Abstract
The growing drug resistance (DR) raises major concerns for the control of visceral leishmaniasis (VL), a neglected disease lethal in 95 percent of the cases if left untreated. Resistance has rendered antimonials (SSG) obsolete in the Indian Sub-Continent (ISC) and the first miltefosine-resistant Leishmania donovani were isolated. New chemotherapeutic options are needed and novel compounds are being identified by high-throughput screening (HTS). HTS is generally performed with old laboratory strains such as LdBOB and we aimed here to validate the activity of selected compounds against recent clinical isolates. In this academic/industrial collaboration, 130 compounds from the GSK “Leishbox” were screened against one SSG-sensitive and one SSG-resistant strain of L. donovani recently isolated from ISC patients, using an intracellular assay of L. donovani-infected THP1-derived macrophages. We showed that only 45% of the compounds were active in both clinical isolates and LdBOB. There were also different compound efficiencies linked to the SSG susceptibility background of the strains. In addition, our results suggested that the differential susceptibility profiles were chemical series-dependent. In conclusion, we demonstrate the potential value of including clinical isolates (as well as resistant strains) in the HTS progression cascade.
Similar content being viewed by others
Introduction
Leishmaniasis is a neglected tropical disease caused by parasites of the genus Leishmania1. It occurs in several parts of the world under different clinical forms, the most severe being visceral leishmaniasis (VL), also known as kala-azar; a systemic illness that is lethal if left untreated. Every year, 200,000–400,000 new cases of VL happen, due to parasites of the L. donovani complex, essentially in India, Nepal, Bangladesh, Sudan, Ethiopia and Brazil, with a mortality estimated at 10%1. In the Indian sub-continent (ISC) a regional program aiming for the elimination of VL (Kala-Azar elimination program or KAEP) is currently running, based on two major pillars, vector control and chemotherapy2.
Currently, there are only few therapeutic options for leishmaniasis and they have various drawbacks3. Pentavalent antimonials (SSG) were used for decades, but they are limited by toxicity and treatment failure (TF) primarily caused by resistant parasites. This led to the progressive withdrawal of SSG in the Indian Sub-Continent (ISC) since 20054. At that time, SSG was replaced by Miltefosine (MIL), the first oral treatment available for leishmaniasis5. However the use of MIL is being threatened by the alarming rise of TF in the ISC6 and recently, the first MIL-resistant strains were detected in the field7. The development of a liposomal form of Amphotericin B (Ambisome) has reduced its toxicity but its availability to patients is restricted by high costs8. Preferential pricing agreement increased access to Ambisome and a single-dose treatment is now used as the first line treatment in the ISC9. Combination therapies are used as an alternative, but this strategy might be questioned, when one of the composing drug is starting to fail (like MIL); in addition, experimental work has shown that L. donovani resistant to combined drugs could easily be selected in vitro10. Currently there are no other drugs available, and new compounds, formulations or combinations are urgently needed.
High-throughput screening (HTS) is an efficient way of identifying active compounds11,12 able to eliminate the parasite without affecting the host. Whole-cell phenotypic HTS is used for anti-leishmania drug discovery because of the low number of molecular targets well characterized and validated13. The parasite life stage used for screening is of utmost importance and intracellular amastigotes have been recognized as the ideal model14. High content image analysis can be incorporated in the screen to quantify changes in cellular phenotype, which is called high content screening (HCS). The first HCS/HTS using intracellular amastigotes infecting human macrophages was reported in 201015 and since then, improvements of HTS protocols have been continuously carried out to reach a good balance of practicality, reproducibility and biological relevance. L. donovani BOB strain (LdBOB, MHOM/SD/62/1S-CL2D) has been the strain of choice for many HTS campaigns16,17,18. It is a clone of Ld1S2D, an East African strain isolated in 1962, that has been maintained in laboratories over the world for decades19. It is of utmost importance to check whether compounds, which are active against laboratory-adapted strains like LdBOB, will be equally active against clinical isolates that may differ genetically and phenotypically (virulence, drug resistance…). This approach, albeit well established in drug discovery against other pathogens, is not common in the Leishmania community and was recently recommended3.
