subsequent thromboembolism10. The downstream cerebral haemodynamic changes and the cerebrovascular reserve may play an important role11. For example, the narrowing cerebral vasculature resulting from cerebral intracranial atherosclerosis can cause a reduction in cerebral perfusion pressure (CPP), and the subsequent autoregulation of the vasculature will maximally dilate the cerebral arterioles to maintain cerebral blood flow (CBF). However, with the further reduction in CPP and the maximally dilated arterioles, CBF will also decrease and potentially increase the risk of stroke12. Therefore, cerebral haemodynamic impairment is considered an important pathophysiological mechanism involved in ischaemic stroke. CBF depends on arterial blood pressure, cerebrovascular resistance, and the distribution of cardiac output. CBP is rigorously regulated by a set of mechanisms that include cerebral autoregulation, neurovascular coupling and cerebrovascular carbon dioxide and oxygen reactivity to safeguard the balance of cerebral metabolic demand and supply13,14. Studies have suggested that an increase in cerebrovascular resistance and a decrease in CPP could cause a reduction in cerebral blood flow15, whereas a slight alteration in cardiac output could also lead to changes in CBF despite blood pressure remaining stable or within the autoregulatory range16. Generally, traditional risk factors of ischaemic stroke, such as ageing, hypertension, diabetes, and lipid disorders, are associated with these conditions. For example, diabetes is associated with an increased risk of cerebral autoregulation dysfunction, whereas poorly controlled hypertension is related to a decline in CBF17,18. Normal ageing is linked to marked structural and functional alterations in the cerebrovascular system19. Recent studies have indicated that an estimated 30% of older community adults over 65 years old suffer from intracranial atherosclerotic stenosis (ICAS), as determined by magnetic resonance angiography20, and that more than 90% of individuals with ICAS have at least one vascular risk factor of cardiovascular disease (CVD)21. Therefore, controlling traditional cardiovascular risk factors and their appropriate treatment are vital to establishing primary preventive strategies of stroke by improving the direct aetiology of ischaemic stroke.
Current evidence clearly shows that exercise or physical activity is an effective intervention for preventing ischaemic stroke or other cardiovascular diseases. Therefore, the American Heart Association (AHA) and American College of Cardiology (ACC) recommend that adults should participate in at least 3 sessions of aerobic physical activity of moderate or vigorous intensity lasting an average of 40 minutes each week22,23. However, fewer than 50% of adults, particularly adults over the age of 60, achieve this recommendation despite the broad recognition of its benefits24. As one of the traditional Chinese Qigong exercises, Baduanjin exercise consists of eight separate, delicate and smooth movements; it is a low-moderate intensity mind-body exercise that has been practised in China for hundreds of years25. Current studies have suggested that Baduanjin training appears to have substantive benefits for older adults and is an appropriate exercise for older community people26,27. Many significant improvements have been reported in balance, strength and flexibility as well as in sleep quality and psychological and mental health28,29,30. Recently, an increasing number of studies have demonstrated the benefits of regular Baduanjin practise in reducing blood pressure, insulin resistance and blood glucose levels as well as in controlling traditional CVD risk factors31,32,33. However, the effects of Baduanjin exercise on the aetiology of ischaemic stroke, such as cerebral haemodynamics in older community people, have not been studied yet. The aim of this study was to conduct a randomized controlled trial to examine the effects of Baduanjin exercise on cerebrovascular functions, cardiac structure and function, static pulmonary function, physical fitness, traditional risk factors of CVD, quality of life and sleep quality in older community adults at risk for ischaemic stroke.
Methods
Design and Setting
This study was a two-armed, randomized, assessor-blinded, parallel controlled trial with computer-generated randomization and the concealed allocation. It was conducted between November 2013 and October 2015 in three community centres (Wufeng, Fengdanbailu, and Chuntian) in Fuzhou, China. The participants were randomly allocated to either a Baduanjin training group or usual physical activity group at a 1:1 ratio. Ethics approval was obtained from a local ethics committee in the Affiliated People’s Hospital of Fujian University of Traditional Chinese Medicine (No. 2013-021-02). This study was performed in accordance with the Declaration of Helsinki. The trial has been registered in the Chinese Clinical Trial Registry (ChiCTR-TRC-13003588). The design of this study was described in further detail in the published study protocol34.
