Abstract
Smoking is known to increase cardiovascular events, but the association and mechanisms between smoking and ventricular arrhythmic events in dilated cardiomyopathy (DCMP) are unknown. The purpose of this study is to investigate the hypothesis that smoking is associated with sudden cardiac death (SCD) and ventricular arrhythmia in DCMP patients. We enrolled 378 patients who underwent cardiovascular magnetic resonance imaging (cMRI) and were diagnosed with DCMP at two general hospitals in Korea. The clinical data and left ventricular late-gadolinium enhancement (LV-LGE) of all patients were analyzed according to being never-smokers or smokers. Smokers were more likely to be male than never-smokers, but there was no other clinical difference between them. Smokers had a greater LV-LGE ratio, and multi-segment involvement of LV-LGEs. Smoking and a low left ventricular (LV) ejection fraction were significant predictors of the presence of LV-LGEs even after adjusting for optimal medical therapy. In addition, smokers had a higher fatal ventricular arrhythmic (FVA; sustained ventricular tachycardia, and ventricular fibrillation) and FVA + SCD, and ex-smokers had a similar FVA to never-smokers during 44.3 ± 36.4 months of follow-up. Finally, smoking independently increased the FVA + SCD even after adjusting for the clinical variables and LV-LGE. Smoking is associated with a multi-segmental involvement of LV-LGE and increased FVA + SCD in DCMP patients when compared to never-smokers.
Similar content being viewed by others
Introduction
Cigarette Smoking is a well-known risk factor for significantly increasing the cardiovascular morbidity and mortality1. In the U.S., approximately 140,000 premature deaths per year from cardiovascular disease are triggered by cigarette smoking2. Although the exact components and mechanism of cigarette smoking that are related to increased cardiovascular morbidity are unclear, cigarette smoking is known to increase inflammation, thrombosis, oxidation of low-density lipoprotein cholesterol, and trigger fibrotic processes in body tissues including atrial muscle3,4,5,6. Cardiac fibrosis has a strong correlation with systolic dysfunction, diastolic dysfunction, and abnormal electrical excitation; thus, it is also known to increase the incidence of arrhythmias, ventricular tachycardia, and sudden cardiac attacks. Studies reveal that the extracellular matrix in between cardiac myocytes slows the electrical conduction and the myofibroblasts produce ectopic electrical activity, which all-together eventually form micro-reentrant circuits within the endocardial tissue, leading to arrhythmogenesis3. Therefore, cardiac fibrosis is suggested as a fundamental factor for predicting the cardiovascular morbidity and mortality by modifying the mechanical, electrical, and vasomotor function7. In the clinical field, cardiac fibrosis can be evaluated through late-gadolinium enhancement (LGE) by cardiovascular magnetic resonance (CMR) imaging8. Recent studies have shown an excellent agreement of the histologic pattern of cardiac fibrosis with in vivo CMR imaging. Using LGE-CMR imaging, the results exposed that the likelihood of the developing arrhythmias in dilated cardiomyopathy (DCMP) is higher in people with midwall fibrosis than in those without fibrosis. Moreover, it has been reported that myocardial fibrosis assessed by LGE-cMRI is associated with cardiovascular mortality and sudden cardiac death (SCD) in patients with dilated cardiomyopathy (DCMP)9. In fact, it is known that as fibrosis measured by the LGE-CMR increases by 3%, the all-cause mortality increases by a mean of 55%7. Therefore, the aim of this study was to investigate the association between smoking and myocardial fibrosis assessed by LGE-CMR in DCMP patients and to determine whether the smoking is associated with incidence of arrhythmic events due to myocardial fibrosis including ventricular arrhythmias and sudden cardiac death (SCD). We limited our case-group to non-ischemic cardiomyopathy (NICM) patients to exclude ventricular fibrosis associated with coronary artery disease10. Further, to support our hypothesis, we divided our group into smokers and never-smokers. Then we compared the amount of cardiac fibrosis within the two groups and analyzed the relationship between left ventricular fibrosis using the LGE by CMR imaging and the incidence of arrhythmic events including ventricular arrhythmias, and SCD.
