Abstract
The aims of this study were to establish guidelines for the surgical occlusion setup of surgery-first orthognathic surgery, and evaluate the resulting characteristics and accuracy. Skeletal Class III patients (N = 53) underwent Le Fort I osteotomy and bilateral sagittal split osteotomy. Study models before orthognathic surgery were set according to the guidelines. Occlusion was measured and computer-aided surgical simulation was used to evaluate the characteristics and accuracy of the surgical occlusion. The mean age of participants was 25 ± 6 years with 24 males and 29 females. The occlusion was set as positive overjet (4.4 ± 2.0 mm) and overbite (1.4 ± 1.8 mm), Class II or I molar relation, and posterior cross bite (overjet: 4.9 ± 2.0 mm and 4.4 ±1.9 mm, respectively for the right and left second molars) and open bite (overbite: −2.0 ± 1.6 mm and −1.9 ± 1.3 mm, respectively for the right and left second molars). Normal jaw relationship and symmetry were noted after virtual surgery. None of the patients required new occlusal setup. Our data contribute the use of the surgery-first approach for skeletal Class III patients by establishing guidelines for a surgical occlusion setup in three dimensions.
Similar content being viewed by others
Introduction
Before the 1960s, most orthognathic surgeries were performed either without orthodontic treatment after removing the orthodontic appliances, or before any orthodontic treatment. Later, the three stages of classic surgical orthodontic treatment became popular because of the stability of the results and satisfaction with the post-treatment outcomes1. The 3-stage approach requires a variable length of presurgical orthodontic preparation to decompensate the malocclusion, which is followed by surgical correction of the skeletal discrepancy and a relatively short period of postsurgical orthodontics for detailing and finishing of the occlusion. Presurgical orthodontics typically includes dental alignment, incisor decompensation, arch leveling and coordination, and usually requires 15 to 24 months2,3. However, this exacerbates facial esthetics and dental function, and causes significant patient discomfort before surgery2. One study found that one third of patients rated the orthodontics as the worst part of their orthognathic treatment owing to the appliances’ visibility and discomfort, and the length of treatment4.
The longer treatment time and transitional detriment to the facial esthetics and dental function associated with presurgical orthodontics have led to a new approach called “surgery-first”, which eliminates the presurgical orthodontic phase5,6,7,8,9. The orthognathic surgery-first approach is becoming popular because of several advantages such as reduced treatment time, efficient tooth decompensation, and early improvement in facial esthetics, especially in Class III malocclusion5,6,8,9,10. These advantages have a very positive influence on patients’ global satisfaction with treatment.
The most difficult step for the surgery-first approach is the setup of the transitional occlusion at the time of surgery (i.e., surgical occlusion). There are some reports showing guidelines for surgical occlusion setup for surgery-first approach in Class III malocclusion7,8,11,12,13. However, the guidelines are rather crude; that is, dental occlusion is proposed in the antero-posterior dimension only8,11,13,14 and, in addition, there are no data available on the occlusal characteristics or accuracy. Accurate surgical occlusion setup is important to avoid severe postoperative occlusal instability, incomplete or excessive skeletal correction, or skeletal asymmetry (i.e., skeletal deformity). Currently, 3D virtual simulation process allows us to assess the accuracy of occlusion setup in terms of skeletal deformity. Thus, we conducted this study to establish guidelines for surgical occlusion setup, and to investigate the characteristics and accuracy of the surgical occlusion.
Results
The 53 patients enrolled in the study were comprised of 24 males and 29 females; mean age was 25 ± 6 years. Genioplasty was performed on 39 patients (Table 1). Thirty-nine patients (74%) had occlusal contact on three segments. The average number of tooth contact was 5.2 ± 2.3 (Table 2). Positive overjet (mean 4.4 ± 2.0 mm) and overbite (mean 1.4 ± 1.8 mm), Class II or I molar relation, and posterior cross bite (buccal overjet: mean 4.9 ± 2.0 mm and 4.4 ±1.9 mm, respectively for the right and left molars) and open bite (buccal overbite: mean −2.0 ± 1.6 mm and −1.9 ± 1.3 mm, respectively for the right and left molars) on second molars were determined at setup (Table 3). Normal jaw relationship (ANB: mean 2.1 ± 1.8 degrees) and symmetry was noted after virtual surgery (Table 4). None of the patients required new occlusal setup due to significant skeletal deformity. There were no differences in characteristics and accuracy of surgical occlusion as well as jaw relation and symmetry after virtual surgery between patients who received genioplasty and those who did not receive genioplasty (Tables 1 through 4).
