Abstract
It is unknown whether the presence of metabolic syndrome (MetS) affects the incidence of laryngeal cancer. The aim of this national population-based retrospective study was to analyze the relationship between MetS and the incidence of laryngeal cancer. Patients with laryngeal cancer (ICD-10: C32) between 2009 and 2010 were retrospectively identified and tracked until 2015 using the Korean Health Insurance claims database. During the seven-year follow-up period, 5,322 subjects were newly diagnosed with larynx cancer. The mean age of people with laryngeal cancer was much higher than those without (63.29 vs. 47.7 years, p < 0.0001), and the incidence of larynx cancer in men was much higher than that in women (93.16% vs. 6.84%, p < 0.0001). Age, gender, smoking status, alcohol intake, and exercise-adjusted hazard ratios indicated that participants with MetS had a 1.13-fold higher hazard of having larynx cancer than those without MetS. The number of MetS components was a strong risk factor for laryngeal cancer with a higher risk estimate of this cancer in both ex- and current smokers as well as people who have never smoked. MetS was found to be an independent risk factor for the incidence of laryngeal cancer. In Korea, MetS and its components are significantly associated with the development of laryngeal cancer.
Similar content being viewed by others
Introduction
Anually, nearly 10,000 people are newly diagnosed as laryngeal cancer which is one of the most common cancer of the upper aerodigestive tract1. Smoking and alcohol use are supposed to be plausible etiological risk factors for laryngeal cancer. In recent years, metabolic syndrome (MetS) is associated with an increased risk of the development or progression of cancer. The prevalence of MetS has increased worldwide, in parallel with the increasing cancer incidence2,3.
MetS is strongly associated with the cancer risk and mortality. Abdominal obesity is thought to be a major risk factor for cancer; it is significantly linked to higher risk of most common cancers and higher mortality rates4. Diabetes mellitus is also closely related with risks of cancer incidence5,6. MetS has been shown to be associated with increased incidences of prostate cancer, colorectal cancer, and the recurrence of breast cancer7,8,9,10. In patients with MetS, hormonal disturbances are usually detected, and this hormonal deregulation is presumed as a risk factor for carcinogenesis in prostate, colorectal, and endometrial cancers11,12,13. However, there has not yet been any investigation conducted to reveal the association between MetS and laryngeal cancer. Thus, we evaluated the association of larynx cancer with MetS and its individual components in the Korean population.
Results
Basic characteristics
The characteristics of the study population are summarised in Table 1. During the seven-year follow-up period, 5,322 subjects were newly diagnosed with larynx cancer. The mean age of people with laryngeal cancer was much higher than those without (p < 0.0001), and the incidence of larynx cancer in men was much higher than that in women (p < 0.0001). The percent of participants who were either current or ex-smokers and heavy drinkers was significantly higher among those with larynx cancer than among those without (p < 0.0001). Study participants with larynx cancer had significantly higher mean waist circumferences, systolic and diastolic blood pressures (BP), fasting blood glucose (FBG) levels, fasting triglyceride (TG) levels, fasting total cholesterol levels, and fasting low-density lipoprotein (LDL) cholesterol levels (p < 0.0001) than those without larynx cancer.
Relationship between individual components of MetS and larynx cancer
Table 2 presents data on the relationship between larynx cancer and each individual component of MetS according to logistic regression models. The rate of age, sex, smoking status, alcohol intake, and motor coordination risk is 1.13 times higher than that of patients without MetS. Age, gender, smoking status, alcohol intake, and exercise-adjusted hazard ratios indicate that the rate of having larynx cancer with MetS is 1.13 times higher than that of patients without MetS. The adjusted multivariable model shows that elevated FBG, elevated TG, low high-density lipoprotein (HDL) cholesterol, and elevated BP were significantly associated with an increased hazard of larynx cancer.
Relationship between MetS, the number of MetS components, and larynx cancer
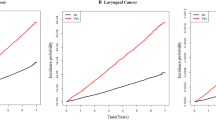
We examined the joint effect of smoking and the number of MetS components at baseline on the risk of laryngeal cancer (Table 3). The number of MetS components was found to be a strong risk factor, with a higher risk estimate of laryngeal cancer in people who are ex- or current smokers as well as people who have never smoked. Specifically, there was an association between smoking and the risk of laryngeal cancer among even those who had never smoked with three, four or five MetS components (hazard ratios [HR]: 1.224; 95% confidence intervals [CI]: 1.009–1.484). Figure 1 shows a significant linear trend between the prevalence of larynx cancer and the number of MetS components present.