Methods
Study population and design
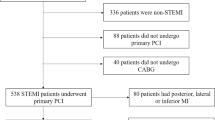
The study protocol was approved by the institutional review boards of two general hospitals. The study protocol was approved by the Institutional Review Board of Yonsei University Health System and Ewha Womans University Mokdong Hospital and conducted in accordance with the tenets of the Declaration of Helsinki (EUMC 2015-07-046-016). All patients provided written informed consent. A total of 378 patients who were diagnosed with non-ischemic DCMP and underwent CMR imaging between May 2003 and December 2015 at two tertiary hospitals in Korea were retrospectively enrolled in this study. All patients underwent a detailed history and clinical evaluation including a 12-lead electrocardiogram (ECG), 2-dimensional transthoracic echocardiography, contrast enhanced CMR, and coronary angiography or coronary computed tomography (CT). DCMP was defined in accordance with the World Health Organization/International Society and Federation of Cardiology’s guidelines11. Thus, studies that were included in this analysis met the following criteria. (1) Patients with a left ventricular ejection fraction (LVEF) of <50% without regional wall-motion abnormalities, (2) LV diastolic dimension of >55 mm, (3) symptoms or signs of heart failure according to the Framingham criteria, and (4) the absence of significant coronary artery disease (CAD) on angiography or 3-dimensional cardiac CT (to ensure exclusion of >50% obstructions of one or more coronary arteries) were included in this study10,12. Patients with significant valvular heart disease of more than moderate to severe, hypertrophic cardiomyopathy, restrictive cardiomyopathy, prior cardiac surgery, or structural heart disease were excluded.
Echocardiography measurements
All patients underwent trans-thoracic echocardiography (TTE; Sonos 5500, Philips Medical System, Andover, MA, USA or Vivid 7, GE Vingmed Ultrasound, Horten, Norway). The LVEF, chamber size (left atrial volume index [LAVI], LA dimension, wall thickness of the LV, and LV mass index [LVMI]), transmitral flow velocity (E wave, A wave), and tissue Doppler images of the mitral annular septal area (peak diastolic velocity [Em], peak systolic velocity [S’]) were acquired according to the American Society of Echocardiography guidelines13,14.
The definition of smoking, alcohol, and medication history
The information on the exposure of smoking and alcohol was acquired from patient questionnaires or medical records at the first visit to the hospital. (1) smokers were defined as having a smoking exposure if they used more than 100 cigarettes in their lifetime (ex-smoker + current smokers), (2) never-smokers were defined as those with a smoking exposure of less than 100 cigarettes over their lifetime, (3) ex-smokers were defined as those with smoking cessation from at least 1 year prior, and (4) current smokers were defined as those with a smoking exposure of more than 100 cigarettes, and that had smoked within the last year. The definition of alcohol intake was described as a frequency of ≥1–3 times per month. The medication history of the patients was analyzed based on the chart review of their use of the following drugs. Angiotensin converting enzyme inhibitors (ACEis) or angiotensin receptor blockers (ARBs), beta-blockers (BBs), diuretics, aldosterone antagonists, statins, digoxin, and amiodarone were included, and the use of each medication was defined for a prescription of more than at least 3 months regardless of the dose.
CMR imaging
All CMR imaging studies were performed using a 1.5-T scanner (Intera Achieva; Philips Medical Systems, Best, the Netherlandsor Philips Healthcare, Andover, MA, USA) with a phased array cardiac coil. electrocardiogram (ECG)-gated cine imaging was performed using a balanced steady-state free precession sequence with the following parameters: TR/TE, 3.4/1.7 ms; flip angle, 50°; field of view, 360 × 360 mm; matrix, 256 × 256; slice thickness, 8 mm; 25 phases per cardiac cycle; average number of signals, 1; and short axis planes encompassing the entire LV without a slice gap. Delayed enhancement imaging was performed 10 minutes after an intravenous injection of gadolinium (0.2 mmol/kg; gadoterate dimeglumine; Dotarem, Geurbet) at 2 mL/sec. Image acquisition was synchronized with the ECG in the mid-diastolic phase in order to minimize motion artifact. An inversion time (TI) was individually optimized to nullify the signal of the normal myocardium using a dedicated TI-determining sequence15.
Image analysis
All CMR images were transferred to a dedicated software program for analysis (CMR42, Circle Cardiovascular Imaging, Calgary, Alberta, Canada). The images were reviewed by three radiologists (H.J.L, Y.J.K., and YKK with 8, 11 and 25 years of experience in cardiac imaging, respectively) in consensus. Cine images were analyzed to determine the ventricular volume and ejection fraction using a semi-automatic segmentation in the software. The LGE was assessed using a modified 16-segment model of the LV16, and each segment model was rearranged to the anterior, interventricular septum, inferior, and lateral wall. In addition, the junction between the LV and right ventricle (RV) was described as a focal, hyperintensity area confined to the junction of the RV wall to the anterior and/or posterior interventricular septum, and multi-segment involvement was defined as involvement of more than 3 segments. An LGE quantification was performed. A semiautomatic segmentation of the endocardial and epicardial borders was performed in each short axis image in order to obtain the myocardial volume. The LGE volume was quantified using a full width at half maximum (FWHM) technique and the region of interest was drawn in the area of the maximum signal intensity of a visible LGE for the FWHM threshold. The myocardial and LGE volumes were determined as the sum of each area for each slice, multiplied by the slice thickness. The percentage of the LGE was calculated by dividing the LGE volume by the myocardial volume, with a quotient multiplied by 100. We used the median value as the cut-off of the LGE volume in the DCMP patients, and in this study, the median value of the LGE volume was 3.5%. We analyzed the patients after dividing the groups into those with an LGE extent of ≥3.5% and those with an LGE extent <3.5%. The CMR imaging was evaluated by three radiologists in each hospital for the location, and quantification of the LGE. As previously reported17, the inter-observer agreement between the first two readers was substantial (kappa value = 0.827, p < 0.005). The intra-observer variability of the LGE quantification for the CV and ICC were 12.5% and 0.99 (95% confidence interval [CI] 0.97–0.99), respectively17.