Discussion
Despite the distinct advantages of the surgery-first approach, there has been no conclusive data regarding variables required for the surgical occlusion setup. To our knowledge, this is the first study to quantify the surgical occlusion setup for a surgery-first approach and subsequently evaluate the accuracy of the setup. We found that the majority of occlusion setups had contact on three segments, and the accuracy of the setup was excellent. Our data contribute the use of the surgery-first approach for skeletal Class III patients by establishing guidelines for a surgical occlusion setup in three dimensions.
The goal of surgery-first is to achieve normal skeletal relationship in three dimensions, skeletal symmetry in six planes of space and facial harmony. The surgical occlusion setup serves to foresee the tooth movements necessary to achieve an ideal occlusion after postsurgical orthodontic treatment. This is similar to the process that the orthodontist performs to correct any malocclusion of skeletal Class I, because skeletal deformity is corrected from the start. Because dental alignment, arch leveling and coordination, and incisor decompensation are deferred after surgery with the surgery-first approach, a major consideration for the surgical occlusion setup is to compensate for the space required for the dental movement. However, the previous guidelines have been rudimentary; that is, dental occlusion was proposed in the antero-posterior dimension only. For example, previous reports suggest the use of first molars as a guide for antero-posterior dental position8,11,13,14, which is similar to our guidelines. Because the compensation of horizontal mandibular relapse is planned for with a 2-mm overcorrection8, the Class II molar relationship is often set in our occlusion setup. Similarly, it is not surprising to note relatively large overjet (mean 4.4 ± 2.0 mm) in our occlusion setup as incisor decompensation is deferred after surgery.
The vertical dimension in our guidelines suggest deep overbite or posterior open bite for preventing bite opening from dental alignment and arch leveling after surgery as described previously15,16. The posterior open bite is easier to correct than anterior open bite after surgery; therefore, surgical occlusion setup with anterior open bite should be avoided. The posterior open bite is also helpful for correction of posterior cross bite from buccoversion of maxillary second molars, which is quite common in Class III malocclusion, due to unlocked occlusion.
Although a number of studies suggest no posterior cross bite at setup7,11,13, our guidelines in the transverse dimension emphasize the coordination of jaw midlines instead of dental arch to avoid positional jaw asymmetry. Posterior cross bite at setup appears in some cases of Class III malocclusion. It is mandatory to note whether it is skeletal or dental in nature. Orthodontic correction by archwire bending, inter- or intra-arch elastics, transpalatal arch or lingual arch is suggested in cases of dental cross bite or mild skeletal cross bite. On the other hand, segmental surgery or surgically assisted rapid palatal expansion is only indicated in patients with severe skeletal cross bite. Similarly, the posterior open bite at setup is also helpful for correction of posterior cross bite due to unlocked occlusion
It has been argued that stable occlusion at the time of surgery is important in postoperative stability5,6,7,12. However, the definition of stable occlusion varied between at least 3-point contact [7, 12] and stable posterior occlusion5,6. Our results indicate that stable occlusion can be achieved by occlusal contact on 5 to 6 teeth or occlusal contact on not only three segments but also on two or one (i.e., anterior) segments. Similarly, the posterior open bite at setup is also helpful to avoid severe postoperative occlusal instability from imperfect occlusal interdigitation, as described earlier.
In conclusion, the surgical occlusion for correction of skeletal Class III deformity using the surgery-first approach was set with positive overjet and overbite, Class II or I molar relation, and posterior cross bite and open bite. On average, there was occlusal contact on five to six teeth; most surgical occlusion setups had contact on three segments. The accuracy of the occlusion setup according the guidelines was excellent. Further studies are required to confirm the generalization of the guidelines to different types of dentofacial deformity.
