Abstract
Non-alcoholic fatty liver disease (NAFLD) is a prevalent liver disease encompassing a broad spectrum of pathologic changes in the liver. Metabolic derangements are suggested to be main causes of NAFLD. As thyroid hormone is a main regulator of energy metabolism, there may be a link between NAFLD and thyroid function. In previous studies, the association between NAFLD and thyroid function was not conclusive. The aim of this study was to clarify the relationship between NAFLD and thyroid function, focusing on subclinical hypothyroidism, using nationwide survey data representing the Korean population. NAFLD was defined as a hepatic steatosis index of 36 or higher. Based on the analysis of nationwide representative data, subclinical hypothyroidism was related to a high risk of NAFLD in males, but not in females. Our study showed that thyroid function might play a substantial role in the development of NAFLD, especially in males. Further study to elucidate the underlying mechanism of gender specific association of mild thyroid dysfunction and NAFLD would be required.
Similar content being viewed by others
Introduction
Non-alcoholic fatty liver disease (NAFLD) is a prevalent liver disease characterized by an accumulation of lipid droplets in hepatocytes without excessive alcohol consumption, as defined as ≥30 g alcohol/day for males and ≥20 g alcohol/day for females1. The prevalence of NAFLD has been reported to be approximately 30% in the Western population2. NAFLD has also become prevalent in Asia, and it has been reported that approximately 16.1–27.2% of adults in Korea have NAFLD according to ultrasonographic findings3,4. Clinical consequences of NAFLD include simple steatosis, non-alcoholic steatohepatitis (NASH), fibrosis, cirrhosis and hepatocellular carcinoma. Liver cirrhosis caused by NAFLD has recently become a leading cause of liver transplantation5. Additionally, NAFLD has been reported to be linked to increased cardiovascular mortality as well as diabetes-related mortality6, emphasizing the clinical importance of NAFLD. The disease can be confirmed by liver biopsy-mediated identification of more than 5% fat infiltration in hepatocytes7. However, as liver biopsy is an invasive procedure, alternative approaches, including magnetic resonance imaging (MRI) and ultrasound sonography (US), are also used for the diagnosis of NAFLD8. Other tools such as the hepatic steatosis index (HSI) and laboratory tests9,10 can also be used for NAFLD diagnosis.
As hypertension, dyslipidaemia, diabetes mellitus (DM), and central obesity are well established risk factors for NAFLD, insulin resistance is suggested to be closely related to the development of NAFLD11,12. Indeed, NAFLD has been considered as the hepatic presentation of metabolic syndrome, which is caused by insulin resistance. Therefore, medical conditions that induce insulin resistance may be associated with a high risk of NAFLD development.
Thyroid hormone plays a key role in energy homeostasis and is directly involved in glucose13 and lipid metabolism14,15. Increased insulin resistance and dyslipidaemia are observed in hypothyroidism, even in subclinical hypothyroidism, and several studies have shown that subclinical hypothyroidism is related to an increased risk of metabolic syndrome16,17,18,19. As metabolic derangements including metabolic syndrome are associated with NAFLD development, several studies had investigated correlations between thyroid dysfunction and NAFLD. However, such an association has not yet been confirmed, with some studies supporting an association between hypothyroidism and NAFLD20,21,22,23,24,25, and others not26,27,28. Thus, the aim of this study was to investigate the risk of NAFLD, as estimated by HSI, in subclinical hypothyroidism subjects compared to euthyroid subjects using nationally representative data.
Results
Baseline characteristics
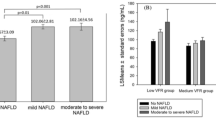
In total, 3452 subjects (43.4%, male; 56.4%. female) were recruited, with a mean age of 44.8 years (range 44.5–45.1). Among these, 128 subjects (3.7%) showed subclinical hypothyroidism. Table 1 summarizes the demographic and clinical baseline characteristics between the euthyroid group and subclinical hypothyroidism group. There were no significant differences in gender, smoking status, physical activity, income, prevalence of metabolic syndrome, DM, or HSI score distribution. However, subjects with subclinical hypothyroidism were older, with significantly higher urine iodine creatinine ratio (UICR) and thyroid peroxidase antibody (TPOAb) positivity. Prevalence of NAFLD by HSI (≥36) was 33.3% in the euthyroid group and 41.5% in the subclinical hypothyroidism group, with no significant difference found between the two groups.
