Abstract
Helicobacter pylori (H. pylori) is the causative agent of gastric cancer, making it the only bacterium to be recognized as a Class I carcinogen by the World Health Organization. The virulence factor cytotoxin associated gene A (CagA) is a known oncoprotein that contributes to the development of gastric cancer. The other major virulence factor vacuolating cytotoxin A (VacA), disrupts endolysosomal vesicular trafficking and impairs the autophagy pathway. Studies indicate that there is a functional interplay between these virulence factors by unknown mechanisms. We show that in the absence of VacA, both host-cell autophagy and the proteasome degrade CagA during infection with H. pylori. In the presence of VacA, CagA accumulates in gastric epithelial cells. However, VacA does not affect proteasome function during infection with H. pylori suggesting that VacA−disrupted autophagy is the predominant means by which CagA accumulates. Our studies support a model where in the presence of VacA, CagA accumulates in dysfunctional autophagosomes providing a possible explanation for the functional interplay of VacA and CagA.
Similar content being viewed by others
Introduction
Helicobacter pylori (H. pylori) is a gram-negative bacterium that colonizes the gastric mucosa in over 50% of the population worldwide causing gastritis in all infected individuals, peptic ulcers in 10–20% and gastric cancer in 1–2% of those infected1,2. The World Health Organization has classified H. pylori as a Class I carcinogen for gastric cancer development3. Gastric cancer accounts for approximately 754,000 deaths per year and is the 4th leading cause of cancer-related deaths worldwide4. The presence of two main virulence factors, the cytotoxin associated gene A (CagA) and the vacuolating cytotoxin A (VacA), are associated with an increased risk of developing gastric cancer5,6.
CagA is a 120–145 kDa oncoprotein injected into host cells by a type IV secretion system7. Once internalized, CagA is tethered to the inner leaflet of the plasma membrane where it can be phosphorylated on tyrosine residues in EPIYA motifs by Src and Abl kinases8. The oncogenic capability of CagA has been directly demonstrated through the use of transgenic mice and zebrafish models that developed gastrointestinal tumors9,10. Further increasing our understanding of the regulation of CagA during host-pathogen interactions should advance the development of novel preventative and therapeutic approaches to combat carcinogenesis.
Cellular proteins are targeted for degradation by the ubiquitin-proteasome system or the autophagy pathway11. Tsugawa et al. have demonstrated that CagA is degraded by autophagy12. Importantly, work from our laboratory and others has shown that VacA can modulate the autophagy pathway13,14,15,16.
VacA is a secreted pore-forming cytotoxin that upon acute exposure stimulates the autophagy pathway in cells12,13,14. However, upon prolonged exposure, VacA disrupts lysosomal trafficking, resulting in the accumulation of dysfunctional autophagosomes that lack cathepsin D and the formation of large intracellular vacuoles that promote the intracellular survival of H. pylori15. All strains of H. pylori harbor the vacA gene, suggesting that VacA plays a crucial role in the colonization and persistence of H. pylori within the gastric mucosa17. Previous studies have demonstrated antagonistic interactions between VacA and CagA18,19,20. This antagonism is evident morphologically where isogenic cagA mutant strains induced greater vacuolation, while isogenic vacA mutant strains have more pronounced hummingbird phenotype, a hallmark of CagA intoxication, compared to wild-type strains21. In fact, CagA has been shown to reduce the entry of VacA into host cells22. Although the exact mechanisms underlying the functional antagonism between the two virulence factors remains unclear, studies have shown that effects on various intracellular pathways, including NFAT, apoptosis, and MAP kinase have been proposed to play a role18,19,20.
Emerging evidence in the past decade has demonstrated considerable “cross-talk” between the ubiquitin-proteasome system and the autophagy pathway23. During proteasome inhibition/dysfunction, autophagy can serve as a compensatory mechanism to clear ubiquitinated substrates24,25. Conversely, autophagy inhibition/dysfunction is not compensated by enhanced proteasome activation26,27. In fact, prolonged disruption of autophagy has been shown to hinder proteasome degradation and leads to an accumulation of proteasome substrates28. Therefore, we determined the role of autophagy and the proteasome in the regulation of CagA levels. Furthermore, since VacA results in accumulation of disrupted autophagosomes, we characterized the impact of VacA on autophagy, the proteasome and CagA levels.
