Abstract
Helix B surface peptide (HBSP) is an erythropoietin (EPO)-derived peptide that protects tissue from the risks of elevated blood pressure and thrombosis. This study focused on the protection of HBSP in hepatic ischaemia/reperfusion (I/R) by enhancing the level of autophagy. In detail, we randomly divided C57BL/6 mice into sham-operated, hepatic ischaemia/reperfusion (I/R), I/R + HBSP, I/R + HBSP + 3-methyladenine (autophagy inhibitor), I/R + HBSP + rapamycin (mTOR inhibitor), and I/R + HBSP + Ly294002 (Akt inhibitor) groups. We assessed alanine aminotransferase (ALT), aspartate aminotransferase (AST) and lactate dehydrogenase (LDH) levels in mouse sera, and performed haematoxylin/eosin (HE) staining, immunohistochemistry, electron microscopy, immunofluorescence microscopy, and western blotting on liver tissue to detect the degree of liver injury, liver apoptosis, autophagy, and the expression of microtubule associated protein 1 light chain 3 alpha (Map1lc3, or LC3), Beclin 1, phospho-mTOR, mTOR, phospho-Akt (P-Akt), and Akt. HBSP relieved hepatic I/R injury in a concentration-independent manner. The expression of LC3II, LC3I, and Beclin 1, and the formation of autophagosomes, in the I/R + HBSP group were higher than those in the I/R group. The protective effects of HBSP were abolished by 3-methyladenine and, to a lesser extent, Ly294002, but enhanced by rapamycin. Furthermore, In vivo, HBSP also protected against hypoxia injury induced by cobalt chloride (CoCl2) through improving the level of autophagy. Therefore, HBSP protected against hepatic I/R injury, mainly via regulating autophagy by targeting mTOR.
Similar content being viewed by others
Introduction
A large number of literatures have confirmed that Erythropoietin (EPO) has tissue protection and erythropoiesis. The erythropoietic effect of EPO has the risk of causing hypertension and thrombosis, which limits its application1,2. Erythropoietin (EPO) helix B surface peptide (HBSP) is a peptide derived from the 11-amino acid sequence of the waterborne surface of helix B in the tertiary structure of the EPO molecule3, as a derivative of EPO, retains the tissue protective effect of EPO and removes its role in erythropoiesis. As HBSP does not interact with Epor24, unlike EPO, it does not promote the production of red blood cell5. Thus, it is not associated with the side effects of thrombosis and hypertension. HBSP plays a broad role in protecting tissues from injury6, as observed in the mouse kidney ischaemia/reperfusion (I/R) model7, a rabbit coronary atherosclerotic model8, and rat dilated cardiomyopathy9. HBSP mediates tissue protection by inhibiting inflammation and apoptosis during organ I/R injury5,7. It has several advantages over EPO as a tissue damage protection agent. However, its effects and potential mechanism in the liver have not been reported.
Hepatic I/R injury is a common cause of liver injury, especially during liver transplantation. The pathophysiology of liver I/R injury includes hypoxia-induced cell damage and inflammatory pathway activation caused by delayed disorders and injuries10,11,12,13,14,15. Recent studies have shown that autophagy is involved in major areas of liver disease. Since autophagy was first recognized due to its role during starvation, the study of autophagy in liver disease has focused on hepatic I/R injury13, during which it renders cells more effective in response to nutritional deficits and hypoxia. Autophagy is the main pathway for intracellular protein degradation. Autophagosomes fuse to lysosomes, then degrade intracellular longevity proteins and organelles to maintain nutrient stability under starvation or stress conditions, and to remove harmful cellular components16,17,18,19. Recently, a large number of studies have confirmed the protective role of autophagy in the kidney, lower limbs, myocardium, nerve tissue of multiple organs, and tissue affected by I/R injury20,21,22,23, but its role in the liver is still not clear24. Despite on-going research, it is also unclear how HBSP regulates autophagy to protect the liver from I/R injury. In this study, we uncovered the mechanism of HBSP protecting hepatic I/R injury.
