Abstract
IL-17C, which is a member of the IL-17 family of cytokines, is preferentially produced by epithelial cells in the lung, skin and colon, suggesting that IL-17C may be involved in not only host defense but also inflammatory diseases in those tissues. In support of that, IL-17C was demonstrated to contribute to development of T cell-dependent imiquimod-induced psoriatic dermatitis and T cell-independent dextran sodium sulfate-induced acute colitis using mice deficient in IL-17C and/or IL-17RE, which is a component of the receptor for IL-17C. However, the roles of IL-17C in other inflammatory diseases remain poorly understood. Therefore, we investigated the contributions of IL-17C to development of certain disease models using Il17c−/− mice, which we newly generated. Those mice showed normal development of T cell-dependent inflammatory diseases such as FITC- and DNFB-induced contact dermatitis/contact hypersensitivity (CHS) and concanavalin A-induced hepatitis, and T cell-independent inflammatory diseases such as bleomycin-induced pulmonary fibrosis, papain-induced airway eosinophilia and LPS-induced airway neutrophilia. On the other hand, those mice were highly resistant to LPS-induced endotoxin shock, indicating that IL-17C is crucial for protection against that immunological reaction. Therefore, IL-17C neutralization may represent a novel therapeutic approach for sepsis, in addition to psoriasis and acute colitis.
Similar content being viewed by others
Introduction
IL-17C is a member of the IL-17 family of cytokines that includes IL-17A, IL-17B, IL-17D, IL-17E/IL-25 and IL-17F. It was originally identified as an IL-17-related cytokine by using EST databases1,2. It is well known that IL-17A and IL-17F are preferentially produced by immune cells such as T cells and group 3 innate lymphoid cells, while IL-17C and IL-25 are predominantly produced by non-immune cells such as colonic and lung epithelial cells3,4,5,6, keratinocytes7,8 and smooth muscle cells9, in mice and/or humans.
IL-17C is known to be important for host defense against such pathogens as Pseudomonas aeruginosa10. On the other hand, inappropriate/excessive IL-17C expression may be involved in development or regulation of various disorders in mice and/or humans. Il17c mRNA was reported to be increased in the inflamed skin from patients with psoriasis7,11 and in anti-TNF-induced psoriasiform skin lesions of patients with Crohn’s disease12. The mRNA for this cytokine is also increased in synovial fluid mononuclear cells from patients with rheumatoid arthritis13, and overexpression of IL-17C in mice resulted in exacerbation of collagen-induced arthritis14. SNPs in Il17re genes, which are components of the receptor for IL-17C3,4, were associated with risk for susceptibility to ulcerative colitis in Germany15. On the other hand, mice deficient in Il17c and Il17re showed aggravated inflammation during dextran sodium sulfate-induced colitis3,4,16, suggesting that IL-17C plays a regulatory role in the setting. Moreover, IL-17C may be involved in development of COPD6, cystic fibrosis6 and atherosclerosis9. IL-17C is also thought to be involved in tumorigenesis: increased expression of Il17c mRNA and IL-17RE protein was observed in lung cancer and hepatocellular carcinoma, respectively17,18, and tumor growth was reduced in Il17c-deficient (Il17c−/−) mice after non-typeable Haemophilus influenza infection17 and in Il17re−/− mice on the Apcmin/+ background19. IL-17C can enhance IL-17A production by Th17 cells, contributing to development of Th17 cell-mediated autoimmune diseases such as experimental autoimmune encephalomyelitis20.
In the present study, we investigated the roles of IL-17C in T cell-dependent diseases such as contact dermatitis and hepatitis, T cell-independent diseases such as pulmonary fibrosis and inflammation, and endotoxin shock using Il17c−/− mice, which we newly generated.
Results
Generation of Il17c −/− mice
Il17c−/− mice were generated from C57BL/6N wild-type mice by replacing the Il17c genes with the neomycin resistance gene, flanked by loxP sequences in C57BL/6 mouse-derived ES cells (Fig. 1a). Il17c−/− mice were born under specific-pathogen-free housing conditions at the expected Mendelian ratio, fertile, and did not show any gross phenotypic abnormalities (data not shown). Expression of Il17c mRNA was detected in various tissues from wild-type mice by quantitative PCR, whereas it was below the limit of detection in tissues from the Il17c−/− mice (Fig. 1b). No apparent abnormalities were found in the proportions of immune cells in the thymus, LNs, spleen and/or bone marrow between the wild-type and Il17c−/− mice (data not shown).
Generation of Il17c−/− mice. (a) IL-17C gene targeting strategy. The region of the Il17c gene containing from exon 1 to exon 3 was replaced with a cassette containing a neomycin resistance gene (Neor), flanked by loxP sequences. (b) Expression of Il17c mRNA in various tissues from wild-type (n = 3) and Il17c−/− (n = 3) mice, determined by qPCR. The data show the mean + SEM.
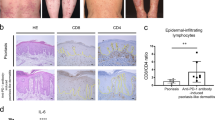
IL-17C is not essential for development of T cell-dependent contact dermatitis
It is known that hapten-induced contact dermatitis/contact hypersensitivity (CHS) is mediated by hapten-specific Th cells21. We found that the thickness of ear skin and severity of skin inflammation (based on histological analysis) were comparable between the Il17c−/− mice and wild-type mice during FITC- and DNFB-induced CHS (Fig. 2a–c). However, mRNA expression for Il17c was increased in the ear skin from the wild-type mice, but not the Il17c−/− mice, after FITC and DNFB challenge (Fig. 3a,b). In addition, mRNA expression for Tnfa and Ccl11 in the skin after FITC challenge and mRNA expression for Ifng and Il6 in the skin after DNFB challenge were reduced in the Il17c−/− mice compared with the wild-type mice (Fig. 3a,b).
Normal development of T cell-dependent contact dermatitis in Il17c−/− mice. (a) Wild-type (n = 18) and Il17c−/− (n = 17) mice were epicutaneously sensitized and challenged with FITC or vehicle alone. The ear skin thickness of the mice was measured at the indicated time points after challenge. (b) Wild-type (n = 15) and Il17c−/− (n = 17) mice were epicutaneously sensitized and challenged with DNFB or vehicle alone. The ear skin thickness of the mice was measured at the indicated time points after challenge. (c) Representative images of skin sections (from 24 hours in (a) and (b)) stained with hematoxylin and eosin. ×100. The data show the mean + SEM (a and b).