Results
Both autophagy and the proteasome regulate intracellular CagA
Cellular proteins can be degraded by autophagy or selectively targeted for degradation by the ubiquitin-proteasome system11. Therefore, we assessed the role of autophagy in regulating CagA by infecting autophagy-deficient cells with H. pylori. To eliminate any effects of VacA, which we have shown disrupts autophagosome maturation15, we infected autophagy-deficient (Atg5−/−) Mouse Embryonic Fibroblasts (MEFs) with a CagA+ vacA- isogenic mutant strain of H. pylori for 8 hours using a gentamycin protection assay and measured intracellular CagA levels by Western Blot. An increase in CagA was detected in infected Atg5−/− MEFs in comparison to wild-type (WT) cells (Fig. 1A). Parallel viability assays were performed to quantify the number of intracellular bacteria and determine if the observed increase in CagA could be due to an increase in bacterial survival. We normalized the levels of CagA to the level of intracellular bacteria as determined by colony forming units (CFU). After controlling for intracellular survival, the increase in CagA levels in Atg5−/− MEFs persisted (Fig. S1A). To further validate our findings, we used siRNA to knockdown Atg12 in gastric epithelial (AGS) cells and infected cells with a CagA+ vacA− isogenic mutant strain of H. pylori (Fig. S2A). Similar to the findings with the Atg5−/− MEFs, an increase in CagA was detected in AGS cells with siRNA knockdown of Atg12, in comparison with control cells.
Autophagy and the proteasome regulate CagA stability. (A) Wild-type (WT) and autophagy-deficient (Atg5−/−) MEFs were infected with a CagA+ vacA− isogenic mutant strain (MOI 100) for 8 hours using a gentamycin protection assay. The autophagy marker LC3-II was used to confirm that Atg5−/− MEFs are autophagy-deficient. CagA protein levels were measured by Western blotting using β-actin as loading control. Graph shows fold change of CagA normalized to β-actin relative to WT MEFs (mean + SEM; n = 4). (B) AGS cells were infected with a CagA+ vacA− isogenic mutant strain (MOI 50) for 19 hours using a gentamycin protection assay. MG132 (5 μM) was added during the 14-hour low-dose gentamycin incubation. DMSO was used as a vehicle control. CagA protein levels were measured by Western blotting using β-actin as loading control. Graph shows fold change of CagA normalized to β-actin relative to vehicle control (mean + SEM; n = 6). (C) AGS cells were infected with a CagA+ vacA− isogenic mutant strain (MOI 50) for 24 hours using a gentamycin protection assay. Lactacystin (10 μM) was added during the 19-hour low-dose gentamycin incubation. Water was used as a vehicle control. CagA protein levels were measured by Western blotting using β-actin as loading control. Graph shows fold change of CagA normalized to β-actin relative to vehicle control (mean + SEM; n = 5). Relevant gel bands were cropped from the original blots. Dotted line indicates slicing of two regions together from the same blot. Statistical analysis was performed using Student’s t-test.
To determine if the proteasome could also regulate CagA levels, we treated AGS cells with proteasome inhibitors and measured intracellular CagA levels. AGS cells infected with a CagA+ vacA− isogenic mutant strain of H. pylori and treated with the proteasome inhibitor MG132 demonstrated an increase in CagA compared to vehicle control (Fig. 1B). We confirmed these findings using a different proteasome inhibitor, lactacystin, which showed a similar increase in CagA levels (Fig. 1C). We performed parallel viability assays to determine if the proteasome influenced intracellular bacterial survival. There was no significant difference in the number of intracellular bacteria in cells treated with proteasome inhibitors compared to control (Fig. S1B-C). These results indicate that intracellular CagA levels are regulated by both autophagy and the proteasome.
VacA promotes CagA accumulation during H. pylori infection
Since VacA disrupts both autophagy and lysosomal degradation within the cell15, we further investigated whether VacA can alter intracellular CagA levels during H. pylori infection. AGS cells were infected with a CagA+ vacA− isogenic mutant strain of H. pylori and co-cultured with or without conditioned culture media supernatant (CCMS) obtained from the wild-type VacA+ strain or the vacA− isogenic mutant strain of H. pylori for up to 24 hours. We confirmed that VacA disrupts autophagic degradation by assessing LC3-II and p62 accumulation (Fig. S3A-B). Following a gentamycin protection assay, cell lysates were tested for intracellular CagA levels. Incubation with VacA+ CCMS significantly increased CagA levels compared to untreated or VacA− CCMS treated cells infected with H. pylori for 24 hours (Fig. 2A). We have shown previously that VacA promotes intracellular survival of H. pylori during chronic infection13. Therefore, to determine if the observed increase in CagA in the presence of VacA could be due to an increase in bacterial survival, we normalized the levels of CagA to the level of intracellular bacteria as determined by CFUs (Fig. 2B). After controlling for intracellular survival, the increase in CagA levels in the presence of VacA persisted. This data suggests that VacA promotes an accumulation of CagA, independent of bacterial survival. We next attempted to assess the subcellular localization of CagA in the presence of VacA+ or VacA− CCMS using AGS cells transfected with CagA-GFP. In control cells, CagA was mainly localized to the cell membrane as expected. In transfected cells treated with either VacA+ or VacA− CCMS, CagA-GFP was redistributed to puncta within the cell (Fig. S2B). There appeared to be an increase in co-localization of the GFP puncta with LC3 in VacA+ CCMS-treated cells in comparison with VacA− CCMS-treated cells.