Result
HBSP reduces liver I/R injury independent of concentration
Firstly, we observed the pathological changes in liver tissue. We found that the sham operation group showed normal liver tissue morphology, whereas the liver tissue in the I/R group had obvious inflammatory cell infiltration, haemorrhagic-induced changes, and a loss of tissue integrity. On the contrary, the degree of liver tissue damage was significantly reduced in the I/R + HBSP groups than that in I/R group, at all HBSP concentrations, and the inflammatory cell infiltration was decreased compared to in the I/R alone group (Fig. 1A). In addition, the ALT, AST and LDH levels in the I/R group were significantly increased over those in the sham group, whereas the levels of ALT and AST in the HBSP group were significantly relieved compared to those in the I/R group (Fig. 1B). These results suggest that HBSP significantly reduces I/R-induced liver injury independent of HBSP concentration.
HBSP can significantly reduce I/R-induced liver injury in a concentration-independent manner. (A) Representative photographs (200×) of haematoxylin–eosin-stained liver sections from sham-operated, I/R, and I/R + HBSP mice. HBSP was injected into mice at the indicated concentrations. Scar bar, 50 μm. (B) Histopathological scoring of hepatic injury was performed. (C) Serum ALT/AST levels in sham, I/R, and HBSP-injected mice. *Significant difference from I/R group, **p < 0.01, ***p < 0.001; NS: Not statistically significant
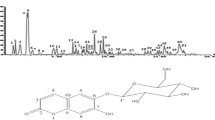
HBSP enhances autophagy in response to hepatic I/R injury
Autophagy is accompanied by lipidation of microtubule associated protein 1 light chain 3 alpha (Map1lc3A, or LC3). Lipidation increases the expression of Beclin 1 and autophagosome formation25. Therefore, in this study, we assessed autophagy using the ratio of LC3II:LC3I, Beclin1 expression, and autophagosome formation. The ratio of LC3II:LC3I and the expression of Beclin1 were significantly higher in the HBSP group than those in the I/R group (Fig. 2B), and the number of autophagosome in the HBSP group was significantly higher than that in the I/R group (Fig. 2A).
HBSP enhances autophagy during hepatic I/R injury. (A) Representative electron micrographs of autophagosomes. Scar bar, 1 μm. (B) Quantification of autophagosomes under EM. (C) Representative images of immunoblots for LC3I, LC3II, Beclin1, and β-actin (full-length blots are presented in the Supplementary Information file). **p < 0.01, compared to the I/R group.
Inhibition of autophagy reverses the effects of HBSP in hepatic I/R injury
The compound 3-methyladenine (3-MA) is commonly used as an autophagy inhibitor26. We found decreases in the LC3II:LC3I ratio and Beclin1 expression in the 3-MA group compared to the HBSP group (Fig. 3A). We also found that 3-MA increased the infiltration of inflammatory cells in the presence of HBSP and caused more severe liver damage than HBSP alone (Fig. 3B). In addition, the levels of ALT and AST in the 3-MA group were significantly higher than those in the HBSP group (Fig. 3C). Thus, the protective effect of HBSP against hepatic I/R injury is weakened by the inhibition of autophagy.
Inhibiting autophagy reverses the protective effects of HBSP in hepatic I/R injury. (A) Representative photographs of immunoblots against LC3I, LC3II, Beclin1, and β-actin (full-length blots are presented in the Supplementary Information file). (B) Representative photographs (200×) of haematoxylin–eosin-stained liver sections, Scar bar,50 μm. (C) Histopathological scoring of hepatic injury was performed. (D) Serum ALT and AST levels. *Significant difference from HBSP group, *p < 0.05, **p < 0.01.