Follow up
After the standardized data collection was completed, all case records were reviewed for the purposes of obtaining additional information. Follow-up data were obtained by a detailed review of all medical records of all patients. Patients had regular follow-ups with or without a standard 12-lead ECG in the outpatient clinic every 3 to 6 months, or when symptoms occurred. Patients with symptoms suggestive of arrhythmias underwent ambulatory Holter monitoring (24 hours) and/or event recording. Patients without any symptoms were evaluated every year with 24-hour Holter monitoring. The analysis of the ECG Holter recordings focused on ventricular tachycardia (VT), either non-sustained (NSVT) or sustained (SuVT). NSVT was defined as a tachycardia (≥100 beats/min) of a ventricular origin that self-terminated within 30 seconds, and SuVT was defined as that which lasted for more than 30 seconds. Ventricular fibrillation (VF) that was identified by the QRS complexes had a markedly different morphology, axis, and amplitude and no obvious P waves were observed and the rate was irregular and usually greater than 300 beats per minute.
Implantable cardioverter defibrillators (ICDs) or cardiac resynchronization therapy devices with a defibrillator (CRT-D) that were implanted for primary prevention were decided by the physician’s discretion and patient’s willingness. A routine ICD or interrogation (at 1 and 3 months; and every 3 months thereafter) and ECG recordings at the time of the symptoms were used to document the occurrence of spontaneous VT during the follow-up period in all patients. An appropriate ICD intervention was defined as a device shock or anti-tachycardia overdrive pacing delivered in response to a VT and documented in the stored intracardiac ECG data. All interrogations were identified and adjudicated by two electrophysiologists (D.G.S. and J.B.P); who were blinded to the clinical data, including the CMR analyses. The outcomes of this study were defined as: (1) major ventricular arrhythmias (MVAs) including NSVT, SuVT, and VF and (2) fatal ventricular arrhythmias (FVAs), including SuVT and VF. We described SCD as an unexpected natural death from a cardiac cause within 1 hour from the onset of symptoms, in a person without any prior condition that would appear fatal18. In addition, the cause and date of death were confirmed by information from the National Population Registry of the Korea National Statistical Office, together with a review of all available clinical records at the time of death17.
Statistical analysis
Continuous variables are reported as the mean ± standard deviation (SD). Continuous variables were analyzed using independent t-tests. Normality was determined using the Kolmogorov-Smirnov goodness-of-fit test. Categorical variables were reported as numbers and percentages and were analyzed using Pearson’s chi-squared tests or Fisher’s exact tests, as appropriate. Cox regression and Kaplan-Meier analysis were performed for predictors of FVA(+SCD) and smoking or never smoking groups, respectively. A P-value ≤ 0.05 was considered statistically significant.
Results
A total of 378 patients (62.2% male, 54.3 ± 14.4 years old) were enrolled for the analysis. Among them, there were 131 (34.7%) smokers, including 48 (12.7%) ex-smokers and 83 (22.0%) current smokers, and there were 247 (65.3%) never-smokers. Smokers more usually were male (95.4 vs. 44.5%, p < 0.001) and drank more alcohol (77.1 vs. 17.0%, p < 0.001) than never-smokers. However, there was no significant difference in the age and co-morbidities such as hypertension and diabetes (Table 1). Figure 1 shows the representative examples of an LV-LGE in a smoker and never-smoker in patients with DCMP. Regarding the cardiac function and MRI findings, the LVEF and end diastolic volume (EDV) also did not exhibit any significant differences between the two groups. However, smokers had a larger ratio of the LV-LGE than the never-smokers (9.3 ± 13.5% vs. 6.8 ± 11.2%, p = 0.059), and the proportion of patients with an LV-LGE of ≥3.5% (median values) was prominently higher in the smoking groups than never-smokers (58.8% vs. 45.3%, p = 0.019). In an analysis of the location of the LV-LGE, the smokers had a greater multi-segmental involvement (≥3 segments; 20.6% vs. 11.7%, p = 0.02) than the never-smokers (Table 2). In a subgroup analysis, the proportion of patients with an LV-LGE ≥3.5% was prominently higher in the ex-smoking groups than the current- and never smokers (69% vs. 53% vs. 46%, p = 0.014). In an analysis of the LV-LGE location, current- smokers had a greater multi-segmental involvement (23% vs. 11% vs. 16%, p = 0.038) than the never-smokers and ex-smokers (Supplement Table 1).