Gene expression in the skin, and Ab production in Il17c−/− mice. (a) Relative mRNA expression levels of cytokines and chemokines in the ear skin of wild-type and Il17c−/− mice 24 hours after FITC challenge. V = vehicle treatment. Wild-type mice (vehicle, n = 3; FITC, n = 5) and Il17c−/− mice (vehicle, n = 3; FITC, n = 6). (b) Relative mRNA expression levels of cytokines and chemokines in the ear skin of wild-type and Il17c−/− mice 24 hours after DNFB challenge. V = vehicle treatment. Wild-type mice (vehicle, n = 3; FITC, n = 5) and Il17c−/− mice (vehicle, n = 3; FITC, n = 5). (c) Sera were collected from mice 72 hours after FITC challenge. The levels of FITC-specific Ig subsets in sera were determined by ELISA. N = naïve. Wild-type mice (naive, n = 8; FITC, n = 30) and Il17c−/− mice (naive, n = 4; FITC, n = 32). (d) Sera were collected from mice 72 hours after DNFB challenge. The levels of DNP-specific Ig subsets in sera were determined by ELISA. N = naïve. Wild-type mice (naive, n = 8; DNFB, n = 27) and Il17c−/− mice (naive, n = 5; DNFB, n = 30). The data show the mean + SEM. *p < 0.05, **p < 0.01 and ***p < 0.001: vehicle vs FITC or DNFB; and †p < 0.05 and ††p < 0.01: wild-type mice vs. Il17c−/− mice. Analyses by Mann-Whitney U-test, two-tailed (a, b) and Student’s t-test, two-tailed (c, d). NS = not significant.
The levels of FITC-specific Ig subsets in sera were comparable between the Il17c−/− and wild-type mice during FITC-induced CHS (Fig. 3c), whereas the levels of DNP-specific IgG1 and IgG2a, but not IgG3, in sera were significantly reduced in the Il17c−/− mice compared with the wild-type mice during DNFB-induced CHS (Fig. 3d). These observations suggest that IL-17c is at least partially involved in such immune responses as mRNA expression and Ab production, but is not essential for development of CHS induced by FITC or DNFB.
IL-17C is not required for development of T cell-mediated hepatitis
It is known that Con A-induced hepatitis is accompanied by apoptosis in tissues via Fas on T cells22. After Con A injection, the levels of GOT and GPT activities in sera were comparable in the Il17c−/− and wild-type mice (Fig. 4a). In addition, infiltration of PMNs into the liver was also similarly observed in both groups (Fig. 4b). These observations suggest that IL-17C is not essential for T cell-mediated tissue injury in Con A-induced hepatitis.
Normal development of T cell-dependent hepatitis in Il17c−/− mice. Female mice were injected intravenously with concanavalin A (Con A). 24 hours later, sera and livers were collected. (a) Serum levels of GOT and GPT. Wild-type mice (Saline, n = 4; Con A, n = 5) and Il17c−/− mice (Saline, n = 3; Con A, n = 5). The data show the mean + SEM. NS = not significant. (b) Representative images of liver sections stained with hematoxylin and eosin. Bars = 20 μm.
IL-17C is crucial for suppression of T cell-independent acute colitis
Dextran sodium sulfate (DSS)-induced acute colitis developed even in mice lacking T cells23,24. It was already demonstrated that Il17c−/− mice and Il17re−/− mice showed aggravated development of T cell-independent DSS-induced acute colitis4,16. We confirmed that body weight loss was more severe in the Il17c−/− mice than in the wild-type mice after drinking of water containing DSS (Fig. 5a,b). The length of the colon in Il17c−/− mice was significantly shortened compared with wild-type mice on Day 8 during DSS-induced colitis (Fig. 5c,d). Histological analysis revealed that local inflammation in the colon was more severe in the Il17c−/− mice than in the wild-type mice on Day 8 during DSS-induced colitis (Fig. 5e,f). These observations indicate that IL-17C is crucial for suppression of DSS-induced acute colitis.
High susceptibility of Il17c−/− mice to T cell-independent DSS-induced colitis. Female mice were provided sterile drinking water containing 2.0% DSS ad libitum for 5 days, followed by 15 days of regular drinking water. (a) Change in body weight (%). Wild-type mice (n = 10) and Il17c−/− mice (n = 10). *p < 0.05 and **p < 0.01 vs. corresponding values for Il17c−/− mice. (b) Area under the curve (AUC) for the body weight on Days 5–8 in (a). **p < 0.01. (c)Representative pictures of the animals’ colons on Day 8. (d) Length of colons on the indicated days. Wild-type mice (naïve, n = 4; and Days 8, 15, and 33, n = 4–5) and Il17c−/− mice (naïve, n = 4; and Days 8, 15, and 33, n = 8–10). (e) Representative images of colon sections (Day 8) stained with hematoxylin and eosin. Bars = 100 μm. (f) Histological scores on Day 8. **p < 0.01. The data show the mean + SEM (a,b,d,f).
IL-17C is not essential for development of T cell-independent lung diseases
Constitutive expression of Il17c mRNA was observed in the lungs from wild-type mice, but not Il17c−/− mice (Fig. 1b), suggesting that IL-17C may be involved in lung disease. Therefore, we investigated the role of IL-17C in bleomycin-induced pulmonary fibrosis, which develops independently of T cells25. However, the numbers of eosinophils, neutrophils, macrophages and lymphocytes in BAL fluids were comparable in Il17c−/− and wild-type mice 14 days after intratracheal bleomycin challenge (Fig. 6a). Inflammation and fibrosis based on histological analysis (HE and EVG staining, respectively) were also comparable in the lungs of Il17c−/− and wild-type mice during bleomycin-induced pulmonary fibrosis (Fig. 6b,c), indicating that IL-17C is not essential for development of bleomycin-induced pulmonary fibrosis.