Participants
The participants were at a high risk of ischaemic stroke according to the “2012 annual screening and intervention project workbook for population with high risk of stroke”35. To be eligible, participants had to be aged 50 to 75 years and not have regularly exercised for at least one year (regular exercise was defined as one exercise that is practised for 30 minutes or longer each time at least three times per week for more than 3 months). Participants were excluded if they suffered from severe cerebrovascular diseases, musculoskeletal system diseases or other sport contraindications or if they had a history of stroke or a communication disorder.
The trial was advertised by posters or leaflets or by establishing a free clinic at the community centres. The community adults who were interested in this trial were assessed by two trained research assistants in the lounge room based on the eligibility criteria, and they were informed regarding the overall design of this study. If the subjects were eligible and agreed to participate, their baseline measurements were acquired after signing the written informed consent.
Practiced the Baduanjin exercise and practiced Baduanjin form
Participants in the Baduanjin training group gathered in their community centres and practised the Baduanjin exercise that originated from the “Health Qigong Baduanjin Standard” established by the State Sports General Administration in 200336. Two certified instructors instructed and supervised their training. The training programme was comprised of 60 minutes per session with five sessions per week for 12 weeks. Each session consisted of 45 minutes of Baduanjin form, a 10-minute warm-up and a 5-minute cool-down. Two research assistants managed the training spot and recorded the participants’ attendance. The participants in the control group were informed to maintain their usual physical activity during the 12-week intervention period.
Following the 12-week intervention period, participants of both the Baduanjin training and control groups entered an additional 12-week unsupervised follow-up period in which no additional exercise intervention was administered to any participant.
In addition, all participants were asked to keep a daily diary of physical activity level during the 12-week intervention period and the additional 12-week follow-up period. The physical activity level was assessed by using self-reported form, in which the duration and intensity of physical activity for each individual in a whole day was classified into three sections including the duration of low-intensity activity (e.g. walking, drop around, walk the dog), the duration of moderate-intensity activity (e.g. brisk walking, square dances, housework), and duration of high-intensity activity (jogging, play ball, swimming).
Measures
The primary and secondary outcomes were assessed at baseline (−2 to −1 week), the end of the intervention (13 weeks) and the end of the additional 12-week follow-up period (25 weeks). All measurements were performed by the professional operators who did not know the allocation group at the Fujian University of Traditional Chinese Medicine Subsidiary Rehabilitation Hospital.
The primary outcomes of this trial were cerebrovascular function, consisting of cerebral haemodynamics and cerebrovascular elasticity. Cerebral haemodynamics was expressed by the maximum blood flow velocity (BFVmax), minimum blood flow velocity (BFVmin) and mean blood flow velocity (BFVmean) parameters, whereas cerebrovascular elasticity was expressed using the vascular pulsatility index (PI, calculated using following formula: (peak systolic velocity - end-diastolic velocity)/mean flow velocity)) and the vascular resistance index (RI, calculated by following formula: (peak systolic velocity – end-diastolic velocity)/end-diastolic velocity)). Those variables were measured in nine main cerebral arteries, including the bilateral vertebral artery (VA), bilateral middle cerebral artery (MCA), bilateral anterior cerebral artery (ACA), bilateral posterior cerebral artery (PCA) and basilar artery (BA), using a colour Doppler ultrasound imaging device (Philips, product type: IU22).
The secondary outcomes were cardiac structure and cardiac function, static pulmonary function, traditional risk factors of CVD and psychological outcomes. Cardiac structure and cardiac function were measured using the colour Doppler ultrasound imaging device (product type: SIEMENS Acuson X300). Static lung function was measured using cardiopulmonary function instruments (JAEGER, Germany, product type: OXYCON PRO PC). Traditional risk factors of CVD include blood pressure, heart rate, plasma indicators and anthropometric measurements. The blood pressure was measured manually by the professional staff at the hospital. The plasma indicators of CVD include blood lipid and fasting blood glucose, which were measured quantitatively using an automatic analyser according to the specifications of the fasting period using kit (Rongshen, Shanghai) and enzymatic method (NSA-400, Shenyang). The anthropometric measurements include body mass index (BMI, calculated by weight (kg)/height (m2)), waist circumference, hip circumference and waist-to-hip ratio (waist circumference (cm)/hip circumference (cm)), which were measured using a body scale for BMI and a metric ruler for waist circumference and hip circumference. The related psychological outcomes, including mood, self-confidence and self-esteem, quality of life and sleep quality, were assessed using the Brief Profile of Mood States (BPOMS), the Rosenberg Self-Esteem Scale, the Chinese version of the Social Functioning 36 (SF-36) scale and the Pittsburgh Sleep Quality Index (PSQI), respectively.