LV fibrosis assessment by LV-LGE is a kind of LV remodeling in NICM patients with ventricular dysfunction. Just a low LVEF was associated with an increased LV-LGE (OR = 0.954, 95% CI 0.924–0.985, p = 0.004), but, the age, gender, and LV dilatation did not have a significant association with the formation of an LV-LGE in the multivariate analysis (Table 3). Especially, alcohol and smoking were associated with the presence of an LV-LGE, even after adjusting for the use of optimal heart failure medications. Finally, a low LVEF (OR = 0.953, 95% CI 0.920–0.987, p = 0.008), exposure to alcohol (OR = 3.239, 95% CI 1.196–8.774, p = 0.021), and smoking (OR = 3.694, 95% CI 1.396–9.775, p = 0.008) were associated with the formation of an LV-LGE (Table 3).
In an analysis of ventricular arrhythmias, the incidence of NSVTs did not exhibit any significant difference between never-smokers and smokers, but SuVTs (7.6% vs. 3.2%, p = 0.05) and VF (4.6% vs. 0.8%, p = 0.015) were significantly increased in smokers as compared to never-smokers (Fig. 2-A). When combined with ventricular arrhythmias and SCD, the incidence of MVAs (16% vs. 8.9%, p = 0.038), FVAs (10.7% vs. 2.8%, p = 0.002), MVA + SCDs (22.9%, vs. 13.4%, p = 0.018), and FVA + SCDs (17.6% vs. 8.5%, p = 0.009) were significantly increased in smokers as compared to never-smokers (Fig. 2-B). In a subgroup analysis, current smokers had the highest incidence of MVAs (10% vs. 9% vs. 19%, p = 0.030), FVAs (6% vs. 3% vs. 13%, p = 0.001), MVA + SCDs (17% vs. 13%. Vs. 27%, p = 0.016) and FVA + SCDs (13% vs. 9% vs. 20%, p = 0.010) as compared to ex- and never smokers, and ex-smokers had a relatively moderate risk compared to that of the other two groups (Fig. 2-D).
During a follow-up duration of 44.3 ± 36.4 months, smokers had significantly increased FVA events as compared to never-smokers (Log Rank p = 0.002, Fig. 3-A), and this result also was consistent in the subgroup analysis of patients with a low EF (<35%) (Log Rank p = 0.043, Fig. 3-B). The FVA free survival of ex-smokers was located between never- and current smokers, which represented that stopping smoking may have protective effects on FVAs (Log Rank p = 0.002, Fig. 3-C). When considering most smokers were male (95.4%), male smokers also had significantly more FVA events than male never-smokers (Log Rank p = 0.043, Fig. 3-D). In an analysis combining an LGE and smoking, never-smokers without an LGE (−) had the lowest number of FVA events, and smokers with an LGE (+) had the highest number of FVA events. Especially smokers without an LGE (−) had a higher risk of FVAs than never-smokers with an LGE (+), and as a consequence, smoking had a greater association with the occurrence of FVAs than the presence of an LGE (Fig. 4-A). Also, in an analysis of FVA + SCD, an LGE (+) and smoking had consistent effects on ventricular arrhythmic events (Fig. 4-B). In a Cox regression multivariate analysis, a young age (HR = 0.96, 95% CI 0.95–0.996, p = 0.028), low body mass index (BMI) (HR = 0.83, 95% CI 0.716–0.962, p = 0.014), increased LVEDV (HR = 1.004, 95% CI 1.001–1.006, p = 0.004), alcohol intake (HR = 3.909, 95% CI 1.005–15.208, p = 0.049), and smoking (HR = 5.588, 95% CI 1.389–22.490, p = 0.015) were associated with FVAs or SCD. Finally, a low BMI and diastolic BP including smoking were common predictors of FVAs and FVA + SCD in patients with DCMP (Table 4), in addition, in the ROC curve analysis, the AUC area of the FVA group including smoking was 0.822, and the AUC area in the FVA + SCD group was 0.787, respectively (Supplement Fig. 1).