Relationship between combinations of MetS components and larynx cancer
Table 4 shows the risk of developing larynx cancer according to each of the fifteen specific combinations of MetS components after adjustment for confounders: ten combinations of three components and five combinations of four components. In multivariable analyses subjects with the following three combinations had the highest HR of having larynx cancer: (1) abdominal obesity, elevated BP, and elevated FBG (HR, 1.325; 95% CI, 1.130–1.554); (2) elevated FBG, elevated BP, and elevated TG (HR, 1.129; 95% CI, 1.055–1.409); and (3) elevated TG, elevated FBG, and low HDL cholesterol (HR, 1.357; 95% CI, 1.1073–1.664). The following four combinations had the highest HR of having larynx cancer among the five combinations of four MetS components: (1) abdominal obesity, elevated TG, elevated BP, and low HDL cholesterol (HR, 1.226; 95% CI, 1.025–1.466); and (2) elevated BP, elevated TG, elevated FBG, and low HDL cholesterol (HR, 1.337; 95% CI, 1.171–1.526).
Discussion
To our knowledge, we showed that the first time report about the associations between the presence of MetS, individual MetS components, and various combinations of MetS components and laryngeal cancer. From the result of our present study, we proved that the prevalence of laryngeal cancer among a group with MetS was significantly higher than that among a group without MetS independent of age, gender, smoking status, alcohol intake, and exercise. Smoking can cuase gender based difference for laryngeal cancer. According to the National Smoking Prevalence Survey, the adult smoking rate was 79.3 percent for males and 12.6 percent for females in Korea14.
Classically, cigarette smoking has been thought of the most important risk factor for laryngeal cancer. Franceschi et al. reported that relative to non-smokers the risk among ever-smokers for larynx cancer were 4.8 (95% CI, 2.3–10.1) for low/medium and 7.1 (95% CI, 3.2–15.6) for high tar cigarettes after adjustment for other risk factors15. We determined the effect of the number of the metabolic components on the risk of larynx cancer according to smoking status. Our results showed that linear associations between the number of the components of MetS and laryngeal cancer were stronger in current smoker than in ex-smoker suggesting more pronounced effects of MetS on laryngeal cancer in current smoker than in ex-smoker. A strong association with laryngeal cancer was also observed in individuals with three, four or five components, even those who were never smokers (HR: 1.224; 95% CI: 1.009–1.484). Compared with individuals presenting none of the components of MetS, relative risks were increased 3.513 (current smoker; 95% CI, 2.924–4.222), 1.924 (ex-smoker; 95% CI, 1.592–2.336) times more for individuals who had one or two metabolic components, and 3.983 (current smoker; 95% CI, 3.307–4.797), 2.159 (ex-smoker; 95% CI, 1.782–2.616) times more for those who had three, four, or five components.
A strong association has been found between the number of MetS components and the HR of laryngeal cancer. Of the three MetS components, the combination of elevated FBG, elevated TG, and low HDL was related to the highest risk of laryngeal cancer. Of the four MetS components, the combination of elevated FBG, elevated BP, low HDL, and elevated TG was related to the highest risk of laryngeal cancer. Furthermore, elevated FBG had the highest odds for larynx cancer in Table 2 after adjustment for age, gender, exercise, smoking status, and alcohol intake (HR: 1.123; 95% CI: 1.064–1.186). This pattern emphasizes the effect of diabetes on the cancer of the larynx in the Korean population. There was also a significant linear association between the number of MetS components and the probability of developing larynx cancer. Participants with five MetS components had 1.275-fold higher odds (95% CI 1.107–1.468) of having laryngeal cancer than those without MetS (HR, 1.018; 95% CI, 0.847–1.228 in one component: HR, 1.077; 95% CI, 0.842–1.393 in two components: HR, 1.177; 95% CI, 0.914–1.542 in three components: HR, 1.179; 95% CI, 0.945–1.468 in four components). Figure 1 revealed a strong association between the prevalence of laryngeal cancer and the number of MetS components present.