Normal development of T cell-independent pulmonary fibrosis in Il17c−/− mice. Male mice were treated intratracheally with bleomycin (BLM) or PBS. 14 days later, bronchoalveolar lavage (BAL) fluids and the lungs were collected. (a) Cell counts in BAL fluids. Wild-type mice (PBS, n = 5; BLM, n = 9) and Il17c−/− mice (PBS, n = 5; BLM, n = 7). The data show the mean + SEM. **p < 0.01 and ***p < 0.001: PBS vs BLM; and †p < 0.05: wild-type mice vs. Il17c−/− mice. (b,c) Representative images of lung sections. Hematoxylin and eosin staining (b) and Elastica van Gieson staining (c). Bars = 100 μm.
Next, we investigated the role of IL-17C in development of airway eosinophilia induced by inhalation of papain, which is a papaya–derived cysteine and a homologue to house dust mite-derived Der p1 and human cathepsin B26. That eosinophilia induction is mediated by IL-33-stimulated ILC2s and basophils, but not T cells27,28,29,30. After papain inhalation, airway eosinophilia was assessed by the eosinophil count in BAL fluids and was similar in both Il17c−/− and wild-type mice (Fig. 7a). The degree of pulmonary inflammation, based on histological analysis (HE and PAS staining, respectively), was also equivalent in the Il17c−/− and wild-type mice during papain-induced airway eosinophilia (Fig. 7b,c). These observations suggest that IL-17C is not essential for induction of ILC2- and basophil-mediated papain-induced airway eosinophilia.
Normal development of T cell-independent airway eosinophilia in Il17c−/− mice. Mice were treated intratracheally with papain or heat-inactivated papain (HIP). 24 hours after the last challenge, bronchoalveolar lavage (BAL) fluids and the lungs were collected. (a) Cell counts in BAL fluids. Wild-type mice (HIP, n = 10; Papain, n = 21) and Il17c−/− mice (HIP, n = 10; Papain, n = 21). The data show the mean + SEM. **p < 0.01 and ***p < 0.001. (b,c) Representative images of lung sections stained with hematoxylin and eosin (b) and PAS (c). Bars = 50 μm.
Inhalation of LPS in mice resulted in induction of neutrophil-dominant airway inflammation31. In addition, LPS-induced airway neutrophilia developed normally in Rag1−/− mice and Il17a−/− mice31, indicating that it is T cell- and IL-17A-independent. We found that T cell- and IL-17A-independent LPS-induced airway neutrophilia was similar in Il17c−/− mice compared with wild-type mice (Fig. 8a). The levels of IL-6, IL-1β and TNF in the BAL fluids were also comparable between Il17c−/− and wild-type mice after LPS inhalation (Fig. 8b). Although the levels of IL-17A in the BAL fluids were significantly increased in Il17c−/− mice compared with wild-type mice (Fig. 8b), these observations indicate that IL-17C is not essential for T cell- and IL-17A-independent LPS-induced airway neutrophilia.
Normal development of T cell- and IL-17A-independent airway neutrophilia in Il17c−/− mice. Mice were treated intratracheally with LPS or saline. 24 hours later, bronchoalveolar lavage (BAL) fluids were collected. (a)Cell counts in BAL fluids. Wild-type mice (saline, n = 5; LPS, n = 10) and Il17c−/− mice (LPS, n = 5). (b) The levels of cytokines in the BAL fluids in (a). The data show the mean + SEM. ***p < 0.001 vs. wild-type mice.
IL-17C is involved in induction of endotoxin shock
Rag2−/− mice were more highly susceptible to LPS-induced endotoxin shock than wild-type mice, suggesting that T cells, B cells and/or NKT cells play suppressive roles in the setting32. In addition, looking at other members of the IL-17 cytokine family, IL-17A, but not IL-17F or IL-25, was important for LPS-induced endotoxin shock in mice32. However, the contribution of IL-17C to the response remains unclear. We found that the Il17c−/− mice were more resistant to endotoxin shock after intraperitoneal LPS injection compared with the wild-type mice (Fig. 9a). The levels of IL-17C were increased in peritoneal lavage fluids from the wild-type mice, but not the Il17c−/− mice, at 3 and 6 hours after intraperitoneal LPS injection (Fig. 9b). On the other hand, the levels of IL-17A, IL-6, IL-1β, TNF, KC and/or MIP2 were similarly increased in peritoneal lavage fluids of both groups and/or in sera (Fig. 9b and data not shown), suggesting that the effect of IL-17C on LPS-induced endotoxin shock is independent of those cytokines. In addition, the number of inflammatory cells and levels of IL-1β, IL-6, TNF, KC and MIP-2 in the BAL fluids were also identical between both groups in the setting (data not shown).
Strong resistance of Il17c−/− mice to T cell-independent endotoxin shock. Female mice were injected intraperitoneally with LPS. After LPS injection, survival was monitored, and peritoneal fluids were collected at the indicated points. (a) Survival of wild-type (n = 47) and Il17c−/− (n = 46) mice after LPS injection. ***p < 0.001. (b) The concentrations of IL-17C, IL-1β, IL-6, IL-17A and TNF in peritoneal lavage fluids from wild-type mice (0 h, n = 5; 3 h, n = 5; 6 h, n = 6) and Il17c−/− mice (0 h, n = 5; 3 h, n = 5; 6 h, n = 6) were measured by ELISA. The data show the mean + SEM. *p < 0.05: wild-type mice vs. Il17c−/− mice. (c) Peritoneal F4/80− and F4/80+ cells were stimulated with LPS for the indicated times. The expression levels of Il17c and Il17re mRNAs in the cells were determined by quantitative PCR. The data show the mean + SEM (n = 3). (d) The expression levels of Il17c, Il17re, Il1b, Il6, Il17a and Tnfa mRNAs in the tissues and peritoneal lavage fluid cells from wild-type mice at 0, 3 and 6 h after LPS injection were determined by quantitative PCR. The data show the mean + SEM (n = 5). *p < 0.05, **p < 0.01 and ***p < 0.001 vs 0 h (c,d).