Recently, GlaxoSmithKline (GSK) has carried out a HTS on a diversity set of 1.8 million compounds through whole-cell phenotypic assays against wild type and eGFP-engineered LdBOB. This generated the “Leishbox” comprising 192 compounds with anti-leishmania activity18. We aimed here to explore the relevance of clinical isolates in the further validation of these compounds. For this proof-of-principle study, we selected two clinical isolates of L. donovani from our ISC collection, respectively sensitive and resistant to SSG and we included them in the screening assay. We show here that 45% of the tested compounds of the Leishbox were pan-active, while 55% were inactive in one or the other clinical isolates. These results demonstrate the importance of a secondary screening with clinical isolates, in support to the selection process and profiling of the hits that can proceed further in the drug discovery pipeline.
Results
Optimization of the HCA for clinical isolates
The InMac assay developed by GSK was modified by the incorporation of horse serum which increased the robustness and the predictive potential of the assay by reducing the amount of extracellular promastigotes remaining after infection17. Moreover, it avoided the reinfection and increased the replication rate of intracellular amastigotes17. The assay was further optimized for the clinical isolates LdBPK_282 and LdBPK_275 (procedure described in Fig. 1).
Experimental setup and analysis parameters of the InMAC assay. THP-1 cells are differentiated for 24 hrs followed by o/n infection with d7 promastigotes. Infected THP-1 cells are plated and incubated with the “Leishbox” compounds and controls for 96 hrs. Finally plates are stained with Draq5, read and analysed. Images were taken by Opera at 40x magnification. The infected cells are shown in red while the non-infected ones are shown in green.
The infection with clinical isolates provided various challenges. A multiplicity of infection (MOI) of 30 was needed to achieve a satisfactory infection level (compared to an MOI of 10 in case of LdBOB). Infections reached a maximum of 55% of infected cells in the case of LdBPK_275 and 44% in the case of LdBPK_282 compared to almost 90% of infected cells with LdBOB. There was also a slight variability in the number of amastigotes per macrophage with an average value of 3.2 for LdBPK_275, 2.7 for LdBPK_282 and 3 for LdBOB. Despite these challenges, the results obtained with drugs used in clinical practice were consistent with the previously reported values, hereby validating the sensitivity of the system (Fig. 2). Amphotericin B showed activity against both clinical isolates. The measured IC50 was 0.25 μM in LdBPK_282 (pIC50 6.6) and 0.316 μM in LdBPK_275 (pIC50 6.5). In literature20 the IC50 reported for amphotericin B against L. donovani was 0.1 to 0.4 μM (pIC50 7 to 6.4, respectively). For MIL, the obtained IC50 values were 2.95 μM in LdBPK_282 (pIC50 5.53) and 3.58 μM in LdBPK_275 (pIC50 5.45) while the values reported in literature were 0.9 to 4.3 μM (pIC50 6.04 to 5.36, respectively)20. In addition to these two gold standards, 22 control compounds were included for each run, these compounds belong to internal drug discovery programs and have different modes of action and potency ranges. The correlation between historic LdBOB data and the 2 clinical isolates was excellent. For this assay and based on these compounds, Minimum Discriminatory Difference (MDD)21 was 0.36, which gives confidence in the quality of the replicates. Regarding the reproducibility and the quality of the assay, even though the Z’ values were low for both strains, the automated imaging assay for wild type clinical isolates had enough statistical significance to evaluate the activity of compounds in dose-response. Finally, screening of the “Leishbox” was run in duplicate obtaining excellent correlations for the 2 copies. Calculated MSD (minimum significant difference) as the average of 2*SD of all the compounds tested is 0.4, a value which is within the acceptable range reported by other authors22.
Quality control of the InMac Assay. (A) A 40x magnification image from Opera of 96 h Amphotericin B dose response curve (0.1 μM to 16 μM) of THP-1 infected with LdBPK_275 in the upper panel and LdBPK_282 in the lower panel at MOI 30, cells are stained with Draq5. (B) Dose response curves for Amphotericin B and Miltefosine for LdBPK_275 in the upper panel and LdBPK_282 in the lower panel; the concentration is represented on the X-axis (M) and the response on the Y-axis. The amastigote/macrophage (AM/MAC) readout is represented in blue and macrophage (MAC) readout in yellow.