VacA promotes CagA accumulation. (A) AGS cells were infected with a CagA+ vacA− isogenic mutant strain and co-cultured in the presence or absence of VacA− or VacA + CCMS for 24 hours using a gentamycin protection assay to assess CagA levels. NT denotes infection with a CagA+ vacA− isogenic mutant strain alone and (-) denotes uninfected control cells. CagA protein levels were measured by Western blotting using β-actin as loading control. Relevant gel bands were cropped from the original blots. Graph shows fold change of CagA normalized to β-actin relative to NT (mean + SEM; n = 5). (B) Bacterial viability assays were performed in parallel to calculate colony forming units (CFU). Graph shows the average CFU relative to NT (mean + SEM; n = 5). (C) Graph shows CagA protein level normalized to β-actin and CFU from each corresponding experiment (mean + SEM; n = 5). Statistical analysis was performed using ANOVA with Tukey’s post-hoc test.
Effect of VacA on the proteasome
Since dysregulation of autophagy has been shown to impair proteasome degradation26,27,28, we next determined if VacA, which disrupts autophagosome maturation, could alter proteasome function. We first explored whether VacA impairs proteasomal degradation by quantifying the total amount of ubiquitinated proteins during H. pylori infection in AGS cells treated with VacA+ or VacA− CCMS. There was a significant increase in the amount of ubiquitinated proteins in cells treated with MG132 (Fig. 3A). In contrast, we did not observe a significant change in ubiquitinated proteins in VacA+ treated cells in comparison with VacA− treated cells, suggesting that VacA does not alter proteasome function. To directly assess the effects of VacA on the proteasome, we used the ubiquitin-proteasome pathway activity reporter UbG76V-GFP, which is degraded by the proteasome and rapidly accumulates if proteasome degradation is impaired29. We employed HeLa cells stably expressing the UbG76V-GFP reporter to compare levels of UbG76V-GFP in cells treated cells with VacA+ or VacA− CCMS. We confirmed that VacA impairs autophagic degradation in these Hela cells (Fig. S3C-D). As shown in Fig. 3B, there was minimal UbG76V-GFP detected in cells treated with VacA− CCMS. Similarly, VacA+ CCMS treatment did not result in increased UbG76V-GFP. As expected, an increase in UbG76V-GFP was detected in cells treated with MG132 or lactacystin. Taken together these findings suggest that VacA does not impact proteasome function.
VacA disrupts autophagy but does not impair proteasome degradation. (A) AGS cells were infected with a CagA+ vacA isogenic mutant strain and co-cultured in the presence or absence of VacA− or VacA+ CCMS for 19 hours using a gentamycin protection assay. MG132 (5 μM) was added during the 14-hour low-dose gentamycin incubation. DMSO was used as a vehicle control. Ubiquitin protein levels were measured by Western blotting using β-actin as loading control. Graph shows fold change of ubiquitin normalized to β-actin relative to vehicle control (mean + SEM; n = 5). (B) UbG76V-GFP HeLa cells were treated with 10 μM of MG132 or Lactacystin for 4 and 8 hours respectively, or VacA+ or VacA− CCMS for 32 hours. UbG76V-GFP protein levels were measured by Western blotting using β-actin as loading control (mean + SEM; n = 3). Relevant gel bands were cropped from the original blots. Dotted line indicates slicing of two regions together from the same blot. Statistical analysis was performed using Student’s t-test.
In contrast to complete inhibition of autophagosome formation seen in Atg5−/− MEFs, VacA disrupts autophagosome maturation, resulting in the accumulation of dysfunctional autophagosomes. We examined the effect of proteasome inhibition in the presence of VacA. As shown in Fig. 4A–C, in the absence of VacA, proteasome inhibition promotes accumulation of CagA. However, in the presence of VacA, proteasome inhibition does not result in further increases in CagA (Fig. 4C). These findings suggest that in the presence of VacA, the functional proteasomes are not able to target CagA for degradation.