Next, we purified F4/80-negative and -positive cells from the peritoneal lavage fluid of naïve wild-type mice and cultured them in the presence and absence of LPS. After LPS stimulation, the expression levels of Il17c and Il17re mRNAs were significantly increased in F4/80+ cells but hardly detectable in F4/80-negative cells (Fig. 9c). However, the level of IL-17C protein in the culture supernatants of F4/80+ cells was below the limit of detection by ELISA (data not shown). In addition, the expression levels of Il17c mRNA were increased in the duodenum, jejunum, ileum and colon, but barely detectable in the peritoneum and peritoneal lavage fluid cells, of wild-type mice after LPS injection (Fig. 8d). On the other hand, Il17re mRNA was constitutively expressed in those tissues/cells, but its level decreased after LPS injection (Fig. 9d). In contrast to Il17c mRNA, expression of mRNA for each of Il1b, Il6, Tnfa and Il17a was increased in peritoneal lavage fluid cells from wild-type mice after LPS injection (Fig. 9d).
To elucidate the contribution of macrophage-derived IL-17C to macrophage activation, we cultured M-CSF-induced bone marrow cell-derived macrophages (BMMϕ) from wild-type and Il17c−/− mice in the presence of LPS. The levels of IL-1β, IL-6 and TNF in the culture supernatants were similar between the two cell populations in the setting (data not shown). In addition, when peritoneal F4/80+ cells of wild-type mice were stimulated with LPS in the presence of recombinant IL-17C, LPS-mediated IL-1β, IL-6 and TNF productions were not affected (data not shown). These observations suggest that cells of the gut other than peritoneal F4/80+ cells are producers of and responders to IL-17C during LPS-induced endotoxin shock.
Discussion
IL-17C is preferentially produced by non-immune cells such as colonic and lung epithelial cells3,4,5,6, keratinocytes7,8 and smooth muscle cells9, in mice and/or humans. It is known to enhance IL-17A production by Th17 cells, contributing to development of Th17 cell-mediated experimental autoimmune encephalomyelitis20. In the present study, we used Il17c−/− mice to investigate the roles of IL-17C in T cell-dependent and -independent diseases.
We demonstrated that Il17c mRNA was constitutively expressed in the skin of mice (Fig. 1b), suggesting that IL-17C may be involved in host defense via the skin and/or in development of certain skin diseases. In support of that, Il17c mRNA was increased in inflamed skin from patients with psoriasis7,11. Moreover, Il17c−/− and Il17re−/− mice showed decreased development of imiquimod-induced psoriatic dermatitis4, which is mediated by IL-17-producing γδ T cells and ILC3, but not Th17 cells33.
Since IL-17C can enhance IL-17A production by Th17 cells20, we examined for involvement of IL-17C in development of allergic dermatitis, such as hapten-induced CHS, which is mediated by hapten-specific Th17 cells21,34. Indeed, we found that Il17c mRNA expression was increased in the inflamed skin of wild-type mice during FITC- and DNFB-induced CHS (Figs 2 and 3). Although mRNA expression for several cytokines and/or chemokines was reduced in the inflamed skin during FITC- and/or DNFB-induced CHS (Figs 2 and 3), Il17c−/− mice showed normal development of FITC- or DNFB-induced CHS.
We previously reported that Il17a−/− mice showed impaired DNFB-induced CHS34. Although IL-17A-heterozygous (Il17a+/−) mice show half–levels of IL-17A production compared with wild-type mice, the development of certain allergic diseases, including CHS, in Il17a+/− mice was similar to in wild-type mice. These observations suggest that even the apparently reduced levels of IL-17A are sufficient to fully induce the inflammation of CHS in Il17a+/− mice. We also found that Il17c−/− mice showed reduced hapten-specific IgG1 and IgG2a production during DNFB-induced CHS. However, it was reported that B cell-deficient mice showed normal development of DNFB-induced CHS35. These observations suggest that although the deficiency of IL-17C resulted in reduced, but not completely abrogated, mRNA expression for certain cytokines and chemokines and Ab production, even the reduced mRNA levels may be sufficient for induction of inflammation. The levels of Il1b mRNA expression were comparable between the Il17c−/− mice and wild-type mice during FITC- and DNFB-induced CHS (Fig. 3a,b). On the other hand, the levels of Il1b mRNA expression were reduced in the vehicle-treated skin of Il17c−/− mice compared with the wild-type mice during FITC-, but not DNFB-, induced CHS (Fig. 3a,b). Those differences may have been caused by the different chemicals used to prepare the vehicles: FITC was dissolved in a mixture of dibutylphathalate and acetone, whereas DNFB was dissolved in a mixture of olive oil and acetone. Dibutylphathalate is known to be an irritant that can induce IL-1β-dependent activation of immune cells36,37. Therefore, although IL-17C seemed to be important for induction of Il1b mRNA expression in response to the irritant effect of dibutylphathalate, this cytokine is not essential for induction of Il1b mRNA expression in the elicitation phase of FITC-induced CHS. Thus, unlike the case of imiquimod-induced psoriatic dermatitis4, IL-17C is not essential for development of FITC- or DNFB-induced CHS. These observations suggest that IL-17C may be involved in IL-17-producing γδ T cell- and ILC3-mediated immune responses, rather than Th17 cell- and Tc17 cell-mediated immune responses, in the skin.
Moreover, it is known that liver injury during Con A-induced hepatitis is mediated by Fas on Tc cells22, and IL-17A is involved in the setting38,39,40. We demonstrated that Con A-induced hepatitis developed normally in Il17c−/− mice, indicating that IL-17C is not essential for that development (Fig. 4). It was recently reported that Con A-induced hepatitis was milder in Il17c−/− mice41. However, even when we used those authors’ experimental protocol, we found that Con A-induced hepatitis developed similarly in Il17c−/− mice to in wild-type mice (data not shown). A similar discrepancy was also observed in Il17c−/− mice during Candida albicans infection: Conti et al. reported that IL-17C was dispensable for host defense against Candida albicans42, whereas Huang et al. reported that IL-17C was important for that defense43.