Association between NAFLD and subclinical hypothyroidism
Subclinical hypothyroidism was related to a high risk of NAFLD, without significance (odds ratio (OR) = 1.42, p = 0.093, 95% CI (0.94–2.14) (Table 2). A significant association between subclinical hypothyroidism and NAFLD was also not observed after adjustment. Considering that the presence of TPOAb is closely related to subclinical hypothyroidism, subgroup analysis according to TPOAb positivity was performed. As shown in Table 2, no significant association between subclinical hypothyroidism and NAFLD was found. In addition, males and females were analysed separately, with males with subclinical hypothyroidism showing an increased risk of NAFLD that was significant after adjustment for possible confounders (OR = 2.37, 95% confidence interval (CI) 1.09–5.12, p = 0.029) (Table 3). The confounders included age, waist circumference and physical activity, socioeconomic status, components of metabolic syndrome, UICR and presence of TPOAb. However, no significant association was found in females with subclinical hypothyroidism and NAFLD.
Discussion
In this study, the association between subclinical hypothyroidism and NAFLD was evaluated in population representative data. Subclinical hypothyroidism was defined by thyroid-stimulating hormone (TSH) reference ranges based on the 2.5th and 97.5th percentiles in the studied population. NAFLD was determined by HSI scores. Unlike in female subjects, subclinical hypothyroidism was related to increased risk of NAFLD in males, and statistical significance was still observed after adjustment for possible confounding factors.
Because thyroid hormone is closely linked to metabolism regulation15, metabolic derangements such as dyslipidaemia and diastolic hypertension29, can occur in overt hypothyroidism. As subclinical hypothyroidism can represent a transition of normal thyroid function to overt hypothyroidism, it is also suspected to have effects on metabolic derangement17,30. Thus, the association between NAFLD, considered to be a hepatic manifestation of metabolic syndrome, and subclinical hypothyroidism should be addressed.
There are several studies to date evaluating the association between overt or subclinical hypothyroidism and NAFLD. A high incidence of hypothyroidism in NAFLD patients suggests a possible link between NAFLD and thyroid dysfunction21,23. Within this context, previous studies have revealed increased TSH and lower serum free thyroxine (fT4) to be associated with NAFLD24,31. However, although increased TSH levels or subclinical hypothyroidism may have been related to NAFLD in some studies20,25,32,33, fT4 or free T3, and not TSH, was found in other studies to be associated with an increased risk of NAFLD34,35,36. No association between thyroid function and NAFLD has also been reported28,37,38. Differences in ethnicity, NAFLD definition and population size might cause inconsistent results. Additionally, most of the studies did not use population-based data. As our study utilized the Sixth Korea National Health and Nutrition Examination Survey (KNAHNES VI 2013–2015), which represents the Korean ethnic population, the observed association between NAFLD and subclinical hypothyroidism in males has clinical significance.
A gender-specific association between subclinical hypothyroidism and NAFLD was found in this study, and there may be several explanations for such gender differences. First, differences in hepatic lipid metabolism between male and female, in terms of development of NAFLD, would be related to our results. In previous study39, male, compared to female, had shown decreased fatty acid oxidation and increased lipogenesis in the liver, which could lead to hepatic steatosis. Considering the substantial effects of thyroid hormone on hepatic lipid metabolisms40, subtle thyroid dysfunction (subclinical hypothyroidism) could augment fatty acid metabolism differences between male and female. It might be related to the significant association of subclinical hypothyroidism with NAFLD risk only in male but not in female. Secondly, effects of hypooestrogenaemia on development of NAFLD would cause the gender-specific association. Recent studies have shown hypooestrogenaemia induced massive hepatic steatosis and hepatic fibrosis in animal models41,42,43. It may be assumed that the impact of oestrogen on NAFLD development is stronger than the impact of subtle thyroid dysfunction in females. However, it could not fully explain the phenomenon because no significant association of subclinical hypothyroidism with increased risk of NAFLD was found in our subgroup analysis of premenopausal women, who would be relatively free from oestrogen deficiency. Lastly, over- and underestimation of subclinical hypothyroidism in males and females, respectively, can affect results. In fact, subclinical hypothyroidism was defined based on the same TSH values in both genders. However, referring to a recent analysis of TSH reference ranges for the Korean population44, the 97.5th percentile of TSH in females was higher than that in males. Thus, overestimation of subclinical hypothyroidism in males and underestimation in females might to some degree affect the association between subclinical hypothyroidism and NAFLD.