Proteasome degradation of CagA is influenced by VacA. AGS cells were infected with a CagA+ vacA− isogenic mutant strain in the presence of VacA− or VacA+ CCMS for (A) 19 hours or (B) 24 hours using a gentamycin protection assay and incubated with (A) MG132 (5 μM) or (B) Lactacystin (10 μM) during the 14-hour or 19-hour low-dose gentamycin incubation, respectively. DMSO and water was used as a vehicle control. CagA protein levels were measured by Western blotting using β-actin as loading control. Relevant gel bands were cropped from the original blots. (C) Graph shows fold change of CagA normalized to β-actin relative to vehicle control in cells treated with MG132 or Lactacystin (mean + SEM; n = 6). Statistical analysis was performed using Student’s t-test (*p < 0.05, **p < 0.01, ns = not significant).
Effects of VacA on phosphorylated CagA
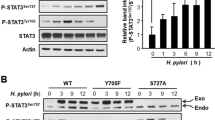
CagA alters specific host cell signaling pathways in both a tyrosine phosphorylation dependent and independent manner30,31,32,33,34,35,36. Furthermore, only intracellular CagA can be tyrosine phosphorylated by host cell kinases, therefore changes in phosphorylated CagA specifically reflect changes in intracellular CagA. We next determined how VacA affects the levels of tyrosine phosphorylated CagA during H. pylori infection (Fig. 5). AGS cells treated with VacA+ CCMS had a significant increase in phosphorylated CagA (Fig. 5A). Next, to confirm that these changes were specific for VacA, we treated cells with purified VacA toxin. As shown in Fig. 5B, VacA is necessary and sufficient to promote CagA and phosphorylated CagA accumulation in AGS cells infected with a CagA+ vacA− isogenic mutant strain of H. pylori.
VacA promotes the accumulation of phosphorylated CagA. AGS cells were infected with a CagA+ vacA− isogenic mutant strain in the presence of (A) VacA− or VacA+ CCMS and (B) untreated or treated with purified VacA toxin for 20 hours using a gentamycin protection assay. Phosphorylated CagA (pTyr) and total CagA levels were measured by Western blotting using β-actin as a loading control. (C) AGS cells were infected with a CagA+ vacA− isogenic mutant strain in the presence of VacA− or VacA+ CCMS for 19 hours using a gentamycin protection assay and incubated with DMSO or MG132 (5 μM). Phosphorylated CagA levels were measured by Western blotting using β-actin as loading control. Graphs show fold change of pTyr or CagA normalized to β-actin (mean + SEM; n = 3). Statistical analysis was performed using Student’s t-test.
Next, we assessed the effect of proteasome inhibition on phosphorylated CagA in the presence or absence of VacA. As shown in Fig. 5C, there was a significant increase in the amount of phosphorylated CagA in VacA− CCMS treated cells in the presence of MG132, suggesting that the proteasome targets both phosphorylated and non-phosphorylated CagA for degradation. Addition of the proteasome inhibitor to VacA+ CCMS treated cells did not result in a further increase in phosphorylated CagA levels, which is consistent with the findings assessing total CagA levels under the same conditions.
Discussion
H. pylori is one of the most successful human pathogens due to its ability to avoid degradation and maintain a chronic infective state without killing its host. This success is mediated in part by the interplay of two key virulence factors, CagA and VacA. In this study, we show that in addition to degradation by the autophagy pathway, CagA is degraded by the proteasome. Furthermore, in the presence of VacA there is an accumulation of both total and phosphorylated CagA. However, VacA does not affect the proteasome suggesting that in the presence of VacA, oncogenic CagA accumulation is likely mediated by VacA−disrupted autophagy thereby demonstrating a complex interplay between CagA and VacA.
Previous studies have shown that CagA is a relatively short-lived protein that is rapidly degraded37 and that this degradation is mediated by autophagy as shown by the use of autophagy inhibitors12. We validated these results using Atg5−/− MEFs and Atg12 siRNA knockdown of AGS cells to show that CagA is degraded by autophagy. Parallel viability assays demonstrate that the accumulation in CagA in Atg5−/− MEFs was not due to increased bacterial survival. These findings are consistent with those of Tsugawa et al. who demonstrated that CagA specifically accumulates in CD44v9-expressing cancer stem-like cells which have suppressed autophagy12. In contrast to their study, which found that VacA exposure increased degradation of CagA, we found that VacA−disrupted autophagy promotes an accumulation of CagA. We had previously shown that acute exposure to VacA enhances autophagy while prolonged exposure to VacA disrupts autophagy14,15. We suggest that differences in methodology may explain this apparent discrepancy. Of interest, a recent study by Li et al., demonstrated that CagA could inhibit autophagy38. We did not assess the effect of CagA on autophagy in the present study.