The Il17c−/− mice in the paper by Huang et al. were originally generated by using 129/TC1 ES cells, as they previously described20. In that earlier report20, the authors used C57BL/6 mice obtained from Jackson Laboratories. Although they did not describe how many times the Il17c−/− mice on the 129/TC1 background were backcrossed with “C57BL/6J mice”, we presume that their mice must be on the “C57BL/6J background”. On the other hand, our Il17c−/− mice were generated by using C57BL/6 ES cells and are on the “C57BL/6N” background. The susceptibility of mice to Con A-induced hepatitis was reported to be affected by their genetic background44. In addition, the intestinal microbiota, which affect immune responses, are different between C57BL/6J and C57BL/6N mice45. Moreover, susceptibility to Con A-induced hepatitis is influenced by the intestinal microbiota46,47. The apparent discrepancy between their and our results may be due to the different genetic backgrounds and/or housing environments of the mice.
Il17c mRNA was constitutively expressed in the lungs of mice (Fig. 1b), and lung epithelial cells are known to produce IL-17C, suggesting that IL-17C may be involved in host defense via the lungs and/or in development of certain pulmonary diseases such as COPD and cystic fibrosis6. Il17a−/− mice showed reduced bleomycin-induced pulmonary fibrosis48, and it was suggested that Th17 cell- and γδ T cell-, but not iNKT cell-, derived IL-17A is important in those settings48,49,50. However, since bleomycin-induced pulmonary fibrosis is known to develop normally in T/B cell-deficient scid/scid mice25, IL-17A produced by non-immune/immune cells other than T cells may be crucial for that. Thus, it was not essential for development of bleomycin-induced pulmonary fibrosis (Fig. 6), although we expected IL-17C to contribute to development of T cell-independent IL-17A-mediated bleomycin-induced pulmonary fibrosis.
Like IL-17A, IL-17C is known to be involved in recruitment of neutrophils into local inflammatory sites2,4,10,17. Indeed, it was shown that IL-17A-mediated IL-17C expression by alveolar epithelial cells is important for recruitment of neutrophils by inducing IL-6 and neutrophil chemoattractants such as KC and MIP-2 in the lungs during Pseudomonas aeruginosa infection10. In contrast, we found that IL-17C is not essential for recruitment of neutrophils or production of cytokines (IL-1β, IL-6 and TNF) and chemokines (KC and MIP-2) in the lungs of mice after LPS inhalation (Fig. 8). Airway neutrophilia during Pseudomonas aeruginosa infection is dependent on IL-17A10, which is produced at least in part by Th17 cells51, whereas LPS-induced airway neutrophilia is independent of IL-17A and T cells31. Thus, IL-17C may be important for IL-17A-dependent, but not -independent, airway neutrophilia.
Rag2−/− mice were highly susceptible, but Il17a−/− mice were resistant, to LPS-induced endotoxin shock compared with wild-type mice32, suggesting that IL-17A produced by other non-immune/immune cells besides T and NKT cells is crucial for protection against LPS-induced endotoxin shock. Like Il17a−/− mice32, we found that Il17c−/− mice were resistant to T cell-independent IL-17A-mediated LPS-induced endotoxin shock, without any effect on production of IL-17A as well as other proinflammatory cytokines such as IL-1β, IL-6 and TNF (Fig. 9). Those findings suggest that IL-17C is crucial for protection against LPS-induced endotoxin shock, independently of IL-17A, IL-1β, IL-6 and TNF.
Taken all together, our observations indicate that IL-17C is not essential for development of T cell-dependent FITC- or DNFB-induced CHS or Con A-induced hepatitis. On the other hand, IL-17C is important for development of T cell-independent DSS-induced colitis and LPS-induced endotoxin shock, but not for bleomycin-induced pulmonary fibrosis, papain-induced airway eosinophilia or LPS-induced airway neutrophilia.
Methods
Mice
C57BL/6N wild-type mice were obtained from Japan SLC, Inc. Il17c−/− mice on the C57BL/6N background were generated as follows. The Il17 gene was disrupted by replacement of the region from exon 1 to exon 3 with a neomycin resistance gene, flanked by loxP sequences (Fig. 1a). Homologous regions were amplified by PCR using the following primers: 5′-AGTAACAACAGATACACCGCCACC-3′ and 5′-AACAGGTGAAGCCTGGCTGTGTGC-3′ to generate a 8-kb fragment, and 5′-TCCAGGACAGACATTCCAGGCACC-3′ and 5′-TAGGGACAGTAAGCAGCTTCAACC-3′ to generate a 1.5-kb fragment. The targeting vector was electroporated into C57BL/6N ES cells (EGR-101, kindly provided by Dr. Masaru Okabe, Osaka University). Male chimeric mice were obtained from two distinct targeted clones and mated with C57BL/6N female mice. Genotyping of Il17c−/− mice was performed by PCR using the following primers: common (5′-CACAAGGCAAAGGCTGGGCATAGC-3′), WT (5′-CCAGCCCACCGAGCTCCGAGCTGC-3′) and MT (5′-GGAAGACAATAGCAGGCATGCTGG-3′). The common and WT primers were used for detection of wild-type alleles (~510 bp), and the common and MT primers were used for detection of mutant alleles (~270 bp). All mice were housed in a specific-pathogen-free environment at The Institute of Medical Science, The University of Tokyo. The animal protocols for experiments were approved by the Institutional Review Board of the Institute (A11-28 and A14-10), and all experiments were conducted according to the ethical and safety guidelines of the Institute.
Quantitative PCR
Total RNA was prepared from tissues using Sepasol (Nacalai Tesque, Inc.) and treated with DNase (TURBO DNA-free-kit; Thermo Fisher Scientific Inc.). cDNA was synthesized from the isolated RNA by RT-PCR (PrimeScript RT Reagent kit; TAKARA BIO Inc.) or ReverTra Ace qPCR (RT Master Mix with gDNA; TOYOBO CO.). Quantitative real-time PCR was performed with SYBER Premix Ex Taq (TAKARA BIO Inc.) or THUNDERBIRD SYBR qPCR Mix (TOYOBO CO.) using a CFX384TM Touch Real-time PCR Detection System (BioRad Laboratories, Inc.). Relative gene expression was determined against the expression levels of 18s rRNA (Fig. 1b) and Gapdh mRNA (other experiments). The designed primers are shown in Table 1.