Based on previous literatures, Possible mechanism of carcinogenesis of MetS is presumed as belows; (1) insulin resistance and hyperinsulinemia, (2) chronic subclinical inflammation, (3) abnormalities in sex hormones metabolism, (4) damage by endocrine disruptors exposure and air pollution, (5) chronic hyperglycemia, and (6) Disorders of circadian clock16. In the aspect of pathophysiology of MetS, hyperglycemia is considered as a key factor. Hyperinsulinemia, insulin resistance, and hyperglycemia are increasing proliferation, angiogenesis, damage to the DNA molecule by oxygen active forms due to glucose excess, cellular mobility, and apoptosis17,18,19. From the results of previous literatures, it has been suggested that, MetS affects tumor cells cancer and finally increasing the risk of cancer through the change in insulin receptor expression as well as the activation/inactivation of the growth and transcription factors, their receptors17,20,21,22. Another notable point is the role of insulin growth factor-1 (IGF-1) and insulin receptors which are overstimulated in MetS due to insulin resistance23. It is known that some tumors, especially squamous cell carcinoma in lung cancer, produce high levels of IGF-1 themselves. IGF-1 usually acts as a promoting factors for stimulation of differentiation, proliferation, and protein synthesis, and at the same time it reduces the apoptosis of cells24. IGF-1 also regulates the cell cycle through modulation of cyclin-dependent kinases, cyclin-dependent kinase inhibitors, and cyclins25. It has been revealed that in osteosarcoma, gynecological, gastrointestinal, proste and lung cancers, the increasing level of IGF-1 and changes of IGF-1 signaling pathway are frequently noticed.
This study has several limitations. First, the research groups are subject to selection bias. Although all Korean residents deserve medical evaluations every two years, it is not actually mandatory but voluntary to be able to receive medical evaluations every two years. Second, the lack of detailed biochemical information including the cancer stage, physical findings and other medical history. Third, the study cohort with laryngeal cancer was small, leading to large standard deviations. And the mean age was higher in the populations with laryngeal cancer than in those without. Age differences can contribute to the association between MetS and larynx cancer. Lastly, although this study has found a statistically significant relationship between MetS and larynx cancer, we still do not have sufficient evidence to claim causality. Based on the result of this study, further investigation to figure out the pathophysiologic mechanism between MetS and laryngeal cancer is still needed.
In conclusion, this population-based study shows evidence of the association between the presence of MetS and development of laryngeal cancer, and the increases in risk vary according to the number and various combinations of MetS components. Although precise pathophysiology could not be determined from the data in our our study, the current results may be helpful for further investigations to verify the relationship between MetS and oncogenesis of laryngeal cancer.
Materials and Methods
Study population
The Korean National Health Insurance Service (KNHIS) is the public medical insurance system which is administered by the Ministry for Health, Welfare and Family Affairs26. As a compulsory social insurance system, the KNHIS program includes about 97% of the entire Korean population. The remaining 3% of the population protected by a Medical Aid program. The KNHIS database includes patient demographics and records on diagnosis, interventions, and prescriptions27. Diagnoses were confirmed using the International Classification of Disease, Tenth Revision, Clinical Modification (ICD-10-CM) codes. Larynx cancer was defined as C32.0–32.3, C32.8, and C32.9. Informed consent was reviewed and signed by all participants. The research protocol was approved by the Institutional Review Board of the Catholic University of Korea. Methods were performed in accordance with the relevant guidelines and regulations.
Patients selection
People who join the National Health Insurance Corporation are encouraged to have standardized medical tests every two years. A total of 23,253,270 people who received the KNHIS health checkup in 2009 and 2010 were included in the KNHIS national sample cohort, and we followed these individuals until 2015. Participants were defined as having larynx cancer if they had admissions records for larynx cancer in their national health insurance data from 2009 to 2015. Participants were defined as larynx cancer if they had a hospitalization record for larynx cancer in the National Health Insurance data from 2009 to 2015. The medical examinations included measurements of height, weight, and BP. Levels of FBG, TG, total cholesterol, and HDL were also obtained. Health-related behaviors, such as past medical history and smoking, alcohol consumption and physical activity, were collected using standardized self-reporting questionnaires.