The present study has several limitations. First, as this study was based on cross-sectional data, we could not confirm a causal relationship between thyroid dysfunction and NAFLD. Second, as insulin was not measured throughout the survey period, insulin resistance, such as that evaluated by Homeostatic Model Assessment of Insulin Resistance (HOMAR-IR), could not be examined. Third, thyroid function and hepatic enzyme levels were only measured once, and triiodothyronine was not assessed. Another limitation is that the exclusion for liver disease was not based on medical records. Finally, NAFLD was not diagnosed by liver biopsy in this study. Although liver biopsy is considered the gold standard for NAFLD45, liver biopsy is not routinely performed for diagnosis of NAFLD due to the invasiveness and complications of this procedure. Therefore, non-invasive methods for diagnosis are commonly used. In this large survey, liver US could not be applied for diagnosing NAFLD because liver US was not performed on all populations. The diagnosis of NAFLD in this study was based on a score (HSI) that utilizes laboratory test results. Several non-invasive approaches reflect biochemical tests and anthropometric parameters, including HSI, the fatty liver index (FLI) and Framingham criteria, for diagnosis of NAFLD46. As ethnicity affects the development of NAFLD47, it would be reasonable to use the method validated in our population. FLI has been validated in Western studies, with good performance48. In contrast, HSI was developed from a large case-control study including more than 5000 Koreans whose ultrasonographic findings indicated the potential for NAFLD. HSI showed a significant correlation with ultrasonographic fatty liver grade and can be used as a diagnostic tool for predicting the presence of NAFLD with reliable accuracy (specificity 93.1% (95% CI, 92.0–94.0) and a positive likelihood ratio of 6.505 (95% CI, 5.628–7.519))10. In several studies, HSI was validated as an overall good diagnostic performance46,49,50. In addition, gamma-glutamyltransferase levels are required for the application of FLI, these were not available in our database. Thus, diagnosis of NAFLD based on HSI appears to be appropriate for studying the Korean population.
Despite some limitations, this study has several strengths. First, this is the first nationwide study investigating the association between subclinical hypothyroidism and NAFLD diagnosed using a non-invasive tool. Second, the TSH reference range analysed to represent the Korean population was used in this study. As previously recommended51, the reference range of TSH may differ among ethnicities. Thus, the incidence of subclinical disease may be changed according to the reference range applied for defining the disease. As we adopted the reference range (2.5th percentile to 97.5th percentile) based on values acquired from population representative data, this can be considered a strength of our study. In fact, we also analysed the data based on the general reference of 0.4–4.0 mIU/L because validation of the TSH cut-off values (6.86 mIU/L;97.5th percentile in Korean population) for subclinical hypothyroidism is still needed. When cut-off values for subclinical hypothyroidism were lowered, statistical significance of the association between NAFLD and subclinical hypothyroidism in males became more prominent (Supplementary Table S2). Third, the large-sized sample enabled multiple sensitivity analyses.
Conclusion
In this study, subclinical hypothyroidism was found to be related to an increased risk of NAFLD in males but not in females. Thyroid function might play a substantial role in the development of NAFLD, especially in males. Further investigation to elucidate the gender-specific effects of mild thyroid dysfunction on NAFLD development is required.
Methods
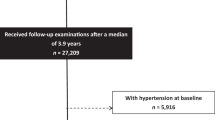
Study population
Data were based on the survey from KNHANES VI 2013–2015, a nationwide, cross-sectional survey conducted by the Korean Centres for Disease Control and Prevention (KCDC). Since 1998, KNHANES has been conducting an on-going nationwide survey that monitors the health and nutritional status of Koreans on an annual basis. The survey is composed of three components: a health interview, health examination and nutritional survey. The health interview and examination are conducted by trained medical personnel. The survey uses a stratified, multistage clustered probability sampling. KNHANES was approved by the Institutional Review Board (IRB) of the KCDC. Witten informed consent was obtained from all participants (KCDC; IRB approval No. 2013-07CON-03-4C). This study complied with the ethical standards of the Helsinki Declaration and was approved by the Catholic University of Korea, Catholic Medical Center, Seoul St, Mary’s Hospital Institutional Review Board (IRB approval No. PC17EESI0054).