Discussion
The findings of the present study can be summarized as follows: (1) In patients with DCMP, smokers were more likely to be male, and have multi-segmental involvement, (2) smoking and alcohol intake were associated with the presence of an LV-LGE, regardless of the optimal use of HF medications and a geometric change in the LV, (3) smokers had an increased number of FVAs as compared to the never-smokers, and stopping smoking within more than 1 year may have a protective effect on FVAs, and (4) smoking was an independent predictor of FVAs or FVA + SCD in patients with DCMP.
The LGE-CMR has been routinely used for the assessment of myocardial fibrosis in patients with DCMP8. The reason is that the extent of the myocardial fibrosis can be determined by the LGE19, the presence of which predicts cardiac events occurring in patients with DCMP8. In various cardiovascular diseases, the detection of fibrosis is a useful assessment of myocardial viability20, and the presence of fibrosis is a better marker of VT inducibility than the LVEF21. The available evidence also has proven that myocardial fibrosis, demonstrated by LGE-CMR, is an important predictor of cardiac mortality in non-ischemic cardiomyopathy17,22. Therefore, it has been reported that the LGE-CMR might be a useful tool for selecting suitable patients for primary ICD implantations in patients with non- ischemic cardiomyopathy23. In the present study, an increased LV-LGE was associated with a low LVEF in patients with DCMP. This is in agreement with the findings from the previous studies8. We also found that an LV-LGE in DCMP patients was associated with a worse prognosis such as SCD and FVA events. These results are based on the theories of the previous studies and suggest that an evaluation of LV-LGEs in patients with DCMP is clinically important.
It has been reported that smoking is associated with poorer outcomes in patients with DCMP24,25. Additionally, the association between smoking and cardiomyopathy has also been proposed by several animal studies26,27. Possible mechanisms underlying the association between smoking and non-ischemic cardiomyopathy include cardiac muscle damage by a disturbance in the oxidative processes and cardiac susceptibility after viral infections27,28. Although it is well known that smoking increases the cardiovascular mortality and morbidity, the association between smoking and an LV-LGE in patients with DCMP is not yet clear. In this study, we found that the smoking was associated with the presence of an LV-LGE, and smokers had a greater ratio of LV-LGEs than never-smokers. Especially, alcohol and smoking were associated with the presence of an LV-LGE, even after adjusting for the use of optimal heart failure medications. Additionally, in our data, the incidence of SuVTs and VF was significantly increased in smokers as compared to never-smokers. These findings suggest that smoking might be related to an increase in an LV-LGE formation and the incidence of FVAs in patients with DCMP.
Myocardial fibrosis is caused by a variety of factors, including alcohol intake, diabetes, hypertension, and smoking. Fibrosis due to alcohol intake is known to be caused by an increased diastolic stiffness and diastolic dysfunction of the left ventricle29. The mechanism of myocardial fibrosis due to hypertension has been reported to be caused by left ventricular diastolic dysfunction30,31. In addition, several cellular mechanisms of diabetic myocardial fibrosis have been reported to include an impaired excitation-contraction coupling, reduced coronary flow reserve, inefficient energy production, and fibrotic remodeling32. In previous reports, hypertension and diabetes influenced the formation of more myocardial fibrosis, so that, thus causing ventricular arrhythmias33,34. However, in our data (Table 1), there was no difference in the comorbid diseases between the two groups. Further, in Table 3, hypertension and diabetes had no association with the formation of an LGE (fibrosis). Although, no difference was found between the comorbid diseases between the groups, diabetes and hypertension singly may alter the myocardial vulnerability and cause arrhythmogenesis. The mechanisms of myocardial fibrosis in DCMP are complex and include inflammation, a genetic predisposition, micro-vascular ischemia, and neurohumoral changes35. Especially, smoking is one of the most important modifiable risk factors for various cardiovascular disease. Further, myocardial and endothelial cells are the targets for which tobacco smoke exerts its effects. Smoking has been reported to affect endothelial cell dysfunction such as endothelial cell injury, increased endothelial permeability, nitric oxide production, and the binding of inflammatory cells forming atherosclerotic plaques36,37. There was also a report that gene expressions related to metabolism, hypoxia, and a response to hormone stimulation were differentially expressed in smokers as compared to non-smokers38. Furthermore, one of the mechanism by which smoking affects cardiovascular disease is through chronic sympathetic activation as demonstrated by the increase in plasma epinephrine concentration levels, heart rate, systolic, diastolic, blood pressure and CO levels. Thus, these results suggest that smoking is a potential mechanism for inducing myocardial fibrosis and increasing the risk of ventricular