Dextran sodium sulfate (DSS)-induced colitis
Mice were provided sterile drinking water containing 2% DSS (MW = 36,000-50,000; MP Biomedicals) ad libitum for 5 days, followed by 15 days of plain drinking water27. Each animal’s body weight was monitored daily. Histological scores were determined as described elsewhere27.
Contact hypersensitivity (CHS)
FITC- and DNFB-induced CHS and measurement of FITC-specific and DNP-specific serum Igs were performed as described elsewhere27.
Bleomycin-induced pulmonary fibrosis
Mice were treated intratracheally with 2 mg/kg bleomycin (NIPPON KAYAKU CO.) or an equal volume of PBS as a control. Fourteen days later, bronchoalveolar lavage (BAL) fluids were collected. The total cell counts and leukocyte profiles were determined with a hemocytometer (XT-1800i; Sysmex), as described previously27.
Papain-induced airway inflammation
Papain-induced airway inflammation was generated as described elsewhere27,30. Twenty-four hours after the last inhalation of papain, BAL fluids were collected, and the total cell counts and leukocyte profiles were determined with a hemocytometer (XT-1800i; Sysmex), as above.
LPS-induced airway inflammation
LPS-induced airway inflammation was established as described elsewhere31. In brief, mice were treated intratracheally with 20 μl of 0.5 mg/ml LPS (Escherichia coli serotype 0111:B4; Sigma–Aldrich) or an equal volume of saline as a control. Twenty-four hours after the last inhalation of LPS or saline, BAL fluids were collected, and the total cell counts and leukocyte profiles were determined as described above.
Concanavalin A (Con A)-induced hepatitis
Con A-induced hepatitis was generated as described elsewhere27. Fourteen hours after the injection of Con A, sera were collected, and the levels of GOT and GPT in the sera were determined using Transaminase CII-test Wako (Wako).
LPS-induced endotoxin shock
Mice were intraperitoneally injected with 15 mg/kg of LPS (Escherichia coli serotype 0111:B4; Sigma–Aldrich) as described elsewhere27,32. After LPS injection, the survival of the mice was monitored. Peritoneal cells and fluids were collected at 0, 3 and 6 hours after LPS injection, as described elsewhere32.
ELISA for cytokines
The concentrations of IL-1β, IL-6, IL-17A, TNF, KC and MIP-2 were determined using ELISA kits (eBioscience, Biolegend or PeproTech), according to the manufacturers’ instructions. For IL-17C detection, plates (Nunc) for ELISA were coated with rat anti-mouse IL-17C mAb (MAB2306; R&D Systems; 2 μg/ml in PBS) as a capture Ab at room temperature overnight. After blocking with 1x Assay Diluent (BioLegend), samples and recombinant mouse IL-17C (R&D Systems) as a standard cytokine were applied to the wells, and the plates were incubated at 4 °C overnight. After washing the wells, goat anti-mouse IL-17C polyclonal Ab (AF2306; R&D Systems; 1.6 μg/ml in 1x Assay Diluent), as a detection Ab, was applied to the wells, followed by incubation at room temperature for 1 hour. After washing the wells, HRP-conjugated donkey anti-goat IgG (V805A; Promega; 1 μg/ml in 1x Assay Diluent) was added to the wells, followed by incubation at room temperature for 30 min. Tetramethylbenzidine solution (Nacalai Tesque) was used as the substrate. The reaction was stopped by adding 0.17 M sulfuric acid, and the OD450 was measured using a plate reader (VersaMax; Molecular Devices).
Peritoneal cell culture
Peritoneal lavage fluid cells were collected from naïve wild-type mice. The cells were incubated with anti-CD16/CD32 mAb (93; eBioscience) in HBSS containing 2% FCS for 15 min at 4 °C, and then with biotinylated anti-mouse F4/80 mAb (BM8, BioLegend) for 25 min at 4 °C. After washing, the cells were incubated with streptavidin-beads (Miltenyi Biotec) for 15 min at 4 °C. After washing, F4/80-negative and -positive cells were separated using a MACS system (Miltenyi Biotec). The F4/80-negative and -positive cells were cultured in AIM V Medium (GIBCO) supplemented with AlbuMAX Supplement (GIBCO) in the presence of 2 μg/ml LPS for 0, 3, 6, 12 and 24 h at 37 °C. The cells were collected, and the total RNA of the cells was prepared as described above.
Histology
Tissues were fixed in Carnoy’s solution and embedded in paraffin. Then sections were prepared and stained using hematoxylin and eosin, periodic acid-Schiff (PAS) or Elastica van Gieson (EVG) staining methods.
Statistics
The Mann-Whitney U test, two-tailed (for quantitative PCR analysis), a Kaplan–Meier method (for survival) and a two-tailed, unpaired Student’s t-test (for other experiments) were applied to test for statistical significance using Graphpad Prism software (Graphpad Prism). P values of less than 0.05 were considered statistically significant.
References
Li, H. et al. Cloning and characterization of IL-17B and IL-17C, two new members of the IL-17 cytokine family. Proc Natl Acad Sci USA 97, 773–778 (2000).
Hurst, S. D. et al. New IL-17 family members promote Th1 or Th2 responses in the lung: in vivo function of the novel cytokine IL-25. J Immunol 169, 443–453 (2002).
Song, X. et al. IL-17RE is the functional receptor for IL-17C and mediates mucosal immunity to infection with intestinal pathogens. Nat Immunol 12, 1151–1158, https://doi.org/10.1038/ni.2155 (2011).
Ramirez-Carrozzi, V. et al. IL-17C regulates the innate immune function of epithelial cells in an autocrine manner. Nat Immunol 12, 1159–1166, https://doi.org/10.1038/ni.2156 (2011).
Im, E., Jung, J. & Rhee, S. H. Toll-like receptor 5 engagement induces interleukin-17C expression in intestinal epithelial cells. J Interferon Cytokine Res 32, 583–591, https://doi.org/10.1089/jir.2012.0053 (2012).
Pfeifer, P. et al. IL-17C is a mediator of respiratory epithelial innate immune response. Am J Respir Cell Mol Biol 48, 415–421, https://doi.org/10.1165/rcmb.2012-0232OC (2013).