Sample Size and Statistical Analysis
A priori sample size calculation was based on an anticipated 10% improvement in cerebral haemodynamic parameters among participants undergoing the 12-week Baduanjin training compared to those in the control group. 85 participants per group was determined a priori based on a 1:1 treatment allocation, considering the target effect size detected, a significance level of 0.05 (type I error), an analysis power of 90% (type II error of 0.10), and a maximum loss to follow-up of 15%34.
All statistical analyses were conducted by a blinded statistician using the IBM SPSS 21.0 (IBM Inc., Chicago, IL, USA) statistical software package. A two-sided p value of less than 0.05 was considered significantly different. Baseline characteristics between the two groups were analysed using the t test or the Mann-Whitney test for continuous variables and Pearson’s χ2 test for categorical variables. Using the linear mixed models based on the intention-to-treat (ITT) principle, a multiple analysis assessed the changes in cerebrovascular function, cardiopulmonary function, plasma traditional risk indicators of CVD, anthropometric measurements, quality of life, happiness, mood and sleep quality from baseline to the endpoint of the intervention or from baseline to the endpoint of follow-up between the Baduanjin group and the control group. The main between-group effect (2 levels: Baduanjin vs control) and interaction effect for group and time point (3 levels: baseline, 12 weeks and 24 weeks) were treated as fixed effects with time and a repeated fixed effect, whereas the participants were random variables. The baseline data and comparison group were used as the reference variable. A fully unstructured variance-covariance matrix was assumed for the error terms. Missing data were imputed using the multiple imputation method based on the Fully Conditional Specification (FCS) algorithm.
Results
Participant Characteristics at Baseline
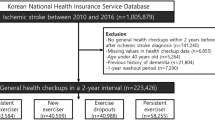
Figure 1 outlines the flow of participants during the trial. Recruitment started on 1 November 2013 and was completed on 28 February 2014. A total of 2,263 older community adults were assessed for eligibility, and 2,093 individuals were excluded because of conflicts with the eligibility criteria or because they were unwilling to participate. In total, 170 eligible participants were randomized into either the Baduanjin training group or the usual physical activity control group with an equal allocation rate. The baseline characteristics were similar between groups (Table 1).
Compliance
Of the 170 participants who completed the baseline assessment, 168 (98.8%) performed the post-intervention evaluation, and 148 (87.1%) completed the 12-week follow-up. The dropout rate was significantly higher in the control group than in the Baduanjin training group according to Pearson’s Chi-square test (χ2 = 5.221, P = 0.04), but no significant difference was found in the baseline characteristics except for fibrillation atrial in between the subjects who dropped out in the study and the subjects who completed the whole study.
Daily Physical Activity During Study Period
Table 2 presents the daily physical activity between Baduanjin training group and control group during study period. The average duration of low intensity activity was not significantly different between the two groups during the study period. The average duration of moderate intensity activity in the Baduanjin exercise group was higher than that for the control group. No high intensity physical activity was reported during the study period.
Cerebrovascular Haemodynamic Parameters
Table 3 presents the changes in haemodynamic parameters, including the maximum, minimum and mean blood flow velocities (BFVmax, BFVmin and BFVmean) and the PI and RI in the cerebral basilar arteries (BAs), bilateral vertebral arteries (LVA and RVA), bilateral anterior, and middle and posterior arteries (LAA, RAA, LMA, RMA, LPA and RPA) at baseline, at 12 weeks post-intervention and after an additional 12 weeks of follow-up. There was no significant difference in any parameters between the groups at baseline. Linear mixed models with repeated measures showed a significant interaction effect of group (intervention) by time in the PI and RI parameters for all the measured cerebrovascular arteries; in BFVmax for BA, RVA and LAA; and in BFVmin and BFVmean for the BA, LVA and RVA. A significant main effect of group in RI for BA; in BFVmax for LVA, and in BFVmean for RMA was observed. These results indicated a significant improvement in those cerebrovascular haemodynamic parameters in the Baduanjin exercise group compared with the control group. After the 12-week intervention, a significant difference between the groups was found in almost all parameters except for the RI in the BA and RMA, BFVmean in the RVA; BFVmax in the RMA; and BFVmax, BFVmix and BFVmin in the LAA, LMA and RPA. A significant difference between the groups was also determined in all the measured parameters except BFVmax in the RPA, BA and LVA; BAFmean and BAFmin in the RAA; and five haemodynamic parameters (BFVmax, BFVmin, BFVmean, PI and RI) in the LPA after the additional 12-week follow-up period. Furthermore, the differences showed that those parameters were significantly lower in the Baduanjin intervention group than in the control group (Table 3).