arrhythmias39,40. Based on these mechanisms, our results showed that the pattern of fibrosis due to smoking was not exactly matched with the territory of the coronary arteries. Further, these kinds of patterns, such as multi-segment involvement including many conductive channels, could induce more ventricular arrhythmias. Yoshida A. et al. reported that a coexisting LV-LGE and perfusion-metabolism mismatch predict future cardiac events in patients with DCMP41. Moreover, multi-segmental involvement of fibrosis may represent many viable tissues and conductive channels for re-entrant circuits between fibrosis. Further, this finding is consistent with previous reports, which ventricular arrhythmias needed conductive channels for re-entrant circuits in the peri-scar region42. The location of the LV-LGE as well as the amount of an LV-LGE were also important in the prognosis of the patients. In our study, in an analysis of the location of the LV-LGE, smokers had a more multi-segmental involvement compared to never-smokers. Multi-segmental involvement of fibrosis was not matched with usual coronary territory, which may suggest a non-ischemic origin. Our study suggested that smoking and the LV-LGE location are clinically related and increase the risk of extended cardiomyopathy. Thus, we thought that further study of hypoxia and the perfusion-metabolism of the myocardium by smoking is needed. However, we clinically showed that a coexisting LV-LGE and smoking had the highest incidence of FVAs and SCD. Finally, although the presence of an LV-LGE could affect the cardiac mortality in DCMP patients, smoking was also a very important risk factor regardless of the presence of an LV-LGE.
Clinical implications
Our results suggest that the association between smoking and an LGE is an important factor for ventricular arrhythmias. Patients with LV-LGEs, smoking and a low LVEF should be recognized as having a high-risk for fatal ventricular arrhythmias in DCMP. Therefore, based on the guidance recommendations, major precautions for FVAs and SCD in smokers with an LGE are needed. Another important result of our study was that current smokers had the highest incidence of FVAs and FVA + SCD compared to that of the ex- and never smokers. Importantly, the FVA free survival of ex-smokers was located between never- and current smokers, which represented that stopping smoking may have protective effects on FVAs.
Study Limitations
This study had several limitations. First, NICM patients were classified by coronary angiography (CAG) and 3-dimensional cardiac CT assessment. At least in the early-stage of DCMP patients10, ischemic cardiomyopathy (ICM) was excluded. However, if NICM patients continuously smoke, it was not possible to exclude that ischemic events occurred during follow-up. Second, this study was a retrospective analysis, and included a select group of patients referred for treatment of cardiomyopathy. The data used in the study were acquired through a retrospective review of the patient’s charts. Thus, there was selection bias and limitations on the data acquisition. Third, only a few patients among those who met the indication for primary prevention received an ICD or CRT-D implantation. Therefore, fewer arrhythmic events in the patients might have been recorded due to suboptimal detection methods. Fourth, the patients did not undergo cardiac biopsy for the evaluation of the definite etiology and myocardial fibrosis. However, we excluded patients with features suggesting cardiomyopathies other than DCMP on CE-CMR. Fifth, diabetes and hypertension can affect myocardial fibrosis formation as well as smoking and can cause arrhythmias. However, there are limitations in comparing the single effects of smoking and alcohol consumption, diabetes, and hypertension, respectively. Especially, cardiomyopathic patients intaking alcohol are addicted to smoking, and patients with hypertension may have diabetes together. Therefore, it is difficult to prove the individual effect of each on myocardial fibrosis.
Conclusion
Our study is the first to show a relationship between smoking and the formation of an LV-LGE in patients with DCMP. Smokers had a greater ratio of the LV-LGEs than never-smokers. Especially, alcohol and smoking were associated with the presence of an LV-LGE, even after adjusting for the use of optimal heart failure medications. Moreover, smokers had increased FVAs as compared to never-smokers. Importantly, the FVA free survival of ex-smokers was located between never- and current smokers, which represented that stopping smoking may have protective effects on FVAs. Therefore, a combined analysis of LV-LGEs and smoking is very important in DCMP patients and may be a useful marker for selecting patients with a high risk of FVAs and SCD.
References
Ambrose, J. A. & Barua, R. S. The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol 43, 1731–1737, https://doi.org/10.1016/j.jacc.2003.12.047 (2004).
In The Health Consequences of Smoking: A Report of the Surgeon General Reports of the Surgeon General (2004).
Rockey, D. C., Bell, P. D. & Hill, J. A. Fibrosis–a common pathway to organ injury and failure. N Engl J Med 372, 1138–1149, https://doi.org/10.1056/NEJMra1300575 (2015).
Zein, C. O. et al. Smoking and severity of hepatic fibrosis in nonalcoholic fatty liver disease. J Hepatol 54, 753–759, https://doi.org/10.1016/j.jhep.2010.07.040 (2011).