Patients and Methods
The study was conducted in accordance with the World Medical Association Declaration of Helsinki on medical research ethics. The approval of the study was granted by the Ethics Committee for Human Research at the Chang Gung Memorial Hospital in Taoyuan, Taiwan. Patients were included in the study if they met the following criteria: age ≥ 18 years; diagnosed with skeletal Class III deformity (ANB ≤ 0°) and no significant facial asymmetry (Menton deviation < 4 mm); surgical occlusion setup and computer-assisted surgical design conducted by a single experienced orthodontist; and received Le Fort I 1-piece osteotomy and bilateral sagittal split rotational setback with or without genioplasty using rigid internal fixation, and no intermaxillary fixation after surgery at Chang Gung Craniofacial Center, Taoyuan, Taiwan. Patients with one or more of the following criteria were excluded: a genetic syndrome or other congenital deformity; history of facial bone surgery; or mental retardation. A total of 53 patients were eligible for the study and were invited to participate.
Guidelines for initial surgical occlusion setup
In the setup of surgical occlusion, it is important to decide (1) where to place the teeth antero-posteriorly, vertically, and transversely; and (2) how to position these teeth or tooth segments either surgically or orthodontically in order to achieve facial and dental esthetics, and maximize the efficacy and speed of treatment (i.e., simplify the orthodontic treatment after surgery). The guidelines used for occlusion setup are detailed below.
Sagittal relationship
When conducting a surgery-first approach, incisors cannot be used as a guide for antero-posterior jaw positioning (i.e., incomplete horizontal skeletal correction), unlike classic surgical-orthodontic treatment, in which incisor decompensation is performed before surgery. Instead, molars are the guide to antero-posterior jaw positioning. The molar relationship can be either Class I, II or III, depending on the tooth number ahead of molars. When there is a need for compensation of horizontal skeletal relapse, 2 mm overcorrection is often designed.
Vertical relationship
Because dental alignment and arch leveling is deferred after surgery with the surgery-first approach, a major consideration for the occlusion setup in the vertical dimension is to compensate for the space required for the dental alignment and arch leveling. Since dental alignment and arch leveling lead to proclination of the lower incisors and downward rotation of the mandible, thus decreasing the incisor overbite, the occlusion is set in deep overbite or posterior open bite. However, insufficient chin throat length (i.e., excessive horizontal skeletal correction) appears in some cases following bimaxillary rotational setback surgery8,17. It is mandatory to increase the posterior open bite by closing rotation of the osteotomized mandibular segment (i.e., distal segment), with the axis of rotation being the mandibular canines or premolars. However, the amount of posterior open bite resulting from this closing rotation should be within the limit of orthodontic tooth movement (<10 mm)8.
Transverse relationship
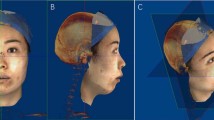
Because arch coordination is deferred after surgery with the surgery-first approach, the occlusion setup in the transverse dimension often poses a significant challenge. A major consideration for the surgical occlusion setup in the transverse dimension is to achieve jaw symmetry. To prevent positional asymmetry, the maxillary and mandibular jaw (alveolar base) midlines must be coincident or close to it (Fig. 1).
Stable occlusion
Because dental alignment, arch leveling and coordination are deferred after surgery with the surgery-first approach, perfect occlusal interdigitation often cannot be achieved due to occlusal interference when performing model setup. To avoid severe postoperative occlusal instability, orthodontists can remove occlusal interference by simple occlusal adjustment in mild cases and opening the bite in more severe cases. Orthodontists can also perform limited orthodontic treatment (i.e., dental alignment) before surgery to remove severe occlusal interference precluding stable surgical occlusion.
Dental midline
Dental alignment is deferred after surgery with the surgery-first approach, therefore the surgical occlusion is sometimes set with dental midline off due to dental arch asymmetry. That is, surgical occlusion is set as coordination of jaw midlines instead of dental midlines.
Contact distribution of surgical occlusion
One month before surgery, the patient’s maxillary and mandibular dental casts were scanned with a 3-dimensional (3D) laser surface scanner (3Shape, Copenhagen, Denmark). Surgical occlusion was then set according to the guidelines described above (initial occlusion setup) and scanned with the same 3D laser surface scanner.
Contact distribution of the surgical occlusion was measured using AVIZO version 7.0 software (FEI, Mérignac, France). The occlusal contact was defined as interocclusal distance being 0.5 mm or less and projected to the maxillary arch. The maxillary arch was divided into three segments: anterior, posterior right, and posterior left. Contact distribution was categorized as contact on three segments (anterior, posterior right, and posterior left), two segments (anterior and posterior right, anterior and posterior left, or posterior right and posterior left), or one segment (anterior, posterior right, or posterior left). Position of tooth contact (anterior, premolar, or molar) was also recorded (Fig. 2).