In addition to autophagic degradation of CagA, our results show for the first time that the proteasome is also involved in the regulation of CagA. We found that in the presence of VacA, the degradation of CagA mediated by the proteasome is prevented. Since VacA does not impair proteasome function, we propose that CagA may accumulate in defective autophagosomes, where it is inaccessible to the proteasome. We attempted to determine the subcellular location of CagA in the presence of VacA by using cells transfected with CagA-GFP. We found that culture supernatants from both VacA+ and VacA− H. pylori caused a redistribution of CagA from the cell membrane to puncta within the cell. In addition, in cells treated with VacA+ CCMS, there appeared to be more colocalization with LC3+ puncta indicative of autophagosomes. However, this data should be interpreted with caution as transfection of CagA may not accurately reflect delivery of CagA during infection. Thus, additional studies will be required to delineate the specific subcellular location of CagA in the presence of VacA during H. pylori infection.
In summary, our studies support a model whereby VacA-mediated disruption of autophagy promotes CagA accumulation in cells. We suggest that CagA may accumulate in dysfunctional autophagosomes that remain inaccessible to the proteasome and limit potential downstream signaling of CagA. Thus, we provide a potential mechanism explaining the functional antagonism of CagA in the presence of VacA.
Materials and Methods
Antibodies
The following antibodies were used for Western blotting: anti-β-actin (A4700; 1:5000; Sigma-Aldrich, Oakville, Canada), anti-LC3B (NB600-1384; 1:1000 for WB; 1:200 for IF; Novus Biologicals; Oakville, Canada), anti-p62 (610832; 1:1000; BD Transduction; Mississauga, Canada), anti-pTyr (4G10; 1:500; EMD Millipore, Etobicoke, Canada), anti-CagA (b-300; 1:500; Santa Cruz, Dallas, TX), anti-Ubiquitin (P4D1; 1:500; Santa Cruz, Dallas, TX), anti-Atg12 (2010; 1:500; Cell Signaling, Whitby, Canada) goat anti-mouse IgG (115-035-003; 1:2500; Jackson ImmunoResearch, West Grove, PA), and goat anti-rabbit IgG (115-035-144; 1:2500; Jackson ImmunoResearch, West Grove, PA).
Pharmacological inhibitors
MG132 (5 μM; Sigma-Aldrich, Oakville, Canada) was dissolved in DMSO and Lactacystin (10 μM; Enzo Life Sciences, Farmingdale, NY) was dissolved in milli-Q water. Cells were incubated with MG132 for 14 hours or Lactacystin for 19 hours during the low-dose gentamycin treatment in order to inhibit the 20 S proteasome subunit. Control cells were treated with DMSO or milli-Q water, respectively.
Bacterial culture and growth conditions
Helicobacter pylori strain 60190 was purchased from American Type Culture Collection (49503, cagA+ , cagE+ , vacA+ ; Rockville, MD). Isogenic vacA and cagA mutants were provided by Dr. Richard Peek (Vanderbilt University School of Medicine, Nashville, TN) and were constructed as described39,40. H. pylori was grown on Columbia agar plates supplemented with 5% sheep blood (Oxoid Microbiology Products, Thermo Scientific, Napean, Canada) for 48–72 hours at 37 °C in microaerophilic conditions (5% oxygen, 10% carbon dioxide). H. pylori was then transferred to Brucella broth (Sigma-Aldrich, Oakville, Canada) supplemented with heat-inactivated Fetal Bovine Serum (FBS; Wisent, St. Bruno, Canada) and grown for 18–24 hours at 37 °C in microaerophilic conditions. H. pylori was then assessed by observing helical morphology as well as viability through active mobility using a light microscope. The concentration of bacteria was determined by measuring the optical density at 600 nm (OD 600), where 1 OD is equivalent to 2 × 108 bacteria/mL.
Preparation of H. pylori culture supernatants and purified VacA toxin
For cell treatment with VacA toxin, wild-type and vacA isogenic mutant H. pylori culture supernatants (OD = 1.0) were filtered through a 0.22-μm-cutoff membrane filter and concentrated 10 times using a 30-kDa-cutoff Amicon Ultra centrifugal filter (Millipore, Billerica, MA). VacA CCMS was utilized at 10% of the final concentration. Purified VacA toxin (kindly provided by Dr. Steven Blanke) was diluted 1:100 and activated by incubation in acidified Ham’s F-12K culture media, pH 2, for 30 minutes at 37 °C. The media was then neutralized to pH 7 and supplemented with 10% FBS. For cell intoxication, AGS cells were incubated in the presence of activated purified VacA toxin (35 nM) for 20 hours.