Cardiac Structure, Cardiac Function and Static Pulmonary Function
We found no significant differences in all parameters of cardiac structure and function and static pulmonary function, including left atrial diameter, right ventricular diameter, left ventricular ejection fraction, minute ventilation volume, vital capacity and maximal voluntary ventilation, between the Baduanjin exercise group and the control group, whereas a significant interaction of group by time was also not identified by the mixed linear model analysis (Table 4).
Traditional Risk Factors of Cerebrovascular Diseases
A significant main effect of group and interaction effect of group by time in the plasma risk factors including the total cholesterol (TC), triglyceride (TG), low density lipoprotein (LDL-C), high density lipoprotein (HDL-C), fasting blood glucose (FBG) and homocysteine (Hcy) was not observed (Table 5).
Among the four measured anthropometric measurements, including body mass index (BMI), waist circumference (WC), hip circumference (HC) and waist/hip ratio, the mixed linear model showed a significant interaction of group by time and main effect of group on WC, HC and the waist/hip ratio; three (WC, HC and the waist/hip ratio) were significantly lower in the Baduanjin training group than in the control group at post-intervention or after the additional 12-week follow-up (Table 5).
For the systolic blood pressure (SBP) and diastolic blood pressure (DBP), the analysis of mixed linear model method showed obviously significant interaction effect of group by time (P < 0.001 and P = 0.023, respectively). The SBP and DBP values were significantly lower in the Baduanjin training group than in the control group at post-intervention (P < 0.001 for SBP and P = 0.044 for DBP), and this effect in SBP was maintained after the additional 12-week follow-up (P < 0.001). No significant main effect of group and interaction effect of group by time in heart rate was observed. These results are listed in Table 5.
The Related Psychological outcomes
The measured psychological outcomes include mood, self-confidence, self-esteem, quality of life and sleep quality. A significant interaction effect of group by time and the main effect of group in all of those measured psychological outcomes were observed based on the mixed linear model analysis. In addition, we also found that all those outcomes in the Baduanjin training group were significantly superior to those in the controls at both post-intervention or after the additional 12-week follow-up (Table 6).
Adverse Events
No adverse events were reported during the exercise training or follow-up period.
Discussion
Main Findings
Compared with the control group, the 12-week Baduanjin training group showed a significant reduction in most of the cerebral haemodynamic parameters, particularly PI and RI, in nine measured cerebral arteries. Furthermore, most of those significant effects were sustained in the additional 12-week follow-up. We also found an obvious reduction in SBP, DBP, heart rate and anthropometric measurements, including WC, HC and the waist/hip ratio, and an obvious improvement in the related psychological or mental outcomes, including mood, self-confidence, self-esteem, sleep quality and quality of life, in the Baduanjin training group after the 12-week intervention or the additional 12-week follow-up.