Johansen, C. et al. Characterization of the interleukin-17 isoforms and receptors in lesional psoriatic skin. Br J Dermatol 160, 319–324, https://doi.org/10.1111/j.1365-2133.2008.08902.x (2009).
Johansen, C., Riis, J. L., Gedebjerg, A., Kragballe, K. & Iversen, L. Tumor necrosis factor alpha-mediated induction of interleukin 17C in human keratinocytes is controlled by nuclear factor kappaB. J Biol Chem 286, 25487–25494, https://doi.org/10.1074/jbc.M111.240671 (2011).
Butcher, M. J., Waseem, T. C. & Galkina, E. V. Smooth Muscle Cell-Derived Interleukin-17C Plays an Atherogenic Role via the Recruitment of Proinflammatory Interleukin-17A + T Cells to the Aorta. Arterioscler Thromb Vasc Biol 36, 1496–1506, https://doi.org/10.1161/ATVBAHA.116.307892 (2016).
Wolf, L. et al. IL-17A-mediated expression of epithelial IL-17C promotes inflammation during acute Pseudomonas aeruginosa pneumonia. Am J Physiol Lung Cell Mol Physiol 311, L1015–L1022, https://doi.org/10.1152/ajplung.00158.2016 (2016).
Johnston, A. et al. Keratinocyte overexpression of IL-17C promotes psoriasiform skin inflammation. J Immunol 190, 2252–2262, https://doi.org/10.4049/jimmunol.1201505 (2013).
Friedrich, M., Tillack, C., Wollenberg, A., Schauber, J. & Brand, S. IL-36g sustains a proinflammatory self-amplifying loop with IL-17C in anti-TNF-induced psoriasiform skin lesions of patients with Crohn’s disease. Inflamm Bowel Dis 20, 1891–1901, https://doi.org/10.1097/MIB.0000000000000198 (2014).
Hwang, S. Y. & Kim, H. Y. Expression of IL-17 homologs and their receptors in the synovial cells of rheumatoid arthritis patients. Mol Cells 19, 180–184 (2005).
Yamaguchi, Y. et al. IL-17B and IL-17C are associated with TNF-alpha production and contribute to the exacerbation of inflammatory arthritis. J Immunol 179, 7128–7136 (2007).
Franke, A. et al. Genome-wide association study for ulcerative colitis identifies risk loci at 7q22 and 22q13 (IL17REL). Nat Genet 42, 292–294, https://doi.org/10.1038/ng.553 (2010).
Reynolds, J. M. et al. Regulation of intestinal inflammation and barrier function by IL-17C. J Immunol 189, 4226–4230, https://doi.org/10.4049/jimmunol.1103014 (2012).
Jungnickel, C. et al. IL-17C mediates the recruitment of tumor-associated neutrophils and lung tumor growth. Oncogene 36, 4182–4190, https://doi.org/10.1038/onc.2017.28 (2017).
Liao, R. et al. High expression of IL-17 and IL-17RE associate with poor prognosis of hepatocellular carcinoma. J Exp Clin Cancer Res 32, 3, https://doi.org/10.1186/1756-9966-32-3 (2013).
Song, X. et al. Alterations in the microbiota drive interleukin-17C production from intestinal epithelial cells to promote tumorigenesis. Immunity 40, 140–152, https://doi.org/10.1016/j.immuni.2013.11.018 (2014).
Chang, S. H. et al. Interleukin-17C promotes Th17 cell responses and autoimmune disease via interleukin-17receptor E. Immunity 35, 611–621, https://doi.org/10.1016/j.immuni.2011.09.010 (2011).
Iwakura, Y., Nakae, S., Saijo, S. & Ishigame, H. The roles of IL-17A in inflammatory immune responses and host defense against pathogens. Immunol Rev 226, 57–79, https://doi.org/10.1111/j.1600-065X.2008.00699.x (2008).
Seino, K. et al. Contribution of Fas ligand to T cell-mediated hepatic injury in mice. Gastroenterology 113, 1315–1322 (1997).
Axelsson, L. G., Landstrom, E., Goldschmidt, T. J., Gronberg, A. & Bylund-Fellenius, A. C. Dextran sulfate sodium (DSS) induced experimental colitis in immunodeficient mice: effects in CD4(+) -cell depleted, athymic and NK-cell depleted SCID mice. Inflamm Res 45, 181–191 (1996).
Schippers, A. et al. b7-Integrin exacerbates experimental DSS-induced colitis in mice by directing inflammatory monocytes into the colon. Mucosal Immunol 9, 527–538, https://doi.org/10.1038/mi.2015.82 (2016).
Helene, M. et al. T cell independence of bleomycin-induced pulmonary fibrosis. J Leukoc Biol. 65, 187–195 (1999).
Chua, K. Y. et al. Sequence analysis of cDNA coding for a major house dust mite allergen, Der p 1. Homology with cysteine proteases. J Exp Med 167, 175–182 (1988).
Oboki, K. et al. IL-33 is a crucial amplifier of innate rather than acquired immunity. Proc Natl Acad Sci USA 107, 18581–18586, https://doi.org/10.1073/pnas.1003059107 (2010).
Halim, T. Y., Krauss, R. H., Sun, A. C. & Takei, F. Lung natural helper cells are a critical source of Th2 cell-type cytokines in protease allergen-induced airway inflammation. Immunity 36, 451–463, https://doi.org/10.1016/j.immuni.2011.12.020 (2012).
Motomura, Y. et al. Basophil-derived interleukin-4 controls the function of natural helper cells, a member of ILC2s, in lung inflammation. Immunity 40, 758–771, https://doi.org/10.1016/j.immuni.2014.04.013 (2014).
Morita, H. et al. An Interleukin-33-Mast Cell-Interleukin-2 Axis Suppresses Papain-Induced Allergic Inflammation by Promoting Regulatory T Cell Numbers. Immunity 43, 175–186, https://doi.org/10.1016/j.immuni.2015.06.021 (2015).
Nakae, S., Suto, H., Berry, G. J. & Galli, S. J. Mast cell-derived TNF can promote Th17 cell-dependent neutrophil recruitment in ovalbumin-challenged OTII mice. Blood 109, 3640–3648, https://doi.org/10.1182/blood-2006-09-046128 (2007).