Cell culture
AGS cells were purchased from American Type Culture Collection (Rockville, MD). AGS cells were grown in Ham’s F-12K media supplemented with 10% heat-inactivated FBS (Wisent, St. Bruno, Canada) and grown at 37 °C in a humidified chamber (5% CO2). Wild-type and Atg5 deficient (Atg5−/−) mouse embryonic fibroblasts (MEFs) were kindly provided by Dr. John Brumell (The Hospital for Sick Children, Toronto, Canada) and grown in Dulbecco’s Modified Eagle’s Media (DMEM; Wiscent, St. Bruno, Canada) supplemented with 10% FBS. HeLa cells stably expressing the UbG76V-GFP reporter was kindly provided by Dr. Nico Dantuma (Karolinksa Institutet, Stockholm, Sweden) and grown in DMEM containing 10% FBS, 0.5 mg/mL G418 (Sigma-Aldrich, Oakville, Canada), 2 mM L-glutamine, and 1% penicillin-streptomycin.
Cell invasion and intoxication assays
For H. pylori infection, bacteria were centrifuged at 2,500 g for 5 minutes and resuspended in the appropriate cell culture media. Cell invasion was performed at a multiplicity of infection (MOI) of 50 on 70–90% confluent cells AGS cells, and an MOI of 100 on 70–90% confluent MEFs. Infected AGS cells were co-cultured with or without VacA− or VacA+ CCMS. For the gentamycin protection assays, cells were infected for 4 hours and then washed 3 times with PBS to remove non-adhered bacteria. Cells were then incubated in cell culture media containing 100 μg/mL gentamycin (Wisent, St. Bruno, Canada) for 1 hour to kill non-internalized bacteria, after which gentamycin was reduced to 10 μg/mL to prevent the growth of extracellular bacteria. VacA− or VacA+ CCMS along with pharmacological inhibitors were co-cultured with the 10 μg/mL of gentamycin for the remaining duration of the experiment.
Viability Assays
Experiments were performed in duplicate; one set was used to prepare lysates for Western blotting and the other to measure bacterial viability. Bacterial viability assays were carried out as previously described41. Briefly, at the end of the invasion assays, cells were washed 3 times with PBS and lysed in a 1% saponin (Sigma-Aldrich Oakville, Canada) solution prepared in serum-free cell culture media for 8–10 minutes. Serial dilutions were prepared in serum-free cell culture media and 50 μL of each dilution was pipetted onto Columbia agar plates supplemented with 5% sheep blood in triplicate. Plates were placed at 37 °C in microaerophilic conditions for 72–96 hours before enumerating colony forming units (CFU). The average CFU value from triplicate plates was used for statistical analysis.
Immunoblotting
Cells were lysed, as previously described42, and separated using SDS-PAGE followed by transfer to nitrocellulose membranes (Pall Corporation, Port Washington, NY). Membranes were probed at 4 °C overnight with the appropriate primary antibodies followed by incubation with the corresponding horseradish peroxidase-conjugated secondary antibodies for 1 hour at room temperature. Bands were visualized by chemiluminescence (Western blotting luminol reagent; Santa Cruz, Dallas, TX) using Licor Odyssey Fc imaging system.
Statistics
Densitometry analysis was performed using Image Studio software (Licor, Lincoln, NE). Densities of proteins bands were measured and expressed as a ratio of protein of interest over the loading control (i.e. CagA/Actin). For graphical representation, the ratio of each treatment was expressed as the fold-change relative to the control. Statistical significance between treatment groups was calculated using GraphPad Prism 6.0c (GraphPad Inc., La Jolla, CA). P values less than 0.05 were deemed statistically significant.
Data Availability
All data and constructs are available upon request.
References
Hooi, J. K. Y. et al. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology 153, 420–429 (2017).
Kusters, J. G., van Vliet, A. H. M. & Kuipers, E. J. Pathogenesis of Helicobacter pylori infection. Clin Microbiol Rev 19, 449–490 (2006).
Polk, D. B. & Peek, R. M. Helicobacter pylori: gastric cancer and beyond. Nat Rev Cancer 10, 403–414 (2010).
Plummer, M. et al. Global burden of cancers attributable to infections in 2012: a synthetic analysis. Lancet Glob. Heal. 4, e609–e616 (2016).
Huang, J. Q., Zheng, G. F., Sumanac, K., Irvine, E. J. & Hunt, R. H. Meta-analysis of the relationship between cagA seropositivity and gastric cancer. Gastroenterology 125, 1636–1644 (2003).
Matos, J. I., de Sousa, H. A. C., Marcos-Pinto, R. & Dinis-Ribeiro, M. Helicobacter pylori CagA and VacA genotypes and gastric phenotype: a meta-analysis. Eur J Gastroenterol Hepatol 25, 1431–1441 (2013).