Activity of “Leishbox” compounds against L. donovani clinical isolates
A set of 130 compounds from the “Leishbox” was selected based on availability (Table 1). The compounds’ activity against LdBPK_282 and LdBPK_275 was tested and compared to their documented values against LdBOB (values obtained after incorporation of horse serum in the assay as described elsewhere23). The results shown are the pIC50 values as calculated from the amastigote per macrophage readout (AM/MAC). Ten compounds lost their activity against LdBOB after the assay modification and addition of horse serum. The remaining 120 compounds were then classified into 4 categories, from I to IV (Fig. 3). Compounds that show activity in the three strains of L. donovani fall in category I (pan-active compounds: 45%). Compounds that lose activity in both clinical isolates fall in category II (25%). While those that show activity in LdBOB and LdBPK_282 (SSG-S) only are in category III (8.33%), and those active only in LdBOB and LdBPK_275 (SSG-R) are in category IV (21.66%). Among the 10 compounds that lost activity with LdBOB, 2 showed activity against one of the clinical isolates: they formed category V. The final set of compounds (8) did not show activity against any of the tested strains (category VI).
Differential efficacy of compounds of the leishbox on the different LD strains. A-C Correlation of the pIC50 values calculated from the AM/MAC readout, inactive compounds are represented with pIC50 of 4.3 (corresponding to an IC50 of 50 μM). (A) SSG-S vs LdBOB. (B) SSG-S vs SSG-R. (C) SSG-R vs LdBOB. Compounds are colour coded based on their categories (I-VI). (D,E) The percentage of compounds per category. (D) Representation of the six categories of the 130 compounds. (E) Representation of the 120 compounds active against LdBOB (categories I-IV).
Chemical analysis of the “Leishbox” compounds results
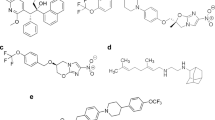
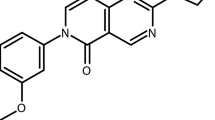
The results of the screening were analysed in function of the chemical structure of the compounds and their hypothetical targets (Table 2 and Fig. 4). Compounds were grouped on the basis of common substructures using Helium as the cheminformatics toolkit that provides search by substructure within a table (the “Leishbox” in this case) through SMILES data, which resulted in the delineation of 13 chemical clusters with at least two members and 68 singletons. Interestingly, compounds of the same chemical cluster generally showed similar activity versus the strains used and at least 50% of the members of each cluster presented the same activity profile (Fig. 4). Clusters 1 to 8 included pan-active compounds (category I), clusters 9, 10 and 11 included compounds which are more active against LdBPK_275 and LdBOB than against LdBPK_282 (category IV), clusters 12 and 13 included the compounds that lost activity in the assay with clinical isolates (category II). For category III (active only on LdBPK_282 and LdBOB
), compound TCMDC-143521 was found in cluster 6 and compound TCMDC-143573 was found in cluster 12. The most active compound in category III was the singleton TCMDC-143239.
Chemical clustering of tested compounds. On the X axis pIC50 of LdBPK_282 and on the Y axis pIC50 of LdBPK_275. Compounds from the “Leishbox” were visually grouped on the basis of common substructures resulting in 13 clusters with at least 2 members and 68 singletons. For each cluster at least 50% of the compounds have the same biological behaviour. (A) Pan-active compounds, cluster 1 to 8. (B) Cluster 9, 10 and 11 includes compounds selective to SSG-R and Cluster 12 and 13 were inactive. A plot with 68 singletons was included to illustrate the data. The two most active singletons were commented in the text and marked and labelled in the figure.