During KNHANES VI (2013–2015), thyroid function tests were performed in subsampled subjects, as opposed to in all subjects, aged 10 years and over based on gender and age in each year (approximately 2400 participants per year). In this study, total 4037 subjects were selected first, as thyroid function test results were available, and these subjects were older than 19 years old. Subjects who met the following criteria were excluded: 1) excessive alcohol consumption, defined as ≥210 g alcohol/week for males and ≥140 g alcohol/week for females (n = 469); 2) history of viral hepatitis, positive serologic markers for hepatitis B and hepatitis C (hepatitis B; n = 38 and hepatitis C; n = 6) or chronic liver disease such as liver cirrhosis (n = 2); and 3) abnormal fT4 level (<0.82 ng/mL or >1.76 ng/mL) or history of treatment for thyroid disease (n = 70). Of the 3452 subjects who met the inclusion criteria, 3321 were ultimately selected for this study.
Clinical and laboratory measurements and definition of metabolic syndrome
Laboratory tests included the following: aspartate aminotransferase (AST), alanine aminotransferase (ALT), thyroid function tests and urine iodine. Blood samples and urine samples were processed by KNHANES protocol using a Hitachi 7600 automated chemistry analyzer (Hitachi, Tokyo, Japan). Serum TSH, fT4, and TPOAb, were measured by an electrochemiluminescence immunoassay using an E-TSH kit (Roche Diagnostics, Mannheim, Germany), an E-Free T4 kit (Roche Diagnostics, Mannheim, Germany) and an E-Anti-TPO kit (Roche Diagnostics, Mannheim, Germany), respectively. For urine analysis, subjects were asked to be fasting after 7 p.m. the day before the survey. Spot urine sampling was performed in fasting status and the first morning midstream urine was collected in most of population. Subjects, who were not able to collect the sample in the morning, were also fasting for more than 8 hours at the time of sampling. Urine iodine concentration (UIC) was analysed by inductively coupled plasma mass spectrometry (ICP-MS; Perkin Elmer ICP-MS, Waltham, MA, USA) using an Iodine standard (Inorganic Venture, Christiansburg, VA, USA). The UICR (mcg [iodine]/g [creatinine]) was calculated to compensate for the limitations of renal function correction and to adjust variable water excretion rates at the time of spot urine collection.
Metabolic syndrome was defined by a revised National Cholesterol Education Program52 and an Asian-specific waist circumference threshold from the International Diabetes Foundation43,53. Metabolic syndrome was diagnosed as the presence of three or more of the following criteria: (1) waist circumference ≥90 cm in males and ≥80 cm in females; (2) elevated triglyceride ≥ 150 md/dl or taking medication; (3) high-density lipoprotein (HDL)-cholesterol <40 mg/dL in males and <50 mg/dL in females or taking lipid-lowering agents; (4) systolic blood pressure ≥130 mmHg or diastolic blood pressure ≥85 mmHg or taking antihypertensive medications; and (5) elevated fasting glucose ≥100 mg/dL or oral hypoglycaemic agents use.
Assessment of thyroid function
In KNHANES, thyroid function tests were performed for TSH, fT4 and TPOAb. Previously, a nation-wide cross-sectional study to evaluate the distribution of serum TSH range in the Korean population, KNHANES VI suggested that the reference value was between 0.62 (the 2.5th percentile) and 6.68 (the 97.5th percentile) mIU/L. We determined a reference for serum TSH (0.62–6.68 mIU/L) and fT4 (0.82–1.76 ng/mL) levels. Euthyroidism was defined as serum TSH and fT4 levels within a normal range. Subclinical hypothyroidism was defined as a serum TSH concentration more than 6.68 mIU/L and serum fT4 within a normal range.
Diagnosis of NAFLD
Histologic staging and grading by liver biopsy are the gold standard for diagnosis of NAFLD. Nonetheless, due to the invasiveness, which can result in complications, imaging tests such as liver US and computed tomography are usually utilized for the diagnosis of NAFLD in clinical practice. However, liver imaging tests were not performed in KNHANES. Therefore, we adopted a diagnostic tool using laboratory tests and anthropometric factors. In our study, NAFLD was diagnosed through the previously validated fatty liver prediction model, namely, HSI:
The use of HSI as a diagnostic tool for NAFLD, compared to US, has been validated in a study of the Korean population10. NAFLD in this study was defined as an HSI value of 36 or higher.