Characteristics and accuracy of surgical occlusion
To determine the characteristics and accuracy of the surgical occlusion setup, one month before surgery cone-beam computed tomography of the head and neck was performed for each patient using an i-CAT 3D Dental Imaging System (Imaging Sciences International, Hatfield, Pa.). Patients were scanned during wakefulness with the following parameters: 120 kVp, 0.4 × 0.4 × 0.4-mm voxel size, 40-second scan time, and 16 × 16-cm field of view. The patient’s head was positioned with the Frankfort horizontal plane parallel to the ground. Throughout the scan, patients were instructed not to swallow, to keep their mouth closed, and to maintain a centric occlusion bite. Images were stored in Digital Imaging and Communications in Medicine format and rendered into volumetric images using Simplant OMS (Materialise, Leuven, Belgium). For a more accurate dental surface, the dental arches were replaced by scanned dental cast images. After defining Le Fort I and bilateral sagittal split osteotomy planes, the head images were reoriented according to the clinical measurements and cranial symmetry as well as Frankfort horizontal plane.
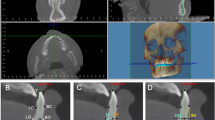
Before virtual simulation, the surgical occlusion was transferred by moving the mandible to the fixed maxilla. Subsequently the maxillary and mandibular osteotomized segments were then moved as one united maxillo-mandibular complex according to the planning principles while maintaining the surgical occlusion8. That is, 3D simulation moved the maxillo-mandibular complex in the three dimensions until a normal jaw relationship and symmetry was achieved. When there was any significant skeletal deformity (often excessive horizontal skeletal correction or positional asymmetry due to incorrect initial occlusion setup), a new surgical occlusion was then set until deformity was corrected (final occlusion setup). The accuracy of the surgical occlusion was thus determined by calculating the incidence of the two setups. Virtual outcome regarding jaw relationship (i.e., ANB angle) and symmetry (i.e., midline deviation and mandibular body symmetry) were also calculated (Figs 3 and 4).
Computed tomography images used for linear and angular measurements of jaw symmetry. (Left) Horizontal deviation for maxilla (anterior nasal spine and upper incisor) and mandible (lower incisor and menton); ANS, anterior nasal spine; UI: upper incisor; LI: lower incisor; Me: menton. (Center) Vertical discrepancy for mandible (distance between point R and point L); point R: inflection point of mandibular body at the level of right mental foramen; point L: contralateral corresponding point of mandibular body on the left side. (Right) Horizontal discrepancy for mandible (distance discrepancy between dr and dl); dr: distance from point R to the facial midsagittal plane; dl: distance from point L to the facial midsagittal plane.
Characteristics of the surgical occlusion were assessed using linear measures to depict overjet and overbite, buccal overjet and overbite on second molars, and dental midline discrepancy. Angle molar relation (Class I, II, or III) was also recorded.
Error of study
The error of the method was assessed through repetitive measuring of 10 randomly selected patients at least 1 week apart by the same investigator. The measurement error, evaluated using intraclass correlation coefficient (ICC), was excellent (mean ICC, 0.997; 95 percent confidence interval, 0.969 to 0.999).
Statistical analysis
Data were analyzed using the statistical package SPSS (Version 17.0; SPSS, Inc., Chicago, Ill.). Unless otherwise specified, data are presented as the mean ± standard deviation (SD). Statistical analysis was carried out using the paired t-test, the Wilcoxon signed ranks test, the Mann-Whitney U test, or the chi-square test. All tests were two-tailed, with statistical significance set at p < 0.05.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on request.
References
Proffit, W. R., White, R. P. & Sarver, D. M. Combining surgery and orthognathics: Who does what, when? Contemporary Treatment of Dentofacial Deformity (ed. Proffit, W.R., White, R.P., Sarver, D.M.) 245–267 (Mosby, 2003).
Luther, F., Morris, D. O. & Hart, C. Orthodontic preparation for orthognathic surgery: How long does it take and why? A retrospective study. Br J Oral Maxillofac Surg. 41, 401–406 (2003).
Diaz, P. M. et al. Time used for orthodontic surgical treatment of dentofacial deformities in white patients. J Oral Maxillofac Surg 68, 88–92 (2010).