Discussion
In a recent opinion paper3, we highlighted that most HTS were done using a single reference strain like LdBOB, a strain isolated in Sudan in 1962 and since then maintained for decades in several laboratories. This strain is particularly adapted for HTS, because of its ability to grow and infect macrophages in vitro. However, considering (i) its status of ‘laboratory-adapted’ strain, (ii) the big genomic differences existing between L. donovani from East Africa and from the Indian sub-continent24 and (iii) the reported differences in treatment efficacy between East Africa and ISC25, it is currently unknown whether/how LdBOB is representative of clinical isolates and parasites from different geographical regions, in terms of drug susceptibility. Therefore, it was recommended to add clinical isolates to the screening cascade following the primary HTS process, including drug-resistant ones3.
The present study is the first experimental validation of this recommendation, with a specific emphasis on the ISC. The two Nepalese strains used here were isolated from VL patients in 2003, maintained for a maximum of 45 passages in vitro and showing different susceptibility to SSG. Using clinical isolates has generally been avoided in HTS because of the difficulty of achieving high quality infections in vitro. Several factors can reduce the quality of the infection including the excess of extracellular promastigotes, which can interfere with the efficacy of the analysis, especially for compounds that are active only on intracellular stages. However addition of horse serum (HS) as recommended by the recent study17 proved to be a good strategy. Another factor could be the lower in vitro infectivity of clinical isolates of L. donovani; in the present study, a higher MOI was needed, but it still resulted in a lower percentage of infected cells (around 50%) than in the case of LdBOB (around 90%). However, these infection levels were sufficient to obtain reliable results and our quality controls validated the sensitivity of the system in terms of the pharmacology response. Moreover, the obtained data for activity of MIL and Amphotericin B fully agreed with the values reported in literature.
We reported here that out of 120 compounds active on LdBOB (i) 45% were also active on the two clinical isolates, independently of their SSG susceptibility (pan-active), (ii) 25% lost their activity on the two clinical isolates, (iii) while 21.7 and 8.3% were only active on the SSG-R and the SSG-S clinical isolate, respectively. Only 2 compounds were active on one clinical isolate and inactive on LdBOB, hereby supporting the further use of LdBOB for primary screening. However, our results strongly confirm the interest of introducing clinical isolates at a second stage of screening. The obvious next question now concerns the implications of these results in an R&D context: should pan-active compounds be prioritized in the pipeline and what should be done with the compounds inactive on one or more clinical isolates?
To answer this question a wide panel of strains, which provides a true representation of the actual clinical setting in the world will be essential. For visceral leishmaniasis, and taking into account genomic and phenotypic diversity, clinical isolates of the following species/variants should be taken into consideration: L. donovani from ISC, L. donovani from East Africa and L. infantum. For each of them, wild-type as well as strains resistant to drugs currently in use should be included (ideally clinically resistant; if not experimentally selected). This will rapidly give a significant number of lines and the next question will be to make these compatible with the secondary screening or could be part of a final validation step. Finally, such sets of well-characterized strains with regards to the genome and the metabolome, should be gathered and distributed to potential users.
Pan activity should be prioritized and, if there is specific susceptibility of some strains, the compounds should at least cover all strains of a particular geographical population. Since development costs are huge, “personalized” or segmented medicines for VL are not feasible so there is not enough value in a drug candidate that covers only a segment of population at risk.
At the current stage, it is impossible to know if the absence of activity of a fifth of the compounds against two clinical isolates of L. donovani from the ISC is due to genetic and phenotypic differences between East African and ISC parasites or to the difference between a laboratory-adapted strain and clinical isolates. Further work including recent clinical L. donovani isolates from East Africa is required, but most likely the two factors must play a role. The differences observed here between the two ISC isolates also deserve a deeper attention. Differences were expected, considering the major functional differences existing between populations represented by both strains, beyond their SSG-susceptibility profiles: differences in (i) capacity for protection against oxidative stress, (ii) fluidity of plasma membrane, (iii) metabolite survival kit and (iv) capacity to up-regulate host IL-10 and to over-express multidrug-resistant protein 1 of the macrophage26,27,28. However, the higher number of active compounds on the SSG-R isolate vs. the SSG-S is surprising, SSG-R parasites being reported to be more virulent and fit, even in the absence of the drug29. At the contrary, the molecular adaptations towards SSG, observed in LdBPK_275 could have made it more sensitive to other drugs. Only 8.3% of the compounds were inactive on the SSG-R strain. As above, further work is required including more SSG-R and SSG-S isolates and those resistant to other drugs used in the field, in order to further document the impact of resistance when screening for new compounds.