Statistical analysis
Statistical analyses were performed using SAS survey procedures version 9.3 (SAS Institute, Cary, NC, USA). All analyses used sample weights for evaluating the entire Korean population by accounting for the complex survey design. Continuous variables are expressed as the median or mean and standard deviations, and categorical variables are described as frequencies (percentages). Comparisons of basic clinical characteristics between euthyroid and subclinical hypothyroidism groups were performed using Cramer-Rao chi-square tests, regarding basic clinical characteristics between the euthyroid group and subclinical hypothyroidism group where appropriate. Logistic regression was used to identify the association between thyroid function, as evaluated by elevated TSH and NAFLD, after adjustment for other variables. The correlation is presented as the OR with 95% confidence intervals. A p-value < 0.05 was considered statistically significant.
Data Availability Statement
All the data generated and/or analyzed during the current study are included in this article and are available from the corresponding author on reasonable request.
References
Angulo, P. Nonalcoholic fatty liver disease. N Engl J Med 346, 1221–1231 (2002).
Torres, D. M. & Harrison, S. A. Diagnosis and therapy of nonalcoholic steatohepatitis. Gastroenterology 134, 1682–1698 (2008).
Kim, H. J. et al. Metabolic significance of nonalcoholic fatty liver disease in nonobese, nondiabetic adults. Arch Intern Med 164, 2169–2175 (2004).
Park, S. H. et al. Prevalence and risk factors of non-alcoholic fatty liver disease among Korean adults. J Gastroenterol Hepatol 21, 138–143 (2006).
Singal, A. K., Hasanin, M., Kaif, M., Wiesner, R. & Kuo, Y. F. Nonalcoholic Steatohepatitis is the Most Rapidly Growing Indication for Simultaneous Liver Kidney Transplantation in the United States. Transplantation 100, 607–612 (2016).
Ballestri, S. et al. Nonalcoholic fatty liver disease is associated with an almost twofold increased risk of incident type 2 diabetes and metabolic syndrome. Evidence from a systematic review and meta-analysis. J Gastroenterol Hepatol 31, 936–944 (2016).
Nascimbeni, F. et al. Clinical relevance of liver histopathology and different histological classifications of NASH in adults. Expert review of gastroenterology & hepatology, 1–17 (2017).
Ballestri, S., Romagnoli, D., Nascimbeni, F., Francica, G. & Lonardo, A. Role of ultrasound in the diagnosis and treatment of nonalcoholic fatty liver disease and its complications. Expert review of gastroenterology & hepatology 9, 603–627 (2015).
Machado, M. V. & Cortez-Pinto, H. Non-invasive diagnosis of non-alcoholic fatty liver disease. A critical appraisal. Journal of hepatology 58, 1007–1019 (2013).
Lee, J. H. et al. Hepatic steatosis index: a simple screening tool reflecting nonalcoholic fatty liver disease. Dig Liver Dis 42, 503–508 (2010).
Lonardo, A., Ballestri, S., Marchesini, G., Angulo, P. & Loria, P. Nonalcoholic fatty liver disease: a precursor of the metabolic syndrome. Dig Liver Dis 47, 181–190 (2015).
Salgado, A. L. et al. Insulin resistance index (HOMA-IR) in the differentiation of patients with non-alcoholic fatty liver disease and healthy individuals. Arq Gastroenterol 47, 165–169 (2010).
McAninch, E. A. & Bianco, A. C. Thyroid hormone signaling in energy homeostasis and energy metabolism. Ann N Y Acad Sci 1311, 77–87 (2014).
Cordeiro, A., Souza, L. L., Einicker-Lamas, M. & Pazos-Moura, C. C. Non-classic thyroid hormone signalling involved in hepatic lipid metabolism. J Endocrinol 216, R47–57 (2013).
Mullur, R., Liu, Y. Y. & Brent, G. A. Thyroid hormone regulation of metabolism. Physiol Rev 94, 355–382 (2014).
Ujwal Upadya, B. et al. Effect of insulin resistance in assessing the clinical outcome of clinical and subclinical hypothyroid patients. J Clin Diagn Res 9, OC01–04 (2015).
Maratou, E. et al. Studies of insulin resistance in patients with clinical and subclinical hypothyroidism. Eur J Endocrinol 160, 785–790 (2009).
Roos, A., Bakker, S. J., Links, T. P., Gans, R. O. & Wolffenbuttel, B. H. Thyroid function is associated with components of the metabolic syndrome in euthyroid subjects. J Clin Endocrinol Metab 92, 491–496 (2007).