Censini, S. et al. cag, a pathogenicity island of Helicobacter pylori, encodes type I-specific and disease-associated virulence factors. Proc Natl Acad Sci USA 93, 14648–14653 (1996).
Murata-Kamiya, N., Kikuchi, K., Hayashi, T., Higashi, H. & Hatakeyama, M. Helicobacter pylori exploits host membrane phosphatidylserine for delivery, localization, and pathophysiological action of the CagA oncoprotein. Cell Host Microbe 7, 399–411 (2010).
Ohnishi, N. et al. Transgenic expression of Helicobacter pylori CagA induces gastrointestinal and hematopoietic neoplasms in mouse. Proc Natl Acad Sci USA 105, 1003–1008 (2008).
Neal, J. T., Peterson, T. S., Kent, M. L. & Guillemin, K. H. pylori virulence factor CagA increases intestinal cell proliferation by Wnt pathway activation in a transgenic zebrafish model. Dis. Model. Mech. 6, 802–810 (2013).
Clague, M. J. & Urbé, S. Ubiquitin: same molecule, different degradation pathways. Cell 143, 682–685 (2010).
Tsugawa, H. et al. Reactive oxygen species-induced autophagic degradation of Helicobacter pylori CagA is specifically suppressed in cancer stem-like cells. Cell Host Microbe 12, 764–777 (2012).
Terebiznik, M. R. et al. Helicobacter pylori VacA toxin promotes bacterial intracellular survival in gastric epithelial cells. Infect Immun 74, 6599–6614 (2006).
Terebiznik, M. R. et al. Effect of Helicobacter pylori’s vacuolating cytotoxin on the autophagy pathway in gastric epithelial cells. Autophagy 5, 370–379 (2009).
Raju, D. et al. Vacuolating cytotoxin and variants in Atg16L1 that disrupt autophagy promote Helicobacter pylori infection in humans. Gastroenterology 142, 1160–1171 (2012).
Zhu, P. et al. Helicobacter pylori VacA induces autophagic cell death in gastric epithelial cells via the endoplasmic reticulum stress pathway. Cell Death Dis. 8, 3207 (2017).
Cover, T. L. & Blanke, S. R. Helicobacter pylori VacA, a paradigm for toxin multifunctionality. Nat Rev Microbiol 3, 320–332 (2005).
Yokoyama, K. et al. Functional antagonism between Helicobacter pylori CagA and vacuolating toxin VacA in control of the NFAT signaling pathway in gastric epithelial cells. Proc Natl Acad Sci USA 102, 9661–9666 (2005).
Oldani, A. et al. Helicobacter pylori counteracts the apoptotic action of its VacA toxin by injecting the CagA protein into gastric epithelial cells. PLoS Pathog 5, e1000603 (2009).
Tegtmeyer, N. et al. Importance of EGF receptor, HER2/Neu and Erk1/2 kinase signalling for host cell elongation and scattering induced by the Helicobacter pylori CagA protein: antagonistic effects of the vacuolating cytotoxin VacA. Cell Microbiol 11, 488–505 (2009).
Argent, R. H. et al. Functional association between the Helicobacter pylori virulence factors VacA and CagA. J Med Microbiol 57, 145–150 (2008).
Akada, J. K. et al. Helicobacter pylori CagA inhibits endocytosis of cytotoxin VacA in host cells. Dis Model Mech 3, 605–617 (2010).
Korolchuk, V. I., Menzies, F. M. & Rubinsztein, D. C. Mechanisms of cross-talk between the ubiquitin-proteasome and autophagy-lysosome systems. FEBS Lett 584, 1393–1398 (2010).
Rideout, H. J., Lang-Rollin, I. & Stefanis, L. Involvement of macroautophagy in the dissolution of neuronal inclusions. Int J Biochem Cell Biol 36, 2551–2562 (2004).
Pandey, U. B. et al. HDAC6 rescues neurodegeneration and provides an essential link between autophagy and the UPS. Nature 447, 859–863 (2007).
Komatsu, M. et al. Loss of autophagy in the central nervous system causes neurodegeneration in mice. Nature 441, 880–884 (2006).
Hara, T. et al. Suppression of basal autophagy in neural cells causes neurodegenerative disease in mice. Nature 441, 885–889 (2006).
Korolchuk, V. I., Mansilla, A., Menzies, F. M. & Rubinsztein, D. C. Autophagy inhibition compromises degradation of ubiquitin-proteasome pathway substrates. Mol Cell 33, 517–527 (2009).