Shimura, E. et al. Potential role of myeloid cell/eosinophil-derived IL-17 in LPS-induced endotoxin shock. Biochem Biophys Res Commun 453, 1–6, https://doi.org/10.1016/j.bbrc.2014.09.004 (2014).
Pantelyushin, S. et al. Rorgammat + innate lymphocytes and gammadelta T cells initiate psoriasiform plaque formation in mice. J Clin Invest 122, 2252–2256, https://doi.org/10.1172/JCI61862 (2012).
Nakae, S. et al. Antigen-specific T cell sensitization is impaired in IL-17-deficient mice, causing suppression of allergic cellular and humoral responses. Immunity 17, 375–387 (2002).
Gorbachev, A. V. & Fairchild, R. L. CD40 engagement enhances antigen-presenting langerhans cell priming of IFN-gamma-producing CD4 + and CD8 + T cells independently of IL-12. J Immunol 173, 2443–2452 (2004).
Chun, K. H., Imai, Y., Higashi, N. & Irimura, T. Migration of dermal cells expressing a macrophage C-type lectin during the sensitization phase of delayed-type hypersensitivity. J Leukoc Biol 68, 471–478 (2000).
Chun, K. H., Imai, Y., Higashi, N. & Irimura, T. Involvement of cytokines in the skin-to-lymph node trafficking of cells of the monocyte-macrophage lineage expressing a C-type lectin. Int Immunol 12, 1695–1703 (2000).
Diao, H. et al. Osteopontin regulates interleukin-17 production in hepatitis. Cytokine 60, 129–137, https://doi.org/10.1016/j.cyto.2012.06.287 (2012).
Nagata, T. et al. Requirement of IL-17RA in Con A induced hepatitis and negative regulation of IL-17 production in mouse T cells. J Immunol 181, 7473–7479 (2008).
Xu, M. et al. Regulation of the development of acute hepatitis by IL-23 through IL-22 and IL-17 production. Eur J Immunol 41, 2828–2839, https://doi.org/10.1002/eji.201141291 (2011).
Huang, J. et al. IL-17C/IL-17RE Augments T Cell Function in Autoimmune Hepatitis. J Immunol 198, 669–680, https://doi.org/10.4049/jimmunol.1600977 (2017).
Conti, H. R. et al. Signaling through IL-17C/IL-17RE is dispensable for immunity to systemic, oral and cutaneous candidiasis. PLoS One 10, e0122807, https://doi.org/10.1371/journal.pone.0122807 (2015).
Huang, J. et al. IL-17C is required for lethal inflammation during systemic fungal infection. Cell Mol Immunol 13, 474–483, https://doi.org/10.1038/cmi.2015.56 (2016).
Habu, Y. et al. Mice deficient in Vbeta8 + NKT cells are resistant to experimental hepatitis but are partially susceptible to generalised Shwartzman reaction. Clin Exp Med 7, 30–38, https://doi.org/10.1007/s10238-007-0122-2 (2007).
Ivanov, I. I. et al. Induction of intestinal Th17 cells by segmented filamentous bacteria. Cell 139, 485–498, https://doi.org/10.1016/j.cell.2009.09.033 (2009).
Kajiya, M. et al. Hydrogen from intestinal bacteria is protective for Concanavalin A-induced hepatitis. Biochem Biophys Res Commun 386, 316–321, https://doi.org/10.1016/j.bbrc.2009.06.024 (2009).
Cai, W., Ran, Y., Li, Y., Wang, B. & Zhou, L. Intestinal microbiome and permeability in patients with autoimmune hepatitis. Best Pract Res Clin Gastroenterol 31, 669–673, https://doi.org/10.1016/j.bpg.2017.09.013 (2017).
Wilson, M. S. et al. Bleomycin and IL-1b-mediated pulmonary fibrosis is IL-17A dependent. J Exp Med 207, 535–552, https://doi.org/10.1084/jem.20092121 (2010).
Braun, R. K. et al. IL-17 producing gammadelta T cells are required for a controlled inflammatory response after bleomycin-induced lung injury. Inflammation 31, 167–179, https://doi.org/10.1007/s10753-008-9062-6 (2008).
Gasse, P. et al. IL-1 and IL-23 mediate early IL-17A production in pulmonary inflammation leading to late fibrosis. PLoS One 6, e23185, https://doi.org/10.1371/journal.pone.0023185 (2011).
Liu, J. et al. Early production of IL-17 protects against acute pulmonary Pseudomonas aeruginosa infection in mice. FEMS Immunol Med Microbiol 61, 179–188, https://doi.org/10.1111/j.1574-695X.2010.00764.x (2011).
Acknowledgements
We thank Masako Fujiwara and Yoshiko Shimamoto for their skilled technical assistance. We also thank Lawrence W. Stiver (Quality Translation Co., Ltd.; Tokyo, Japan; qualityt@gol.com) for his critical reading of the manuscript. This work was supported by Grants-in-Aid for Scientific Research (B) (S. Nakae) from the Ministry of Education, Culture, Sports, Science and Technology, Japan and a grant from Precursory Research for Embryonic Science and Technology, Japan Science and Technology Agency (S. Nakae.).
Author information
Authors and Affiliations
Contributions
S.Y., A.N. and S. Nakae designed the experiments. S.Y., A.N., T.N., T.Y., E.S., Y.H., K.A., S. Narushima and H.M. performed the experiments. A.N., S.Y., K.S. and S. Nakae generated the Il17c−/− mice. K.M. and I.H. provided resources. S.Y., I.H. and S.N. wrote the manuscript. All authors reviewed the article.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yamaguchi, S., Nambu, A., Numata, T. et al. The roles of IL-17C in T cell-dependent and -independent inflammatory diseases. Sci Rep 8, 15750 (2018). https://doi.org/10.1038/s41598-018-34054-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-34054-x
Keywords
This article is cited by
-
Role of IL-17 family cytokines in the progression of IPF from inflammation to fibrosis
Military Medical Research (2022)
-
The role of unconventional T cells in COVID-19
Irish Journal of Medical Science (1971 -) (2022)
-
The IL-17 receptor IL-17RE mediates polyIC-induced exacerbation of experimental allergic asthma
Respiratory Research (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.