Yang, L. et al. Subclinical hypothyroidism and the risk of metabolic syndrome: A meta-analysis of observational studies. Endocr Res 41, 158–165 (2016).
Chung, G. E. et al. Non-alcoholic fatty liver disease across the spectrum of hypothyroidism. J Hepatol 57, 150–156 (2012).
Liangpunsakul, S. & Chalasani, N. Is hypothyroidism a risk factor for non-alcoholic steatohepatitis? J Clin Gastroenterol 37, 340–343 (2003).
Silveira, M. G., Mendes, F. D., Diehl, N. N., Enders, F. T. & Lindor, K. D. Thyroid dysfunction in primary biliary cirrhosis, primary sclerosing cholangitis and non-alcoholic fatty liver disease. Liver Int 29, 1094–1100 (2009).
Pagadala, M. R. et al. Prevalence of hypothyroidism in nonalcoholic fatty liver disease. Dig Dis Sci 57, 528–534 (2012).
Bano, A. et al. Thyroid Function and the Risk of Nonalcoholic Fatty Liver Disease: The Rotterdam Study. J Clin Endocrinol Metab 101, 3204–3211 (2016).
Carulli, L. et al. Is nonalcoholic steatohepatitis associated with a high-though-normal thyroid stimulating hormone level and lower cholesterol levels? Intern Emerg Med 8, 297–305 (2013).
Jaruvongvanich, V., Sanguankeo, A. & Upala, S. Nonalcoholic Fatty Liver Disease Is Not Associated withThyroid Hormone Levels and Hypothyroidism: A Systematic Review and Meta-Analysis. Eur Thyroid J 6, 208–215 (2017).
Zhang, J. et al. Relationship between serum TSH level with obesity and NAFLD in euthyroid subjects. J Huazhong Univ Sci Technolog Med Sci 32, 47–52 (2012).
Lee, K. W. et al. Impact of hypothyroidism on the development of non-alcoholic fatty liver disease: A 4-year retrospective cohort study. Clin Mol Hepatol 21, 372–378 (2015).
Cappola, A. R. & Ladenson, P. W. Hypothyroidism and atherosclerosis. J Clin Endocrinol Metab 88, 2438–2444 (2003).
Yang, N. et al. Novel Clinical Evidence of an Association between Homocysteine and Insulin Resistance in Patients with Hypothyroidism or Subclinical Hypothyroidism. PLoS One 10, e0125922 (2015).
Xu, C., Xu, L., Yu, C., Miao, M. & Li, Y. Association between thyroid function and nonalcoholic fatty liver disease in euthyroid elderly Chinese. Clin Endocrinol (Oxf) 75, 240–246 (2011).
Lingad-Sayas, R. C., Montano, C. N. & Isidro, M. J. C. Prevalence of Elevated TSH and its Association with Dyslipidemia and NAFLD Among Filipino Adult Executive Check-Up Patients in a Tertiary Hospital. Philipp J Intern Med 55, 1–8 (2017).
Kassem, A., Khalil, F., Ramadan, M. R. & Rashed, M. Association and impact of non-alcoholic fatty liver disease on thyroid function. International Journal of Current Research in Medical Sciences 3, 94–107 (2017).
Ittermann, T. et al. Inverse association between serum free thyroxine levels and hepatic steatosis: results from the Study of Health in Pomerania. Thyroid 22, 568–574 (2012).
van den Berg, E. H. et al. Higher free triiodothyronine is associated with non-alcoholic fatty liver disease in euthyroid subjects: the Lifelines Cohort Study. Metabolism 67, 62–71 (2017).
Liu, G. et al. Free triiodothyronine levels are positively associated with non-alcoholic fatty liver disease in euthyroid middle-aged subjects. Endocr Res 40, 188–193 (2015).
Mazo, D. F. et al. Gluco-lipidic indices in treated hypothyroidism associated with nonalcoholic fatty liver disease. Arq Gastroenterol 48, 186–189 (2011).
Eshraghian, A., Dabbaghmanesh, M. H., Eshraghian, H., Fattahi, M. R. & Omrani, G. R. Nonalcoholic fatty liver disease in a cluster of Iranian population: thyroid status and metabolic risk factors. Arch Iran Med 16, 584–589 (2013).
Pramfalk, C. et al. Sex-Specific Differences in Hepatic Fat Oxidation and Synthesis May Explain the Higher Propensity for NAFLD in Men. J. Clin. Endocrinol. Metab. 100, 4425–4433, https://doi.org/10.1210/jc.2015-2649 (2015).