An analysis of the data available in the public domain has allowed us to relate the common substructure in chemical clusters with biological features. This result contributed to further validate the specificity of our data. Clusters 1 to 8 included pan active compounds (category I). The first cluster contained eight bi-pyridinyl compounds whose target has been hypothetically identified as a gene related with Nicotinate and nicotinamide metabolism18. The scaffold of pyrimido-pyrimidines has been previously described as DHFR inhibitor mainly for compounds that contain 2,4-diamino substitution in pyrimidine ring (cluster 2)30. The compounds sharing a N-(4-(pyridin-2-yl)thiazol-2-yl) amide in their structure (cluster 3) showed activity in both strains. This chemical feature was previously identified as antimycobacterial31. The compounds of cluster 6 contain a nitro-furane in their structure and 7 out of the 11 compounds were pan active. Nitro drugs are well known to treat parasitic diseases (e.g. nifurtimox, benznidazole, fexinidazole) upon selective activation by parasite nitroreductases32. Clusters 9, 10 and 11 include compounds, which are more active against LdBPK_275 vs. LdBPK_282. Six members of cluster 11 share the N-methyl-4-(1H-pyrazol-1-yl)-1,3,5-triazin-2-amine core that has been previously described as an anti-plasmodium agent33. Singleton TCMDC-143603 also shows a higher activity against LdBPK_275 vs. LdBPK_282 and it contains a primaquine-like structure, a known antimalarial drug. Cluster 12 and 13 included the compounds that have lost their activity in the assay with clinical isolates. The loss of activity of cluster 12, dioxolanes compounds, has been reported in a previous assay with L. donovani using horse serum as supplement in the testing culture media23. However, in the case of cluster 13 (2-(pyridin-2-yl) pyrimidin-4-amines) the absence of activity could be related to the use of clinical isolates instead of laboratory strains. Overall, these results suggest that the differential susceptibility profile against Leishmania strains is more related with the mode of action, thus chemical series-dependent, than with the particular physicochemical features of the compounds.
In conclusion this study resulted from an inter-institutional, academic-industrial collaboration, aiming at improving the drug discovery process for anti-leishmanials. Based on our results, including a multi-strain panel is of utmost importance for the improvement of the preclinical stage of anti-leishmania drug discovery. In particular, in the context of VL chemotherapy, screening should involve recent clinical isolates of the L. donovani complex, with different susceptibility profiles to existing drugs and from different geographical areas. Noteworthy, a similar problem arose in the context of diagnostics of VL. The rK39-based ICT rapid diagnostic test provided high sensitivity and specificity in the ISC and Brazil. Yet it showed to be less sensitive and less specific in sub-Saharan Africa34,35. One explanation was the extensive kinesin genetic diversity identified between strains from East Africa and ISC36. The use of clinical isolates for the validation of HTS can increase the predictive potential of the in vitro assays. It also can eliminate the chance of TF by knowing if the drugs are species-specific, which can facilitate identifying the target population that will benefit from the new anti-leishmania drugs released if they do proceed to further production stages. Diversity of Leishmania is a reality, which must be taken into account in the quest for new tools for diseases control.
Methods
Parasites and mammalian cell cultures
THP-1 cells; (human monocytic leukemia) (ATCC-TIB-202) were provided by the GSK- Biological Reagents and Assay Development Department (BRAD, Stevenage, UK). The THP-1 cells were maintained in RPMI media (Life Technologies) supplemented with 1.25 mM pyruvate (Life Technologies), 2.5 mM glutamine (Life Technologies), and 25 mM HEPES (Life Technologies), and 10% heat-inactivated fetal bovine serum (FBS) (Gibco). Two L. donovani cloned strains: MHOM/NP/03/BPK282/0 clone 4 (SSG-Sensitive/LdBPK_282) passage number R40/17 (meaning 40 passages since original isolation from patient, including 17 passages since cloning) and MHOM/NP/03/BPK275/0 clone 18 (SSG-Resistant/LdBPK_275) passage number R45/14 were used in the study. The strains were isolated from Nepalese patients with confirmed VL, and cryo-preserved at the Institute of Tropical Medicine, in Antwerp, Belgium. Promastigotes were maintained at 26 °C in M199 medium supplemented with 20% (v/v) heat- inactivated fetal calf serum.