Inhibition of mTOR enhances autophagy and strengthens HBSP-mediated protection against hepatic I/R injury
We found that mTOR phosphorylation levels in the HBSP group were significantly lower than those in the I/R group (Fig. 4A). Inhibition of mTOR phosphorylation with rapamycin27,28 reinforced autophagy (Fig. 4B), alleviated the infiltrated inflammatory cells (Fig. 4C), and intensified the ALT and AST levels (Fig. 4D) compared with the levels in the HBSP group. Together, these findings suggest that the protective effects of HBSP on the liver are bolstered by enhancing autophagy via inhibition of phospho-mTOR.
mTOR inhibition enhances autophagy and strengthens the protective effect of HBSP. (A) Representative photographs of immunoblots against phospho-mTOR and mTOR (full-length blots are presented in the Supplementary Information file) (B) Representative photographs of immunoblots against phospho-mTOR, mTOR, LC3, and β-actin. full-length blots are presented in the Supplementary Information file. (C) Representative photographs (200×) of haematoxylin–eosin-stained liver sections, Scar bar, 50 μm. (D) Histopathological scoring of hepatic injury was performed. (E) Serum ALT and AST levels. *Significant difference from HBSP group, *p < 0.05, **p < 0.01.
HBSP partially reduces liver tissue apoptosis during hepatic I/R injury
Terminal deoxynucleotidyl transferase dUTP nick end labelling (TUNEL) was used to assess the degree of liver tissue apoptosis. Apoptosis of liver cells in the HBSP group occurred less frequently than those in the I/R group (Fig. 5A). The protective effect of HBSP on liver tissue was diminished by the Akt inhibitor Ly294002, and the degree of apoptosis was higher in the Ly294002 group than that in the HBSP group (Fig. 5B). However, comparing to 3-MA, which inhibited autophagy, the degree of liver function injury evaluated by ALT and AST in Ly294002 group was not that worse than that in 3-MA group. It may be inferred that autophagy play the primary role, and the activation of akt makes a partially contribution to the protection of HBSP in hepatic I/R injury.
HBSP reduces liver tissue apoptosis during hepatic I/R injury. (A) Representative photographs of haematoxylin–eosin-stained section, and immunohistochemical staining for TUNEL in liver sections; Scar bar, 50 μm. (B) Serum ALT and AST levels. (C) Histopathological scoring of hepatic injury was performed and TUNEL-positive level was also quantificated. (D) Representative photographs of immunoblots against phospho-Akt and Akt (full-length blots are presented in the Supplementary Information file). *Significant difference from HBSP group; *p < 0.05, **p < 0.01.
HBSP alleviates AML-12 cells hypoxia injury induced by CoCl2
CoCl2 was often used as hypoxia mimic reagent. We found that the levels of ALT, AST, and LDH in the culture supernatant of AML-12 cells increased as the CoCl2 stimulation time increased (Fig. 6A) and the levels of ALT, AST, and LDH in the supernatants of cells treated with HBSP were lower than those without HBSP treatment (Fig. 6B). In addition, the expression of HIF-1α (a key transcription factor response to hypoxic stress)29 in cells treated with HBSP also decreased when compared with that in non-HBSP-treated cells (Fig. 6C,D). We also found that the level of autophagy in HBSP treated group was higher than that in non-HBSP treated group (Fig. 6E,F).
(A,B) AML-12 cells culture supernatant ALT, AST and LDH levels, *Significant difference from normal group (0 h). *p < 0.05, **p < 0.01. (C) Immunohistochemical staining for HIF-α in slides of AML-12 cells, Scar bar, 50 μm. (D) HIF-α positive level. (E) Representative image of GFP-LC3B puncta and mRFP-LC3B puncta in AML-12/mRFP-GFP-LC3 cells. (F) Quantification of LC3B positive autolysosomes or autophagosomes in AML-12/mRFP-GFP-LC3 cells. (B,D,F) *Significant difference from HBSP-/CoCl2 12 h group, #Significant difference from HBSP-/CoCl2 24 h group; *p < 0.05, #p < 0.05.
Discussion
Early studies showed that autophagy played an important role in different I/R injury30,31,32,33 and increased autophagy was believed to have a beneficial effect on liver I/R injury34,35,36. Some features of hepatocytes were tightly dependent on autophagy37. Based on prior studies that autophagy played an unprecedented role in regulating cell function, as well as regulating liver lesions, by using genetic or chemical methods to block or increase the level of autophagy.
Recently, several studies have reported that HBSP displayed anti-inflammatory and tissue-protective activities in various I/R injuries3. However, the underlying mechanism remained largely unknown. HBSP mediates protective effects against myocardial I/R injury, chronic heart failure (CHF), and renal I/R injury4,5,38. But its role in hepatic I/R injury has not been reported in the literature. We found that HBSP protected against hepatic I/R injury via autophagy and Akt signalling.