Zein, C. O. et al. Smoking and increased severity of hepatic fibrosis in primary biliary cirrhosis: A cross validated retrospective assessment. Hepatology 44, 1564–1571, https://doi.org/10.1002/hep.21423 (2006).
Goette, A. et al. Cigarette smoking induces atrial fibrosis in humans via nicotine. Heart 93, 1056–1063, https://doi.org/10.1136/hrt.2005.087171 (2007).
Wong, T. C. et al. Association between extracellular matrix expansion quantified by cardiovascular magnetic resonance and short-term mortality. Circulation 126, 1206–1216, https://doi.org/10.1161/CIRCULATIONAHA.111.089409 (2012).
Assomull, R. G. et al. Cardiovascular magnetic resonance, fibrosis, and prognosis in dilated cardiomyopathy. J Am Coll Cardiol 48, 1977–1985, https://doi.org/10.1016/j.jacc.2006.07.049 (2006).
Gulati, A. et al. Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathy. JAMA 309, 896–908, https://doi.org/10.1001/jama.2013.1363 (2013).
Pueschner, A. et al. The Prevalence, Correlates, and Impact on Cardiac Mortality of Right Ventricular Dysfunction in Nonischemic Cardiomyopathy. JACC Cardiovasc Imaging 10, 1225–1236, https://doi.org/10.1016/j.jcmg.2017.06.013 (2017).
Richardson, P. et al. Report of the 1995World Health Organization/International Society and Federation of Cardiology Task Force on the Definition and Classification of cardiomyopathies. Circulation 93, (841–842 (1996).
Felker, G. M., Shaw, L. K. & O’Connor, C. M. A standardized definition of ischemic cardiomyopathy for use in clinical research. J Am Coll Cardiol 39, 210–218 (2002).
Nagueh, S. F. et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 22, 107–133, https://doi.org/10.1016/j.echo.2008.11.023 (2009).
Lang, R. M. et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18, 1440–1463, https://doi.org/10.1016/j.echo.2005.10.005 (2005).
Messroghli, D. R. et al. Modified Look-Locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn Reson Med 52, 141–146, https://doi.org/10.1002/mrm.20110 (2004).
Cerqueira, M. D. et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. J Nucl Cardiol 9, 240–245 (2002).
Shin, D. G. et al. Pattern of late gadolinium enhancement predicts arrhythmic events in patients with non-ischemic cardiomyopathy. Int J Cardiol 222, 9–15, https://doi.org/10.1016/j.ijcard.2016.07.122 (2016).
Zipes, D. P. et al. ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation 114, e385–484, https://doi.org/10.1161/CIRCULATIONAHA.106.178233 (2006).
Kim, R. J. et al. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation 100, 1992–2002 (1999).
Kim, R. J. et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med 343, 1445–1453, https://doi.org/10.1056/NEJM200011163432003 (2000).
Bello, D. et al. Infarct morphology identifies patients with substrate for sustained ventricular tachycardia. J Am Coll Cardiol 45, 1104–1108, https://doi.org/10.1016/j.jacc.2004.12.057 (2005).
Wu, K. C. et al. Late gadolinium enhancement by cardiovascular magnetic resonance heralds an adverse prognosis in nonischemic cardiomyopathy. J Am Coll Cardiol 51, 2414–2421, https://doi.org/10.1016/j.jacc.2008.03.018 (2008).
Chimura, M. et al. Distribution of ventricular fibrosis associated with life threatening ventricular tachyarrhythmias in patients with nonishcemic dilated cardiomyopathy. J Cardiovasc Electrophysiol, https://doi.org/10.1111/jce.12767 (2015).
Li, X. et al. The effects of smoking and drinking on all-cause mortality in patients with dilated cardiomyopathy: a single-center cohort study. Eur J Med Res 20, 78, https://doi.org/10.1186/s40001-015-0171-z (2015).
Wang, J. et al. Comparison of Various Strategies for the Prognosis and Outcomes of Ischaemic Dilated Cardiomyopathy in Smokers: Complete Revascularisation and Smoking Cessation Produces a Superior Outcome. Heart Lung Circ 26, 463–476, https://doi.org/10.1016/j.hlc.2016.09.003 (2017).
Ahmed, S. S., Moschos, C. B., Oldewurtel, H. A. & Regan, T. J. Myocardial effects of long-term cigarette smoking: relative roles of carbon monoxide and nicotine. Am J Cardiol 46, 593–598 (1980).
Gvozdjakova, A. et al. Smoke cardiomyopathy: disturbance of oxidative processes in myocardial mitochondria. Cardiovasc Res 18, 229–232 (1984).