Nurminen, L., Pietilä, T. & Vinkka-Puhakka, H. Motivation for and satisfaction with orthodontic-surgical treatment: A retrospective study of 28 patients. Eur J Orthod. 21, 79–87 (1999).
Nagasaka, H., Sugawara, J., Kawamura, H. & Nanda, R. “Surgery first” skeletal Class III correction using the Skeletal Anchorage System. J Clin Orthod. 43, 97–105 (2009).
Villegas, C., Uribe, F., Sugawara, J. & Nanda, R. Expedited correction of significant dentofacial asymmetry using a “surgery first” approach. J Clin Orthod 44, 97–103 (2010).
Baek, S. H., Ahn, H. W., Kwon, Y. H. & Choi, J. Y. Surgery-first approach in skeletal Class III malocclusion treated with 2-jaw surgery: Evaluation of surgical movement and postoperative orthodontic treatment. J Craniofac Surg. 21, 332–338 (2010).
Liao, Y. F. et al. Presurgical orthodontics versus no presurgical orthodontics: Treatment outcome of surgical-orthodontic correction for skeletal class III open bite. Plast Reconstr Surg. 126, 2074–2083 (2010).
Hernandez-Alfaro, F., Guijarro-Martınez, R., Molina-Coral, A. & Badía-Escriche, C. “Surgery first” in bimaxillary orthognathic surgery. J Oral Maxillofac Surg. 69, e201–e207 (2011).
Liou, E. J. et al. Surgery-first accelerated orthognathic surgery: postoperative rapid orthodontic tooth movement. J Oral Maxillofac Surg. 69, 781–785 (2011).
Liou, E. J. et al. Surgery-first accelerated orthognathic surgery: orthodontic guidelines and setup for model surgery. J Oral Maxillofac Surg 69, 771–780 (2011).
Kim, C. S. et al. Stability of mandibular setback surgery with and without presurgical orthodontics. J Oral Maxillofac Surg 72, 779–787 (2014).
Yu, H. B. et al. The surgery-first approach in orthognathic surgery: a retrospective study of 50 cases. Int J Oral Maxillofac Surg. 4, 1463–1467 (2015).
Park, K. R., Kim, S. Y., Park, H. S. & Jung, Y. S. Surgery-first approach on patients with temporomandibular joint disease by intraoral vertical ramus osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol 116, e429–e436 (2013).
Ko, E. W. et al. Comparison of progressive cephalometric changes and postsurgical stability of skeletal Class III correction with and without presurgical orthodontic treatment. J Oral Maxillofac Surg. 69, 1469–1477 (2011).
Park, H. M., Lee, Y. K., Choi, J. Y. & Baek, S. H. Maxillary incisor inclination of skeletal Class III patients treated with extraction of the upper first premolars and two-jaw surgery: Conventional orthognathic surgery vs surgery-first approach. Angle Orthod. 84, 720–729 (2014).
Hsieh, Y. J. et al. Effect of bimaxillary rotational setback surgery on upper airway structure in skeletal Class III deformities. Plast Reconstr Surg 135, 361e–369e (2015).
Acknowledgements
The work was supported by the Ministry of Science and Technology, Taiwan (MOST105-2314-B-182-030) and the Chang Gung Memorial Hospital, Taiwan.
Author information
Authors and Affiliations
Contributions
Yu-Fang Liao: Study design, data collection, statistical analysis, writing the article. Shu Hsien Lo: data collection, statistical analysis, writing the article.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liao, YF., Lo, S.H. Surgical Occlusion Setup in Correction of Skeletal Class III Deformity Using Surgery-First Approach: Guidelines, Characteristics and Accuracy. Sci Rep 8, 11673 (2018). https://doi.org/10.1038/s41598-018-30124-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-30124-2
This article is cited by
-
Three-dimensional positioning of the maxilla using novel intermediate splints in maxilla-first orthognathic surgery for correction of skeletal class III deformity
Clinical Oral Investigations (2024)
-
Skeletal stability after bimaxillary surgery with surgery-first approach for class III asymmetry is not related to virtual surgical occlusal contact
Clinical Oral Investigations (2022)
-
Comparative stability and outcomes of two surgical approaches for correction of class III asymmetry with lip or occlusal cant
Clinical Oral Investigations (2021)
-
Large versus small mandibular counterclockwise rotation during bimaxillary surgical correction of class II deformities—a retrospective CBCT study on skeletal stability
Clinical Oral Investigations (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.