Whether the activation of autophagy is the key mechanism of the protection conferred by HBSP in liver I/R injury remains unclear. Therefore, the aim of our study was to determine whether the autophagy pathway mediates the protective effects of HBSP treating in the liver. In our study, we found that HBSP could reduce hepatic I/R injury in vivo and the damage caused by hypoxia culture of hepatocytes in vitro. Simultaneously, HBSP resulted in increased autophagy in liver tissue in vivo and hepatocytes in vitro. The protective effects of HBSP in hepatic I/R injury were abolished with the inhibition of autophagy by 3-MA. These findings reveal that the hepatoprotective effect of HBSP against hepatic I/R injury depends, at least in part, on the activation of the autophagy. These findings indicate a critical role for autophagy in HBSP-mediated protection from hepatic I/R injury. Many molecules regulate and mediate autophagy, such as the ULK1 complex, mTORC1, AMPK, and TFEB39. There are literatures confirming that HBSP works through the mTOR pathway in disease, however its mechanism in hepatic ischaemia-reperfusion injury is not clear40,41. In order to identify the possible mechanism of HBSP in the regulation of hepatic I/R injury, we inhibited the activity of mTOR by Rapamycin. We found that rapamycin enhanced the protective effect and the level of autophagy in the model of HBSP protection hepatic I/R injuries. These results suggest that the mTOR pathway may be involved in the regulation of autophagy associated with HBSP-induced protection against hepatic I/R injury, and regulating mTOR-autophagy signaling pathway may be a way to reduce liver I/R injury.
In addition, we found that AKT was activatied by HBSP in vivo and HBSP can reduce liver tissue apoptosis. Furthermore, the combination of HBSP and Ly294002 treatment group contributed a lower hepatoprotective effect and relatively more severe apoptosis, indicating that Akt may be partially involved in the regulation of liver tissue apoptosis by HBSP during hepatic I/R injury.
However, there are still some limitations to our study that should be acknowledged. Firstly, the consequence of I/R injury include transient liver dysfunction and the systemic inflammatory response to syndrome, the indicators that reflected the systemic cytokines such as IL-6 or TNF levels in the sera from the blood samples of mice were not given. We only focused on the main outcome of I/R injury, which referred to the indicators widely used in clinical such as hepatic serum enzymes. Secondly, for some economic and technical limitations, the lack of autophagy gene knockout mice was an area of weakness for this study. So, in next research, we plan to screen out the key autophagy gene, then acquiring the right gene KO mice, and eventually could explain the molecular mechanism in depth of HBSP-protected the hepatic I/R injury.
In summary, our data demonstrated that HBSP mediated protective effects against hepatic I/R injury by regulating autophagy through the mTOR-autophagy pathway. This is the first time to clarify the key role of mTOR-autophagy signaling in regulating HBSP-mediated the protection of liver I/R injury. Another important implication of our results was that AKT was also an important factor in hepatic I/R injury. It is not clear whether the autophagy pathway and AKT pathway interact in this process.
Our study offers further evidence for the protective mechanism of HBSP in hepatic I/R injury, which has remained unclear despite numerous previous studies. This study also provides new targets for drugs to relieve hepatic I/R injury. However, the potential relationship between the different pathways involved requires further investigation.
Methods
Animals
The study was approved by the Institutional Animal Care and Use Committee at Tongji Medical College, Huazhong University of Science and Technology and all methods were carried out in accordance with the relevant guidelines and regulations of the Institutional Animal Care and Use Committee at Tongji Medical College, Huazhong University of Science and Technology. C57BL/6 mice were purchased from Beijing Vital River Laboratory Animal Technology, and maintained in the animal facility of the Institute of Transplantation, Tongji Hospital Affiliated to Tongji Medical College, Huazhong University of Science and Technology. At the time of experimentation, the mice were 8–10 weeks of age and weighed 22 g ± 2 g.