Definition of metabolic syndrome
The definition of MetS was based on a definition established by the Task Force’s joint interim report for epidemiology and prevention by the IDF Special Committee28. According to this institution, MetS should have at least three of the following five components: abdominal obesity (≥90 cm for men and ≥85 cm for women), elevated BP (systolic ≥ 130 and/or diastolic ≥ 85 mmHg), hyperglycemia (FBG ≥ 100 mg/dL), hypertriglyceridemia (TG ≥ 150 mg/dL), and low HDL-cholesterol levels (<40 mg/dL for men and <50 mg/dL for women)29. The BMI was calculated by dividing the weight in kilograms by the square of height in meters (kg/m2).
Statistical analysis
Statistical analyses were performed using SAS software (version 9.2; SAS Institute, Cary, NC, US). Baseline characteristics of study participants based on the presence of MetS are expressed as mean ± standard deviation for continuous variables and as a percentage of the number of categorical variables. The values were compared using independent t tests for continuous variables and chi-square tests for categorical variables. The incidence of larynx cancer was calculated by dividing the number of cases by 1,000 person-years. A Cox proportional risk analysis was performed to assess the association of the MetS and its components with larynx cancer, and hazard ratio (HR) and the 95% confidence interval (CI). Model 1 was unadjusted. Model 2 was adjusted for age and sex. Model 3 was additionally adjusted for smoking status, alcohol intake, and exercise. The Kaplan-Meier curve represents the cumulative probability of developing larynx cancer and a log ranking test was performed to investigate the association of the number of MetS components at risk of larynx cancer. We also assessed the risk of developing larynx cancer according to the number of MetS components used by individuals in the Cox proportional risk analysis. Analyzing hierarchy by gender and age was also performed. A p-value < 0.05 was considered statistically significant.
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics. CA Cancer J Clin. 66, 7–30 (2016).
Yunusova, N. V. et al. The role of metabolic syndrome variant in the malignant tumors progression. Diabetes Metab Syndr. S1871–4021, 30112–7 (2018).
Stoll, B. A. Western nutrition and the insulin resistance syndrome: a link to breast cancer. Eur J Clin Nutr. 53, 83–7 (1999).
Calle, E. E. & Kaaks, R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer. 4, 579–91 (2004).
Jee, S. H. et al. Fasting serum glucose level and cancer risk in Korean men and women. JAMA. 293, 194–202 (2005).
Inoue, M. et al. Diabetes mellitus and the risk of cancer: results from a large-scale population-based cohort study in Japan. Arch Intern Med. 166, 1871–7 (2006).
Chiu, H. M. et al. Association of metabolic syndrome with proximal and synchronous colorectal neoplasm. Clin Gastroenterol Hepatol. 5, 221–9 (2007).
Laukkanen, J. A. et al. Metabolic syndrome and the risk of prostate cancer in Finnish men: a population-based study. Cancer Epidemiol Biomarkers Prev. 13, 1646–50 (2004).
Lund Håheim, L., Wisløff, T. F., Holme, I. & Nafstad, P. Metabolic syndrome predicts prostate cancer in a cohort of middle-aged Norwegian men followed for 27 years. Am J Epidemiol. 164, 769–74 (2006).
Pasanisi, P. et al. Metabolic syndrome as a prognostic factor for breast cancer recurrences. Int J Cancer. 119, 236–8 (2006).
Trabert, B. et al. Metabolic syndrome and risk of endometrial cancer in the united states: a study in the SEER-medicare linked database. Cancer Epidemiol Biomarkers Prev. 24, 261–7 (2015).
Samad, A. K., Taylor, R. S., Marshall, T. & Chapman, M. A. A meta-analysis of the association of physical activity with reduced risk of colorectal cancer. Colorectal Dis. 7, 204–13 (2005).
Esposito, K. et al. Effect of metabolic syndrome and its components on prostate cancer risk: meta-analysis. J Endocrinol Invest. 36, 132–9 (2013).
Korean Association of Smoking and Health. National Smoking Prevalence Survey. Available, http://www.kash.or.kr/user_new/main.asp.
Franceschi, S. et al. Smoking and drinking in relation to cancers of the oral cavity, pharynx, larynx, and esophagus in Northern Italy. Cancer Res 50, 6502–6507 (1990).