Intra-macrophage L. donovani assay
384-well Assay plates (CellCarrier Ultra, PerkinElmer) were prepared by adding 250 nL of compound to each well with an Echo 555 (Labcyte). For potency determination, eleven-point, one in three dilution curves were generated with a top concentration of 50 μM. The assay was adapted from de Rycker et al.37 and Peña et al.18. THP-1 cells were grown in CELLMASTER roller bottles (Greiner cat. #680048) for 72 hrs. The cells were monitored using an optical microscope and counted using a CASY cell counter. Differentiation was carried out in 225 cm3 T-FLASK in the presence of 30 nM of phorbol 12-myristate 13-acetate (PMA) (Sigma- Aldrich). Following incubation for 24 h at 37 °C, 5% CO2, cell differentiation was visually confirmed using an optical microscope. Cells were washed twice using cell culture media. Cells were infected using day-7 promastigotes of LdBPK_282 or LdBPK_275 at a multiplicity of infection (MOI) of 30 in the T-FLASK containing differentiated THP-1 cells. Each T- FLASK was incubated overnight and the remaining parasites were removed by washing three times with sterile DPBS. The infected cells were harvested by treatment with 0.05% (w/v) trypsin plus 0.48 mM EDTA for 5 mins and an aliquot was fixed and counted in a CASY cell counter. A cell preparation with a final concentration of 1.6*105 cells/mL was prepared in assay media consisting of RPMI (InvitrogenTM), supplemented with 2% heat-inactivated horse serum (HS)17 (Gibco) and 25 mM sodium bicarbonate (InvitrogenTM) containing 30 nM of PMA. Infected cells were plated onto assay plates containing the compounds (3000 cells/well, 50 μL) using a Multidrop Combi dispenser and incubated for 96 hrs at 37 °C. Plates were then fixed and stained by the addition of 50 μl of a solution containing 8% formaldehyde and 4 μM Draq5 DNA dye (BioStatus, UK) per well. The complete methodology is summarized in Fig. 1.
Image and data analysis
Images were taken with a HCS system (Opera QEHS, PerkinElmer) with a 40x objective, five fields per well, for a final number of 300 THP-1 cells per well. Automated image analysis was performed with an image analysis algorithm developed on Acapella high-content imaging and analysis software (PerkinElmer). The THP-1 cell count (MAC) and the average number of amastigotes per macrophage (AM/MAC) were calculated for each well, using the building blocks included in the analysis program. Briefly, using Draq5 signal, the host nuclei and cytoplasm were detected. Inside the cytoplasm spots were selected and filtered using morphology and texture properties identifying the amastigotes. Dose response curves were created and the pIC50 (−log IC50 – in molar units) was calculated. Data were normalized to percent of biological response by using positive (i.e. highest response achieved by non infected cells, RCtrl2) or negative (i.e. lowest response achieved in presence of DMSO, RCtrl1) controls by using equation (1):
where Rx is the assay response measured for the compound X. RCtrl1 and RCtrl2 are calculated as the average of replicates in the same microtiter plate where the compound X is tested. pIC50 values were obtained using the ActivityBase XE (IDBS, Guilford, Surrey, UK) nonlinear regression function in the full curve analysis bundle.
Minimum discriminatory difference (MDD) was calculated using equation (2) as follows:
where S is the pooled variance of the pIC50 determinations of the repeated compounds and N are the replication level of the assay.
Biosafety
Experimental procedures with L. donovani were carried out following standard operating procedures in compliance with biosafety level 3 (BSL3) regulations. THP-1 cells were treated according to GSK policies for the manipulation of human biological samples.
Data availability
All data generated or analysed during this study are included in this published article.
References
Alvar, J. et al. Leishmaniasis Worldwide and Global Estimates of Its Incidence. PLoS One 7, e35671 (2012).