Cell culture
For cell propagation, AML12 cell line (ATCC®CRL-2254TM) were grown in DMEM/F12 medium (Hyclone) containing 10% fetal bovine serum (Gibco), supplemented with 100 U/mL penicillin and 100 g/mL streptomycin (Gibco), and incubation under an atmosphere of 5% CO2. The cell hypoxia model was established by chemical regent cobalt chloride42 (CoCl2, Sigma, St. Louis, Missouri). The final concentration of CoCl2 was 200 μM. When CoCl2 was added to culture medium, the FBS final concentration was changed to 0.5%. Cells were harvested in the indicated time and then detecting the ALT/AST/LDH from the culture medium.
Reagents
HBSP was synthesized at Shanghai Ketai Biotechnology. Rapamycin (9904) and Ly294002 (9901), and antibodies against LC3 (2775), Beclin1 (3495), β-actin (4967), phospho-mTOR (5536), mTOR (2983), p-Akt (4060), and Akt (4691) were purchased from Cell Signaling Technology. Antibodies against HIF-1α (ab82832) was purchaded from Abcam. Goat anti-rabbit IgG (7074) and goat anti-mouse IgG (7076) were purchased from Cell Signaling Technology. We purchased 3-MA (S2767) from Selleck Chemicals. Ad-mRFP-GFP-LC3 adenoviral was purchaded from DesignGene (Shanghai).
Hepatic I/R model
In this study, we used a 70% hepatic I/R model. The blood vessels were occluded for 60 minutes to block the flow of blood to the left and middle lobes of the liver. The mice were sacrificed 6 hours after the blood vessels were opened. The sham operation group underwent only laparotomy without clamping of the blood vessels. Mice in the HBSP group were intraperitoneally injected with HBSP 12 hours before the operation, during the operation, and 3 hours after opening the blood vessel. The I/R group were injected intraperitoneally with an equal volume of saline at the same time points. Ly294002, 3-MA, and rapamycin were injected intraperitoneally into mice 0.5 hours before the administration of HBSP11.
Serum sample assays
Serum ALT, AST and LDH levels were measured with a standard clinical automatic analyser in the clinical laboratory of Tongji Hospital affiliated to Tongji Medical College, Huazhong University of Science and Technology.
Liver tissue pathology
We fixed fresh liver tissue in 10% paraformaldehyde, then dehydrated the tissue in a series of increasing alcohol concentrations followed by xylene. Then, the tissue was placed in paraffin wax, embedded, and stained with standard haematoxylin–eosin–safran and picrosirius. We captured images with a microscope (NIKON ECLIPSE CI). Histological evaluation was performed using a semi-quantitative scoring system43.
Histological criteria for assessment of liver damage after I/R injury
The morphology results were assessed single blindly by a pathologist. In detail, the histological criteria for assessment of liver damage after I/R injury in this study was first introduced by Suzuki in 199344. In brief, the assessment was considered in three aspects, including sinusoidal congestion, hepatocyte necrosis and ballooning degeneration. Each item was given the score from 0 to 4 depending on the degree of liver damage. When there were no congestion, vacuolization and necrosis, it was given a best score 0. Otherwise, if there were severe congestion accompanying with severe vacuolization and >60% necrosis area, the score was up to 12.
Confocal microscopy
AML12 cell line was cultured on glass coverslip in 24 well plates and transfected with Ad-mRFP-GFP-LC3 adenoviral (MOI = 50) for 48 h followed by adding CoCl2 (final concentration 200 μM). The strength of the autophagic flow was determined by different fluorescence using a confocal scanning laser microscopy connected to the controlled computer. One of the fluorescence, mRFP was used to label and track LC3. Since the sensitivity of GFP fluorescent proteins to acidity, when autophagosomes were fused with lysosomes, GFP fluorescence was quenched and only red fluorescence was detected. So, the attenuation of GFP indicated the fusion stage of lysosomes and autophagosomes, which were formed into autolysosome occurred at the late autophagy stage. The yellow spots that appeared after we merged red-green double fluorescence after microscopic imaging were only autophagosomes. The red spots indicated autolysosome, and the intensity of autophagic flow could be clearly seen by counting the spots of different colors.