Cerebrovascular Haemodynamic Changes
Generally, normal ageing will cause marked structural and functional alterations in the cardiovascular and cerebrovascular systems, which may be linked to reductions in global CBF37. However, regular aerobic exercise can increase long-term CBF. The mechanisms are related to that aerobic exercise can enhance systemic arterial endothelial function, reduce large elastic artery stiffness and risk of arterial atherosclerosis in middle-aged and older adults38,39. The findings in this study show that the blood velocity of most measured cerebral arteries in the Badjanjin training group were significantly lower than in the control group. Those results seem to indicate that CBF is lower in the intervention group than in the control group, which conflicts with previous studies that showed that regular aerobic exercise was associated with elevated CBF in adults40,41. However, the resting CBF changes are tightly coupled to neuronal activity via adjustments in vascular resistance15, and they are easily influenced by physiological or psychological factors42. In our study, we also observed that the PI and RI of almost all measured arteries were significantly lower in the Baduanjin training group than in the control group. Furthermore, the observed psychological or mental variables including mood, self-confidence, self-esteem, sleep quality and quality of life were better in the Baduanjin training group than in the control group and may be a reasonable explanation for the findings in this study. In addition, low-intensity aerobic exercise may not directly affect the cerebrovascular blood velocity or cause CBF changes, and an increase in exercise intensity up to nearly 60% of the maximal oxygen uptake can result in elevations in CBF43. Ainslie PN, et al. reported that regular aerobic-endurance exercise (vigorous road running or cycling races more than 4 times per week) is associated with higher blood flow velocity in the MCA40. This study used rigorously screened healthy humans to avoid the known effects of prevalent age-related diseases on CBF. Another cross-sectional study also reported that over 150 minutes of moderate- to vigorous-intensity aerobic activity per week sustained during the adult lifespan can maintain aerobic fitness throughout the lifespan and improve cerebral haemodynamics later in life44. Baduanjin is a traditional Chinese Qigong exercise with a low exercise intensity. It consists of eight separate, delicate and smooth movements. Practising Baduanjin requires body-mind coordination by combining body posture, movement and breathing with meditation45. Therefore, we speculated that 12 weeks of regular Baduanjin training might improve cerebrovascular compliance by reducing the resistance of cerebral arteries due to relaxed body-mind training, thus resulting in a decrease in cerebral blood velocity.
Cardiopulmonary Structure and Function
Cardiorespiratory capacity is typically associated with cerebrovascular diseases, and low cardiorespiratory capacity is an independent risk factor of ischaemic stroke46. Regular physical activity, particularly aerobic exercise, can substantially improve cardiorespiratory capacity, not only among healthy older adults but also among patients with chronic diseases, by improving cardiac structure, cardiac function and lung function47,48,49. However, no significant differences were found in the outcomes of cardiopulmonary structure and function between groups in the present study. A possible explanation is that the 12-week Baduanjin exercise intervention period may not have been sufficiently long to identify significant differences in those parameters among older community-dwelling adults at risk for ischaemic stroke.
Blood Pressure, Heart Rate, Plasma Risk Factors and Anthropometric measurements
We observed significantly lower SBP after the 12-week Baduanjin training intervention and the additional 12-week follow-up. We also observed lower DBP and heart rate after 12 weeks of the Baduanjin intervention in community elderly adults at a high risk of ischaemic stroke in the Baduanjin training group compared to the control group. DBP and heart rate did not differ between the groups after the additional 12-week follow-up. High blood pressure in elderly adults is associated with an increased risk of ischaemic stroke and thus must be controlled. Li et al.50 did not observe effects on blood pressure in healthy adults with normal pressure after 16 weeks of Baduanjin training in their RCT, but a recent systematic review of 8 RCTs reported the beneficial effect of Baduanjin training combined with antihypertensive drugs versus antihypertensive drug use alone among patients with hypertension32. In our study, 54.1% of the participants (46/85) in the Baduanjin exercise group had hypertension, and 50.6% (43/85) of the patients in the control group had hypertension. Therefore, our findings indicate the efficacy of Baduanjin training as a management method for hypertension.
Plasma risk factors of ischaemic stroke include TC, TG, LDL, HDL, FBG and Hcy and were measured in our study, but no significant differences were found between groups except for the TC level, which was lower in the Baduanjin exercise group than in the control group at post-intervention. These findings were in line with those from the Li et al. study on healthy adults48 but in conflict with our previous systematic review regarding healthy adults or patients with hyperlipidaemia33. Additional studies are necessary to ascertain whether Baduanjin training can modulate blood lipids in adults with a high risk of ischaemic stroke.
Anthropometric measurements, including WC, HC and ratio of the waist/HCs, but not BMI, were significantly decreased in the Baduanjin training group compared to the control group. Li et al. found that a 16-week Baduanjin training intervention significantly decreased BMI and skinfold thickness at the abdomen in healthy adults in their RCT, whereas no significant differences were observed between groups for waist and hip parameters50.
The Psychological or Mental Effect
To our knowledge, several previous studies have evaluated the effect of the Baduanjin training intervention on psychological outcomes among healthy adults or patients and have reported the positive beneficial results30,31. Chen et al. also observed that the 12-week Baduanjin training intervention could significantly improve sleep quality among community-dwelling older adults aged 60 years or older29. The findings in the present study are in accordance with the results of those previous studies.