Bellastella, G., Scappaticcio, L., Esposito, K., Giugliano, D. & Maiorino, M. I. Metabolic syndrome and cancer: The common soil hypothesis. Diabetes Res Clin Pract. [Epub ahead of print] (26 May 2018).
Yunusova, N. V. et al. Association of IGFBP-6 Expression with Metabolic Syndrome and Adiponectin and IGF-IR Receptor Levels in Colorectal Cancer. Asian Pac J Cancer Prev. 17, 3963–9 (2016).
Berstein, L. M. Modern approach to metabolic rehabilitation of cancer patients: biguanides (phenformin and metformin) and beyond. Future Oncol. 6, 1313–23 (2010).
Chia, P. P., Fan, S. H. & Say, Y. H. Screening of Peroxisome Proliferator-Activated Receptors (PPARs) alpha, gamma and alpha Gene Polymorphisms for Obesity and Metabolic Syndrome Association in the Multi-Ethnic Malaysian Population. Ethn Dis. 25, 383–90 (2015).
Gao, J. et al. Leptin induces functional activation of cyclooxygenase-2 through JAK2/STAT3, MAPK/ERK, and PI3K/AKT pathways in human endometrial cancer cells. Cancer Sci. 100, 389–95 (2009).
Kim, A. Y. et al. Adiponectin represses colon cancer cell proliferation via AdipoR1- and -R2-mediated AMPK activation. Mol Endocrinol. 24, 1441–52 (2010).
Wang, Y. et al. Visfatin stimulates endometrial cancer cell proliferation via activation of PI3K/Akt and MAPK/ERK1/2 signalling pathways. Gynecol Oncol. 143, 168–78 (2016).
Ouchi, N., Parker, J. L., Lugus, J. J. & Walsh, K. Adipokines in inflammation and metabolic disease. Nat Rev Immunol. 11, 85–97 (2011).
Mendonca, F. M. et al. Metabolic syndrome and risk of cancer: which link? Metabolism. 64, 182–9 (2015).
Braun, S., Bitton-Worms, K. & LeRoith, D. The link between the metabolic syndrome and cancer. Int J Biol Sci. 7, 1003–15 (2011).
Kim, D. S. Introduction: health of the health care system in Korea. Soc Work Public Health 25, 127–41 (2010).
Yhim, H. Y. et al. Incidence of venous thromboembolism following major surgery in Korea: from the Health Insurance Review and Assessment Service database. J Thromb Haemost 12, 1035–43 (2014).
KGMM, A., Zimmet, P. & Shaw J. Metabolic syndrome-a new world-wide definition. A consensus statement from the international diabetes federation. Diabet Med. 23, 469–80 (2006).
Renehan, A. G., Frystyk, J. & Flyvbjerg, A. Obesity and cancer risk: the role of the insulin–IGF axis. Trends Endocrinol Metab. 17, 328–36 (2006).
Acknowledgements
This work was supported, in part, by grants from the Korean Society of Otorhinolaryngology-Head and Neck Surgery, 2017, and the alumni associated of the Department of Otolaryngology Head and Neck Surgery, The Catholic University of Korea, 2017.
Author information
Authors and Affiliations
Contributions
S.Y.K. wrote the first draft of the manuscript. K.D.H. took part in the data analyses and performed statistical analyses. Y.H.J. designed the study and critically revised the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, SY., Han, Kd. & Joo, YH. Metabolic Syndrome and Incidence of Laryngeal Cancer: A Nationwide Cohort Study. Sci Rep 9, 667 (2019). https://doi.org/10.1038/s41598-018-37061-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-37061-0
This article is cited by
-
Identification of Metabolic Syndrome-Related miRNA–mRNA Regulatory Networks and Key Genes Based on Bioinformatics Analysis
Biochemical Genetics (2023)
-
Association between metabolic syndrome and gastric cancer risk: results from the Health Examinees Study
Gastric Cancer (2023)
-
Synergistic association between underweight and type 2 diabetes on the development of laryngeal cancer: a national population-based retrospective cohort study
BMC Cancer (2022)
-
The effect of metabolic syndrome on head and neck cancer incidence risk: a population-based prospective cohort study
Cancer & Metabolism (2021)
-
Contribution of RAGE axis activation to the association between metabolic syndrome and cancer
Molecular and Cellular Biochemistry (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.