Sinha, R. A., Singh, B. K. & Yen, P. M. Direct effects of thyroid hormones on hepatic lipid metabolism. Nat. Rev. Endocrinol. 14, 259–269, https://doi.org/10.1038/nrendo.2018.10 (2018).
Angulo, P., Keach, J. C., Batts, K. P. & Lindor, K. D. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology 30, 1356–1362, https://doi.org/10.1002/hep.510300604 (1999).
Pinto, H. C. et al. Nonalcoholic steatohepatitis. Clinicopathological comparison with alcoholic hepatitis in ambulatory and hospitalized patients. Dig. Dis. Sci. 41, 172–179 (1996).
Lazo, M. et al. Prevalence of nonalcoholic fatty liver disease in the United States: the Third National Health and Nutrition Examination Survey, 1988–1994. Am J Epidemiol 178, 38–45 (2013).
Kim, W. G. et al. Thyroid Stimulating Hormone Reference Range and Prevalence of Thyroid Dysfunction in the Korean Population: Korea National Health and Nutrition Examination Survey 2013 to 2015. Endocrinol Metab (Seoul) 32, 106–114 (2017).
Fedchuk, L. et al. Performance and limitations of steatosis biomarkers in patients with nonalcoholic fatty liver disease. Aliment. Pharmacol. Ther. 40, 1209–1222, https://doi.org/10.1111/apt.12963 (2014).
Papagianni, M., Sofogianni, A. & Tziomalos, K. Non-invasive methods for the diagnosis of nonalcoholic fatty liver disease. World J Hepatol 7, 638–648 (2015).
Lonardo, A. et al. Epidemiological modifiers of non-alcoholic fatty liver disease: Focus on high-risk groups. Dig Liver Dis 47, 997–1006 (2015).
Ballestri, S. et al. Ultrasonographic fatty liver indicator detects mild steatosis and correlates with metabolic/histological parameters in various liver diseases. Metabolism 72, 57–65 (2017).
Meffert, P. J. et al. Development, external validation, and comparative assessment of a new diagnostic score for hepatic steatosis. The American journal of gastroenterology 109, 1404–1414 (2014).
Shen, Y.-N. et al. External validation of non-invasive prediction models for identifying ultrasonography-diagnosed fatty liver disease in a Chinese population. Medicine 96 (2017).
Boucai, L., Hollowell, J. G. & Surks, M. I. An approach for development of age-, gender-, and ethnicity-specific thyrotropin reference limits. Thyroid 21, 5–11 (2011).
Grundy, S. M. et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 112, 2735–2752 (2005).
Alberti, K., Zimmet, P. & Shaw, J. IDF Epidemiology Task Force Consensus Group. The metabolism syndrome-A new worldwide definition. Lancet. 366, 1059–62 (2005).
Acknowledgements
This work was supported by the Korean Thyroid Association Outstanding Investigator Award 2015. The consultation for statistical analysis was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health & Welfare, Republic of Korea.
Author information
Authors and Affiliations
Contributions
J.L. and M.H.K. were responsible for the conception. M.H.K. conceived and coordinated this study. J.L., J.H., K.J., J.M.L., S.-A.C. and M.H.K. designed the research. J.L., J.H., K.J. and M.H.K. performed the data analysis. J.L. and M.H.K. drafted the manuscript. J.L., J.H., K.J., D.J.L., J.M.L., S.-A.C., M.-I.K., B.Y.C. and M.H.K. participated in interpretation of the findings. All authors reviewed and commented on the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, J., Ha, J., Jo, K. et al. Male-specific association between subclinical hypothyroidism and the risk of non-alcoholic fatty liver disease estimated by hepatic steatosis index: Korea National Health and Nutrition Examination Survey 2013 to 2015. Sci Rep 8, 15145 (2018). https://doi.org/10.1038/s41598-018-32245-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-32245-0
Keywords
This article is cited by
-
Polymorphisms within DIO2 and GADD45A genes increase the risk of liver disease progression in chronic hepatitis b carriers
Scientific Reports (2023)
-
Characteristics of coronary artery disease in patients with subclinical hypothyroidism: evaluation using coronary artery computed tomography angiography
BMC Cardiovascular Disorders (2021)
-
Molecular functions and clinical impact of thyroid hormone-triggered autophagy in liver-related diseases
Journal of Biomedical Science (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.