Strengths and Limitations of the Study
This is the first RCT to provide empirical evidence regarding the effectiveness of traditional Chinese Qigong-Baduanjin exercise on cerebral haemodynamic parameters; cardiopulmonary structure and function; traditional risk factors of CVD; and the related psychological outcomes of ischaemic stroke among older community adults at risk of ischaemic stroke. Our sample is representative of the population at risk for ischaemic stroke because all of them were recruited from the older population in the general community. A standardized and supervised Baduanjin exercise training programme makes it easy to reproduce. Furthermore, we had thorough recordings of exercise adherence and physical activity levels in the two groups. Second, no specific exercise intervention was used in the control group, which means that the between-group differences were due to the Baduanjin exercise training.
The main limitation of our study was that nine cerebral arteries with forty-five haemodynamic parameters (five parameters per artery) were selected as the primary outcomes, which may thereby increase the risk of detecting differences between groups by chance and making type I errors. Furthermore, we indirectly assessed CBF and cerebral vascular function using the cerebral haemodynamic parameters. Although it is well established that the blood flow velocity of some cerebral arteries may be considered a reliable indicator of cerebral perfusion at rest51, the positive changes in those haemodynamic parameters may not directly lead to improvements in CBF and cerebral vascular function. Second, a double-blinded study design was not possible due to the difficulty in administration and operation. Therefore, participants in the Baduanjin training group might have had higher expectations of the intervention effect. This awareness of intervention assignment might have introduced some bias into the results. Third, the 12-week follow-up assessment may not have been long enough to observe long-term effects, such as clinical events related to ischaemic stroke. Additional long-term randomized controlled trials should be conducted to determine whether and to what extent improvements in CBF and cerebral vascular function after Baduanjin training affect disease activity and the clinical events of ischaemic stroke in older community adults. Finally, Due to the difference of percentage of fibrillation atrial between the dropped out participants and the participants finished the study, it may cause to some extent confounding effect to the main results.
Conclusion
This study demonstrated that Baduanjin significantly contributed to modulating cerebral haemodynamic parameters, reducing blood pressure and improving anthropometric parameters, mood, sleep quality and quality of life. Baduanjin exercise may be a useful and feasible strategy to reduce the risk of ischaemic stroke in older community populations.
Availability of Data and Materials
The datasets used and/or analysed during the current study are available from the corresponding author upon request.
References
Writing group members. et al. Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 121, e46–e215 (2010).
Roth, G. A. et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 372, 1333–41 (2015).
Feigin, V. L. et al. Update on the global burden of ischemic and hemorrhagic stroke in 1990–2013: the GBD 2013 Study. Neuroepidemiology. 45, 161–176 (2015).
Lackland, D. T. et al. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke. 45, 315–53 (2014).
Allen, C. L. & Bayraktutan, U. Risk factors for ischaemic stroke. Int J Stroke. 3, 105–116 (2008).
The European Stroke Organisation (ESO) Executive Committee and the ESO Writing Committee. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis. 25, 457–507 (2008).
O’Donnell, M. J. et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 376, 112–23 (2010).
Hankey, G. J. INTERSTROKE Study and the EPITHET Trial. Stroke: fresh insights into causes, prevention, and treatment. Lancet Neurol. 10, 2–3 (2011).
Di, L. S., Koch, G., Diomedi, M., Stanzione, P. & Sallustio, F. Stroke prevention: managing modifiable risk factors. Stroke Res Treat. 2012, 391538 (2012).
Zafar, A., Al-Khamis, F. A., Al-Bakr, A. I., Alsulaiman, A. A. & Msmar, A. H. Risk factors and subtypes of acute ischemic stroke. A study at King Fahd Hospital of the University. Neurosciences (Riyadh). 21, 246–51 (2016).
Gupta, A. et al. Cerebrovascular reserve and stroke risk in patients with carotid stenosis or occlusion: a systematic review and meta-analysis. Stroke. 43, 2884–91 (2012).
Bramlett, H. M. & Dietrich, W. D. Pathophysiology of cerebral ischemia and brain trauma: similarities and differences. J Cereb Blood Flow Metab. 24, 133–50 (2004).