Dhillon, G. P. S., Sharma, S. N. & Nair, B. Kala-azar elimination programme in India. J. Indian Med. Assoc. 106(664), 666–8 (2008).
Hefnawy, A., Berg, M., Dujardin, J.-C. & De Muylder, G. Exploiting Knowledge on Leishmania Drug Resistance to Support the Quest for New Drugs. Trends Parasitol. 33, 162–174 (2016).
Mittal, M. K. et al. Characterization of natural antimony resistance in Leishmania donovani isolates. Am. J. Trop. Med. Hyg. 76, 681–688 (2007).
Sundar, S., Jha, T. K., Thakur, C. P., Bhattacharya, S. K. & Rai, M. Oral miltefosine for the treatment of Indian visceral leishmaniasis. Trans. R. Soc. Trop. Med. Hyg. 100, S26–S33 (2006).
Rijal, S. et al. Increasing failure of miltefosine in the treatment of Kala-azar in Nepal and the potential role of parasite drug resistance, reinfection, or noncompliance. Clin. Infect. Dis. 56, 1530–8 (2013).
Srivastava, S. et al. Laboratory confirmed miltefosine resistant cases of visceral leishmaniasis from India. Parasit. Vectors 10, 49 (2017).
Meheus, F. et al. Cost-Effectiveness Analysis of Combination Therapies for Visceral Leishmaniasis in the Indian Subcontinent. PLoS Negl. Trop. Dis. 4, e818 (2010).
Singh, O. P., Singh, B., Chakravarty, J. & Sundar, S. Current challenges in treatment options for visceral leishmaniasis in India: a public health perspective. Infect. Dis. Poverty 5, 19 (2016).
García-Hernández, R., Manzano, J. I., Castanys, S. & Gamarro, F. Leishmania donovani Develops Resistance to Drug Combinations. PLoS Negl. Trop. Dis. https://doi.org/10.1371/journal.pntd.0001974 (2012).
Siqueira-Neto, J. L. et al. An image-based high-content screening assay for compounds targeting intracellular Leishmania donovani amastigotes in human macrophages. PLoS Negl. Trop. Dis. 6, e1671 (2012).
De Muylder, G. et al. A Screen against Leishmania Intracellular Amastigotes: Comparison to a Promastigote Screen and Identification of a Host Cell-Specific Hit. PLoS Negl. Trop. Dis. 5, e1253 (2011).
Freitas-Junior, L. H., Chatelain, E., Kim, H. A. & Siqueira-Neto, J. L. Visceral leishmaniasis treatment: What do we have, what do we need and how to deliver it? Int. J. Parasitol. Drugs Drug Resist. 2, 11–19 (2012).
da Luz, R. I., Vermeersch, M., Dujardin, J.-C., Cos, P. & Maes, L. In vitro sensitivity testing of Leishmania clinical field isolates: preconditioning of promastigotes enhances infectivity for macrophage host cells. Antimicrob. Agents Chemother. 53, 5197–203 (2009).
Siqueira-Neto, J. L. et al. Antileishmanial High-Throughput Drug Screening Reveals Drug Candidates with New Scaffolds. PLoS Negl. Trop. Dis. 4, e675 (2010).
Nühs, A. et al. Development and Validation of a Novel Leishmania donovani Screening Cascade for High-Throughput Screening Using a Novel Axenic Assay with High Predictivity of Leishmanicidal Intracellular Activity. PLoS Negl. Trop. Dis. 9, e0004094 (2015).
Tegazzini, D. et al. A Replicative In Vitro Assay for Drug Discovery against Leishmania donovani. Antimicrob. Agents Chemother. 60, 3524–32 (2016).
Peña, I. et al. New compound sets identified from high throughput phenotypic screening against three kinetoplastid parasites: an open resource. Sci. Rep. 5, 8771 (2015).
Goyard, S. et al. An in vitro system for developmental and genetic studies of Leishmania donovani phosphoglycans. Mol. Biochem. Parasitol. 130, 31–42 (2003).
Vermeersch, M. et al. In vitro susceptibilities of Leishmania donovani promastigote and amastigote stages to antileishmanial reference drugs: practical relevance of stage-specific differences. Antimicrob. Agents Chemother. 53, 3855–9 (2009).