Electron microscopy (EM)
The liver tissue was cut into pieces (1 mm × 1 mm × 2 mm), washed twice with saline, then fixed in glutaraldehyde for 2 hours. After rinsing, the tissue pieces were dehydrated in a series of increasing alcohol concentrations, then embedded, and cut into slices of 50–60 nm using the ultrathin slicer (Leica, LeicaUC7); photographs were taken with the transmission electron microscope (Hitachi, HT7700).
TUNEL assay
Cell death in liver paraffin sections was detected by the TUNEL assay. The assay was performed according to the manufacturer’s instructions for the In Situ Cell Death Detection Kit (Roche, 11684817910).
Western blot analysis
Briefly, 60 μg of extracted protein was subjected to separation by 12% SDS–PAGE and transferred to PVDF membranes (Millipore). Nonspecific binding sites were blocked with TBST with 5% bovine serum albumin for 1 hour at room temperature. The membranes were incubated with primary antibodies at 4 °C overnight, then washed and incubated with the secondary antibodies for 1 hour at room temperature, followed by washing and signal detection. The protein expression levels were quantified with Image-Pro Plus software (Media Cybernetics).
Statistical analysis
All data are expressed as the mean ± SD. The data were analysed using a one-way analysis of variance followed by the least squares difference test (assuming equal variances) or Tamhane’s T2 test (without the assumption of equal variances). Comparisons between groups were performed with the two-tailed Student’s t test. A p-value < 0.05 was considered statistically significant.
References
Hache, G. et al. ARA290, a Specific Agonist of Erythropoietin/CD131 Heteroreceptor, Improves Circulating Endothelial Progenitors’ Angiogenic Potential and Homing Ability. Shock 46, 390–397, https://doi.org/10.1097/SHK.0000000000000606 (2016).
Chen, H. et al. Therapeutic effects of nonerythropoietic erythropoietin analog ARA290 in experimental autoimmune encephalomyelitis rat. J Neuroimmunol 268, 64–70, https://doi.org/10.1016/j.jneuroim.2014.01.006 (2014).
Muller, C. et al. ARA290 improves insulin release and glucose tolerance in type 2 diabetic GK rats. Mol. Med. 21, 969–978 (2015).
Brines, M. et al. Nonerythropoietic, tissue-protective peptides derived from the tertiary structure of erythropoietin. Proc. Natl. Acad. Sci. USA 105, 10925–10930 (2008).
Ahmet, I. et al. A small nonerythropoietic helix B surface peptide based upon erythropoietin structure is cardioprotective against ischemic myocardial damage. Mol. Med. 17, 194–200 (2011).
Ueba, H. et al. Cardioprotection by a nonerythropoietic, tissue-protective peptide mimicking the 3D structure of erythropoietin. Proc. Natl. Acad. Sci. USA 107, 14357–14362 (2010).
Yang, C. et al. A novel proteolysis-resistant cyclic helix B peptide ameliorates kidney ischemia reperfusion injury. Biochim. Biophys. Acta 1842, 2306–2317 (2014).
Ueba, H. et al. Suppression of coronary atherosclerosis by helix B surface peptide, a nonerythropoietic, tissue-protective compound derived from erythropoietin. Mol. Med. 19, 195–202 (2013).
Ahmet, I. et al. Chronic administration of small nonerythropoietic peptide sequence of erythropoietin effectively ameliorates the progression of postmyocardial infarction-dilated cardiomyopathy. J. Pharmacol. Exp. Ther. 345, 446–456 (2013).
Hu, J. et al. Targeting TRAF3 signaling protects against hepatic ischemia/reperfusions injury. J. Hepatol. 64, 146–159 (2016).
Wang, D. et al. The role of AKT1 and autophagy in the protective effect of hydrogen sulphide against hepatic ischemia/reperfusion injury in mice. Autophagy 8, 954–962 (2012).
Rickenbacher, A. et al. Fasting protects liver from ischemic injury through Sirt1-mediated downregulation of circulating HMGB1 in mice. J. Hepatol. 61, 301–308 (2014).
Rautou, P. E. et al. Autophagy in liver diseases. J. Hepatol. 53, 1123–1134 (2010).