Bor-Seng-Shu, E. et al. Cerebral hemodynamics: concepts of clinical importance. Arq Neuropsiquiatr. 70, 352–6 (2012).
Meng, L. et al. Cardiac output and cerebral blood flow: the integrated regulation of brain perfusion in adult humans. Anesthesiology. 123, 1198–208 (2015).
Grüne, F., Kazmaier, S., Stolker, R. J., Visser, G. H. & Weyland, A. Carbon dioxide induced changes in cerebral blood flow and flow velocity: role of cerebrovascular resistance and effective cerebral perfusion pressure. J Cereb Blood Flow Metab. 35, 1470–7 (2015).
Paulson, O. B., Strandgaard, S. & Edvinsson, L. Cerebral autoregulation. Cerebrovasc Brain Metab Rev. 2, 161–92 (1990).
Kim, Y. S. et al. Dynamic cerebral autoregulatory capacity is affected early in Type 2 diabetes. Clin Sci (Lond). 115, 255–62 (2008).
Muller, M. et al. Hypertension and longitudinal changes in cerebral blood flow: the SMART-MR study. Ann Neurol. 71, 825–33 (2012).
Yu, H., Huang, G.P., Yang, Z., Liang, F. & Ludwig, B. The Influence of Normal and Early Vascular Aging on Hemodynamic Characteristics in Cardio- and Cerebrovascular Systems. J Biomech Eng. 138, https://doi.org/10.1115/1.4033179 (2016).
Suri, M. F. et al. Prevalence of Intracranial Atherosclerotic Stenosis Using High-Resolution Magnetic Resonance Angiography in the General Population: The Atherosclerosis Risk in Communities Study. Stroke. 47, 1187–93 (2016).
Zhang, S. et al. Prevalence and risk factors of asymptomatic intracranial arterial stenosis in a community-based population of Chinese adults. Eur J Neurol. 20, 1479–85 (2013).
Haskell, W. L. et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 116, 1081–93 (2007).
Eckel, R. H. et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 129, S76–99 (2014).
Kernan, W. N. et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 45, 2160–236 (2014).
Koh, T. C. Baduanjin—an ancient Chinese exercise. Am J Chin Med. 10, 14–21 (1982).
Zou, L., Wang, C., Chen, X. & Wang, H. Baduanjin Exercise for Stroke Rehabilitation: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. Int J Environ Res Public Health. 15, 600 (2018).
Zou, L. et al. Mindfulness-Based Baduanjin Exercise for Depression and Anxiety in People with Physical or Mental Illnesses: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 15, 321 (2018).
Zeng, Y. G., Zhou, X. Q., Wang, A. L., Yang, B. & Wang, S. T. Research on the impacts of fitness Qigong Baduanjin on figure and physical function among the middle-aged and aged people. J Beijing Sport Univ. 9, 1207–1209 (2005).
Chen, M. C., Liu, H. E., Huang, H. Y. & Chiou, A. F. The effect of a simple traditional exercise programme (Baduanjin exercise) on sleep quality of older adults: a randomized controlled trial. Int J Nurs Stud. 49, 265–273 (2012).
Cheng, F. K. Effects of Baduanjin on mental health: a comprehensive review. J Bodyw Mov Ther. 19, 138–149 (2015).
Wu, Y. M., Lin, K. L. & Chen, R. F. Research the intervention with Baduanjin exercise and healthy education to the 175 plasma glucose of diabetes mellitus subhealthy state. Chin Primary Health Care. 22, 80–82 (2008).
Xiong, X., Wang, P., Li, S., Zhang, Y. & Li, X. Effect of Baduanjin exercise for hypertension: a systematic review and meta-analysis of randomized controlled trials. Maturitas. 80, 370–8 (2015).
Mei, L., Chen, Q., Ge, L., Zheng, G. & Chen, J. Systematic review of chinese traditional exercise baduanjin modulating the blood lipid metabolism. Evid Based Complement Alternat Med. 2012, 282131, https://doi.org/10.1155/2012/282131 (2012).
Zheng, G. et al. Primary prevention for risk factors of ischemic stroke with Baduanjin exercise intervention in the community elder population: study protocol for a randomized controlled trial. Trials. 15, 113, doi: 10.1186 (2014).
Wang, L. D. Screening of subjects at high risk for stroke [M]. Beijing: Screening and Prevention Program of Stroke Organized by Ministry of Public Health Press. 2–4 (2012).