Hayes, J. M. & Hall, G. V. The Myocardial Toxicity of Carbon Monoxide. Med J Aust 1, 865–868 (1964).
Rajiyah, G. et al. Influence of nicotine on myocardial stiffness and fibrosis during chronic ethanol use. Alcohol Clin Exp Res 20, 985–989 (1996).
Jang, S. Y. et al. Prehypertension and Left Ventricular Diastolic Dysfunction in Middle-Aged Koreans. Korean Circ J 46, 536–541, https://doi.org/10.4070/kcj.2016.46.4.536 (2016).
Brilla, C. G., Funck, R. C. & Rupp, H. Lisinopril-mediated regression of myocardial fibrosis in patients with hypertensive heart disease. Circulation 102, 1388–1393 (2000).
Miki, T., Yuda, S., Kouzu, H. & Miura, T. Diabetic cardiomyopathy: pathophysiology and clinical features. Heart Fail Rev 18, 149–166, https://doi.org/10.1007/s10741-012-9313-3 (2013).
Fein, F. S., Cho, S., Zola, B. E., Miller, B. & Factor, S. M. Cardiac pathology in the hypertensive diabetic rat. Biventricular damage with right ventricular predominance. Am J Pathol 134, 1159–1166 (1989).
Ashrafi, R. et al. Arrhythmogenic gene remodelling in elderly patients with type 2 diabetes with aortic stenosis and normal left ventricular ejection fraction. Exp Physiol 102, 1424–1434, https://doi.org/10.1113/EP086412 (2017).
Matoh, F. et al. Usefulness of delayed enhancement magnetic resonance imaging to differentiate dilated phase of hypertrophic cardiomyopathy and dilated cardiomyopathy. J Card Fail 13, 372–379, https://doi.org/10.1016/j.cardfail.2007.02.001 (2007).
Rahman, M. M. & Laher, I. Structural and functional alteration of blood vessels caused by cigarette smoking: an overview of molecular mechanisms. Curr Vasc Pharmacol 5, 276–292 (2007).
Cacciola, R. R., Guarino, F. & Polosa, R. Relevance of endothelial-haemostatic dysfunction in cigarette smoking. Curr Med Chem 14, 1887–1892 (2007).
Obeidat, M. et al. The Effect of Different Case Definitions of Current Smoking on the Discovery of Smoking-Related Blood Gene Expression Signatures in Chronic Obstructive Pulmonary Disease. Nicotine Tob Res 18, 1903–1909, https://doi.org/10.1093/ntr/ntw129 (2016).
Kotlyar, M., Thuras, P., Hatsukami, D. K. & al’Absi, M. Sex differences in physiological response to the combination of stress and smoking. Int J Psychophysiol 118, 27–31, https://doi.org/10.1016/j.ijpsycho.2017.05.008 (2017).
Nemmar, A. et al. Chronic exposure to water-pipe smoke induces cardiovascular dysfunction in mice. Am J Physiol Heart Circ Physiol 312, H329–H339, https://doi.org/10.1152/ajpheart.00450.2016 (2017).
Yoshida, A. et al. Comparison of perfusion-metabolism mismatch in 99mTc-MIBI and 123I-BMIPP scintigraphy with cardiac magnetic resonance in patients with dilated cardiomyopathy. J Card Fail 19, 445–453, https://doi.org/10.1016/j.cardfail.2013.05.009 (2013).
Lin, L. Y. et al. Conductive channels identified with contrast-enhanced MR imaging predict ventricular tachycardia in systolic heart failure. JACC Cardiovasc Imaging 6, 1152–1159, https://doi.org/10.1016/j.jcmg.2013.05.017 (2013).
Acknowledgements
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2015R1C1A1A02037085, NRF-2014R1A1A1003699, NRF-2017R1A2B3003303) and grants from the Korean Healthcare Technology R&D project funded by the Ministry of Health & Welfare (HI16C0058, HI15C1200).
Author information
Authors and Affiliations
Contributions
J.B.P., B.Y.J. formulated study predictions and study design. H.J.L., J.E.Y., D.G.S., J.M.L., Y.K.K., Y.J.K. contributed to data acquisition and analysis. J.B.P., S.K.K., wrote the main manuscripts text. B.Y.J. Revised the manuscripts. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, J., Lee, HJ., Kim, S.K. et al. Smoking aggravates ventricular arrhythmic events in non-ischemic dilated cardiomyopathy associated with a late gadolinium enhancement in cardiac MRI. Sci Rep 8, 15609 (2018). https://doi.org/10.1038/s41598-018-34145-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-34145-9
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.