Dantuma, N. P., Lindsten, K., Glas, R., Jellne, M. & Masucci, M. G. Short-lived green fluorescent proteins for quantifying ubiquitin/proteasome-dependent proteolysis in living cells. Nat Biotechnol 18, 538–543 (2000).
Suzuki, M. et al. Interaction of CagA with Crk plays an important role in Helicobacter pylori-induced loss of gastric epithelial cell adhesion. J Exp Med 202, 1235–1247 (2005).
Tammer, I., Brandt, S., Hartig, R., König, W. & Backert, S. Activation of Abl by Helicobacter pylori: a novel kinase for CagA and crucial mediator of host cell scattering. Gastroenterology 132, 1309–1319 (2007).
Higashi, H. et al. SHP-2 tyrosine phosphatase as an intracellular target of Helicobacter pylori CagA protein. Science (80-.). 295, 683–686 (2002).
Higashi, H. et al. Helicobacter pylori CagA induces Ras-independent morphogenetic response through SHP-2 recruitment and activation. J Biol Chem 279, 17205–17216 (2004).
Tsutsumi, R., Takahashi, A., Azuma, T., Higashi, H. & Hatakeyama, M. Focal adhesion kinase is a substrate and downstream effector of SHP-2 complexed with Helicobacter pylori CagA. Mol Cell Biol 26, 261–276 (2006).
Buti, L. et al. Helicobacter pylori cytotoxin-associated gene A (CagA) subverts the apoptosis-stimulating protein of p53 (ASPP2) tumor suppressor pathway of the host. Proc Natl Acad Sci USA 108, 9238–9243 (2011).
Murata-Kamiya, N. et al. Helicobacter pylori CagA interacts with E-cadherin and deregulates the beta-catenin signal that promotes intestinal transdifferentiation in gastric epithelial cells. Oncogene 26, 4617–4626 (2007).
Ishikawa, S., Ohta, T. & Hatakeyama, M. Stability of Helicobacter pylori CagA oncoprotein in human gastric epithelial cells. FEBS Lett 583, 2414–2418 (2009).
Li, N. et al. Helicobacter pylori CagA Protein Negatively Regulates Autophagy and Promotes Inflammatory Response via c-Met-PI3K/Akt-mTOR Signaling Pathway. Front. Cell. Infect. Microbiol. 7, 417 (2017).
Peek, R. M. et al. Helicobacter pylori strain-specific genotypes and modulation of the gastric epithelial cell cycle. Cancer Res 59, 6124–6131 (1999).
Tummuru, M. K., Cover, T. L. & Blaser, M. J. Mutation of the cytotoxin-associated cagA gene does not affect the vacuolating cytotoxin activity of Helicobacter pylori. Infect. Immun. 62, 2609–2613 (1994).
Raju, D., Rizzuti, D. & Jones, N. L. Cell culture-based assays to test for bacterial adherence and internalization. Methods Mol Biol 921, 69–76 (2012).
Rizzuti, D. et al. Helicobacter pylori inhibits dendritic cell maturation via interleukin-10-mediated activation of the signal transducer and activator of transcription 3 pathway. J. Innate Immun. 7, 199–211 (2015).
Acknowledgements
This research was funded by the Canadian Institutes of Health Research (CIHR MOP-341293).
Author information
Authors and Affiliations
Contributions
M.A., D.B., M.I.C. and D.R. performed the experiments. D.B. and D.R. carried out the experiments using the UbG76V-GFP HeLa cells in Figure 3B and Figure S3C–D. M.I.C. performed the experiments in Figure 5A,B. D.B. carried out the experiments in Figure S2B. Data analysis and interpretations were done by M.A., L.K.G., D.B., M.I.C. and N.L.J., M.A. and N.L.J. wrote the manuscript and all of the authors revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdullah, M., Greenfield, L.K., Bronte-Tinkew, D. et al. VacA promotes CagA accumulation in gastric epithelial cells during Helicobacter pylori infection. Sci Rep 9, 38 (2019). https://doi.org/10.1038/s41598-018-37095-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-37095-4
This article is cited by
-
A nanoparticle-based sonodynamic therapy reduces Helicobacter pylori infection in mouse without disrupting gut microbiota
Nature Communications (2024)
-
Reduction of UreB and CagA expression level by siRNA construct in Helicobacter pylori strain SS1
BMC Microbiology (2023)
-
The crosstalk between bacteria and host autophagy: host defense or bacteria offense
Journal of Microbiology (2022)
-
The impacts of probiotics in eradication therapy of Helicobacter pylori
Archives of Microbiology (2022)
-
Chronic in vivo exposure to Helicobacter pylori VacA: Assessing the efficacy of automated and long-term intragastric toxin infusion
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.