Cardinal, J., Pan, P. & Tsung, A. Protective role of cisplatin in ischemic liver injury through induction of autophagy. Autophagy 5, 1211–1212 (2009).
Yang, J. et al. The role of 1,25-dyhydroxyvitamin D3 in mouse liver ischemia reperfusion injury: regulation of autophagy through activation of MEK/ERK signaling and PTEN/PI3K/Akt/mTORC1 signaling. Am. J. Transl. Res. 7, 2630–2645 (2015).
Kang, J. W., Cho, H. I. & Lee, S. M. Melatonin inhibits mTOR-dependent autophagy during liver ischemia/reperfusion. Cell. Physiol. Biochem. 33, 23–36 (2014).
Wang, J. H. et al. Autophagy suppresses age-dependent ischemia and reperfusion injury in livers of mice. Gastroenterology 141, 2188–2199 (2011).
Czaja, M. J. Functions of autophagy in hepatic and pancreatic physiology and disease. Gastroenterology 140, 1895–1908 (2011).
Rossman, J. S. & Lamb, R. A. Autophagy, apoptosis, and the influenza virus M2 protein. Cell Host Microbe 6, 299–300 (2009).
Fan, W. et al. Endothelial deletion of mTORC1 protects against hindlimb ischemia in diabetic mice via activation of autophagy, attenuation of oxidative stress and alleviation of inflammation. Free Radic. Biol. Med. 108, 725–740 (2017).
Delbridge, L. M. D., Mellor, K. M., Taylor, D. J. & Gottlieb, R. A. Myocardial stress and autophagy: mechanisms and potential therapies. Nat. Rev. Cardiol. 14, 412–425 (2017).
Dai, S. H. et al. Sirt3 confers protection against neuronal ischemia by inducing autophagy: Involvement of the AMPK-mTOR pathway. Free Radic. Biol. Med. 108, 345–353 (2017).
Pu, T. et al. Augmenter of liver regeneration regulates autophagy in renal ischemia-reperfusion injury via the AMPK/mTOR pathway. Apoptosis 22, 955–969 (2017).
Gracia-Sancho, J., Guixe-Muntet, S., Hide, D. & Bosch, J. Modulation of autophagy for the treatment of liver diseases. Expert Opin. Investig. Drugs 23, 965–977 (2014).
Ghavami, S. et al. S100A8/A9 induces autophagy and apoptosis via ROS-mediated cross-talk between mitochondria and lysosomes that involves BNIP3. Cell Res. 20, 314–331 (2010).
Liu, A. et al. Ischemic preconditioning attenuates ischemia/reperfusion injury in rat steatotic liver: role of heme oxygenase-1-mediated autophagy. Oncotarget 7, 78372–78386 (2016).
Li, T. et al. Arsenic trioxide promoting ETosis in acute promyelocytic leukemia through mTOR-regulated autophagy. Cell Death Dis 9, 75, https://doi.org/10.1038/s41419-017-0018-3 (2018).
Ma, L. L. et al. Mammalian target of rapamycin inhibition attenuates myocardial ischaemia-reperfusion injury in hypertrophic heart. J Cell Mol Med 22, 1708–1719, https://doi.org/10.1111/jcmm.13451 (2018).
Majmundar, A. J., Wong, W. J. & Simon, M. C. Hypoxia-inducible factorsand the response to hypoxic stress. Mol Cell 40, 294–309 (2010).
Xin, D. et al. l-Cysteine suppresses hypoxia-ischemia injury in neonatal mice by reducing glial activation, promoting autophagic flux and mediating synaptic modification via H2S formation. Brain Behav Immun, https://doi.org/10.1016/j.bbi.2018.05.007 (2018).
Song, D. D. et al. Sphingosine kinase 2 activates autophagy and protects neurons against ischemic injury through interaction with Bcl-2 via its putative BH3 domain. Cell Death Dis 8, e2912, https://doi.org/10.1038/cddis.2017.289 (2017).
Xie, Y. et al. Ischemic preconditioning attenuates ischemia/reperfusion-induced kidney injury by activating autophagy via the SGK1 signaling pathway. Cell Death Dis 9, 338, https://doi.org/10.1038/s41419-018-0358-7 (2018).