Health Qigong Management Center of General Administration of Sport of China: Health Qigong-Baduanjin. Beijing: People’s Sports Publishing House of China (2003).
Niehaus, L., Lehmann, R., Röricht, S. & Meyer, B. U. Age-related reduction in visually evoked cerebral blood flow responses. Neurobiol Aging. 22, 35–8 (2001).
Ainslie, P. N. et al. Elevation ctivity prevents age-related impai with aerobic fitness throughout healthy human ageing. J Physiol. 586, 4005–4010 (2008).
Taddei, S. et al. Physical activity prevents age-related impairment in nitric oxide availability in elderly athletes. Circulation. 101, 2896–901 (2000).
Ainslie, P. N. et al. Elevation in cerebral blood flow velocity with aerobic fitness throughout healthy human ageing. J Physiol. 586, 4005–10 (2008).
Wang, Y., Li, M., Dong, F., Zhang, J. & Zhang, F. Physical exercise-induced protection on ischemic cardiovascular and cerebrovascular diseases. Int J Clin Exp Med. 8, 19859–66 (2015).
Nagata, K. et al. Cerebral circulation in aging. Ageing research review. 30, 49–60 (2016).
Querido, J. S. & Sheel, A. W. Regulation of cerebral blood flow during exercise. Sports Med. 37, 765–782 (2007).
Bailey, D. M. et al. Elevated aerobic fitness sustained throughout the adult lifespan is associated with improved cerebral hemodynamics. Stroke. 44, 3235–8 (2013).
Zheng, G. et al. The effect of Baduanjin exercise for physical and psychological wellbeing of college students: study protocol for a randomized controlled trial. Trials. 14, 422, https://doi.org/10.1186/1745-6215-14-422 (2013).
Kodama, S. et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 301, 2024–35 (2009).
Mahdiabadi, J., Gaeini, A. A., Kazemi, T. & Mahdiabadi, M. A. The effect of aerobic continuous and interval training on left ventricular structure and function in male non-athletes. Biol Sport. 30, 207–11 (2013).
Spruit, M. A. et al. COPD and exercise: does it make a difference? Breathe (Sheff). 12, e38–49 (2016).
Platt, C., Houstis, N. & Rosenzweig, A. Using exercise to measure and modify cardiac function. Cell Metab. 21, 227–36 (2015).
Li, R. et al. The effect of baduanjin on promoting the physical fitness and health of adults. Evid Based Complement Alternat Med. 2014, 784059 (2014).
Serrador, J. M., Picot, P. A., Rutt, B. K., Shoemaker, J. K. & Bondar, R. L. MRI measures of middle cerebral artery diameter in conscious humans during simulated orthostasis. Stroke. 31, 1672–1678 (2000).
Acknowledgements
We thank the participants and staff at the communities and hospitals for their work in this project, including the Fujian University of Traditional Chinese Medicine Subsidiary Rehabilitation Hospital and the Health Check Center of the Second People’s Hospital of Fujian Province. This study was supported by the Programme for Fostering Middle-Aged and Young Key Talent at Fujian Provincial Health and Family Planning Commission (2014-ZQN-ZD-27) and the Collaboration Innovation Center for Rehabilitation Technology (X2012002-Xietong).
Author information
Authors and Affiliations
Contributions
C.L.D. and Z.G.H. conceived and designed the study protocol. Z.G.H. wrote the manuscript. T.J. was in charge of coordination and direct implementation. C.B. and F.Q.Y. managed the training location and the follow-up. L.Q. instructed the participants in Baduanjin training. All authors contributed to drafting the manuscript and have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zheng, G., Chen, B., Fang, Q. et al. Baduanjin exercise intervention for community adults at risk of ischamic stroke: A randomized controlled trial. Sci Rep 9, 1240 (2019). https://doi.org/10.1038/s41598-018-37544-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-37544-0
This article is cited by
-
Effects of Baduanjin exercise on the physical function of middle-aged and elderly people: a systematic review and meta-analysis of randomized controlled trials
BMC Complementary Medicine and Therapies (2023)
-
Benefits of Community-Based Approaches in Assessing and Addressing Sleep Health and Sleep-Related Cardiovascular Disease Risk: a Precision and Personalized Population Health Approach
Current Hypertension Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.