Zheng, Z. et al. Mesenchymal Stem Cells Protect Against Hypoxia-Ischemia Brain Damage by Enhancing Autophagy Through Brain Derived Neurotrophic Factor/Mammalin Target of Rapamycin Signaling Pathway. Stem Cells. https://doi.org/10.1002/stem.2808 (2018).
Xu, D. et al. The triterpenoid CDDO-imidazolide ameliorates mouse liver ischemia-reperfusion injury through activating the Nrf2/HO-1 pathway enhanced autophagy. Cell Death Dis 8, e2983, https://doi.org/10.1038/cddis.2017.386 (2017).
Sun, H. et al. Octreotide Attenuates Acute Kidney Injury after Hepatic Ischemia and Reperfusion by EnhancingAutophagy. Scientific reports 7, 42701, https://doi.org/10.1038/srep42701 (2017).
Schneider, J. L. & Cuervo, A. M. Liver autophagy: much more than just taking out the trash. Nat. Rev. Gastroenterol. Hepatol. 11, 187–200 (2014).
Czaja, M. J. et al. Functions of autophagy in normal and diseased liver. Autophagy 9, 1131–1158 (2013).
Liu, P. et al. Helix B Surface Peptide Protects against Acute Myocardial Ischemia-Reperfusion Injury via the RISK and SAFE Pathways in a Mouse Model. Cardiology 134, 109–117, https://doi.org/10.1159/000443680 (2016).
Wang, X. & Cui, T. Autophagy modulation: a potential therapeutic approach in cardiac hypertrophy. Am. J. Physiol. Heart Circ. Physiol. 313, H304–H319 (2017).
Lin, C. et al. Helix B surface peptide attenuates diabetic cardiomyopathy via AMPK-dependent autophagy. Biochemical and biophysical research communications 482, 665–671, https://doi.org/10.1016/j.bbrc.2016.11.091 (2017).
Wu, S. et al. The Protective Effects of Helix B Surface Peptide on Experimental Acute Liver Injury Induced by Carbon Tetrachloride. Digestive diseases and sciences 62, 1537–1549, https://doi.org/10.1007/s10620-017-4553-7 (2017).
Hudson, C. C. et al. Regulation of hypoxia-inducible factor 1 alpha expression and function by the mammalian target of rapamycin. Mol Cell Biol 22, 7004–7014 (2002).
Fang, H., Liu, A., Dahmen, U. & Dirsch, O. Dual role of chloroquine in liver ischemia reperfusion injury: reduction of liver damage in early phase, but aggravation in late phase. Cell Death Dis. 4, e694, https://doi.org/10.1038/cddis.2013.225 (2013).
Suzuki, S. et al. Neutrophil infiltration as an important factor in liver ischemia and reperfusion injury. Modulating effects of FK506 and cyclosporine. Transplantation 55, 1265–1272 (1993).
Acknowledgements
This study was supported by a grant from the National Natural Science Foundation of China (No. 81370581, 81770652, 81470934).
Author information
Authors and Affiliations
Contributions
Rumeng Tan and Zhishui Chen conceived the article. Rumeng Tan, Hongzhe Tian and Zhishui Chen wrote the main text. Rumeng Tan, Hongzhe Tian, Bo Yang, Bo Zhang, Chen Dai, Zhenyi Han, Yakun Li, Meixi Wang, Guangyao Wang, Huifang Yang, and Zhishui Chen performed experiments. Rumeng Tan, Hongzhe Tian, Lai Wei, Dong Chen and Zhishui Chen analyzed data. Fan He gave us great help during the article revision stage. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tan, R., Tian, H., Yang, B. et al. Autophagy and Akt in the protective effect of erythropoietin helix B surface peptide against hepatic ischaemia/reperfusion injury in mice. Sci Rep 8, 14703 (2018). https://doi.org/10.1038/s41598-018-33028-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-33028-3
Keywords
This article is cited by
-
Autophagy in hepatic ischemia–reperfusion injury
Cell Death Discovery (2023)
-
Erythropoietin and its derivatives: from tissue protection to immune regulation
Cell Death & Disease (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.