Landqvist, C., Middleton, B. Jones, B. & O’Donnell, C. A novel approach by AstraZeneca to monitor primary DMPK assay performance & understand the inter and intra site assay variability. At http://www.ddw-online.com/drug-discovery/p218111-a-novel-approach-by-astrazeneca-to-monitor-primary-dmpk-assay-performance-&-understand-the-inter-and-intra-site-assay-variabilityfall-14.html (2014).
Heidelberg, E. Assay validation, performance and quality control Computational Aspects of High-Throughput Screening planning and analysis. At http://www.biomedbridges.eu/sites/biomedbridges.eu/files/training/9_-_david_murray_-_assay_validation.pdf (2013).
Tegazzini, D., Cantizani, J., Peña, I., Martín, J. & Coterón, J. M. Unravelling the rate of action of hits in the Leishmania donovani box using standard drugs amphotericin B and miltefosine. PLoS Negl. Trop. Dis. 11, e0005629 (2017).
Downing, T. et al. Genome-wide SNP and microsatellite variation illuminate population-level epidemiology in the Leishmania donovani species complex. Infect. Genet. Evol. 12, 149–59 (2012).
Musa, A. M. et al. Paromomycin for the treatment of visceral leishmaniasis in Sudan: a randomized, open-label, dose-finding study. PLoS Negl. Trop. Dis. 4, e855 (2010).
Mukhopadhyay, R. et al. Characterisation of antimony-resistant Leishmania donovani isolates: biochemical and biophysical studies and interaction with host cells. Int. J. Parasitol. 41, 1311–21 (2011).
Berg, M. et al. Metabolic adaptations of Leishmania donovani in relation to differentiation, drug resistance, and drug pressure. Mol. Microbiol. 90, 428–442 (2013).
Mukherjee, B. et al. Antimony-resistant but not antimony-sensitive Leishmania donovani up-regulates host IL-10 to overexpress multidrug-resistant protein 1. Proc. Natl. Acad. Sci. USA 110, E575–82 (2013).
Vanaerschot, M. et al. Linking In Vitro and In Vivo Survival of Clinical Leishmania donovani Strains. PLoS One 5, e12211 (2010).
Banjanac, M., Tatic, I., Ivezic, Z., Tomic, S. & Dumic, J. Pyrimido-Pyrimidines: A Novel Class of Dihydrofolate Reductase Inhibitors. Food Technol. Biotechnol. 47, 236–245 (2009).
Mjambili, F. et al. Synthesis and biological evaluation of 2-aminothiazole derivatives as antimycobacterial and antiplasmodial agents. Bioorg. Med. Chem. Lett. 24, 560–4 (2014).
Wyllie, S., Patterson, S. & Fairlamb, A. H. Assessing the Essentiality of Leishmania donovani Nitroreductase and Its Role in Nitro Drug Activation. Antimicrob. Agents Chemother. 57, 901–906 (2013).
Synthesis of 2-[3,5-substituted pyrazol-1-yl]-4,6-trisubstituted triazine derivatives as antimalarial agents. Bioorg. Med. Chem. Lett. 15, 4957–4960 (2005).
Boelaert, M. et al. Diagnostic tests for kala-azar: a multi-centre study of the freeze-dried DAT, rK39 strip test and KAtex in East Africa and the Indian subcontinent. Trans. R. Soc. Trop. Med. Hyg. 102, 32–40 (2008).
Bezuneh, A. et al. Comparison of point-of-care tests for the rapid diagnosis of visceral leishmaniasis in East African patients. Am. J. Trop. Med. Hyg. 91, 1109–15 (2014).
Bhattacharyya, T., Boelaert, M. & Miles, M. A. Comparison of Visceral Leishmaniasis Diagnostic Antigens in African and Asian Leishmania donovani Reveals Extensive Diversity and Region-specific Polymorphisms. PLoS Negl. Trop. Dis. 7, e2057 (2013).
De Rycker, M. et al. Comparison of a high-throughput high-content intracellular Leishmania donovani assay with an axenic amastigote assay. Antimicrob. Agents Chemother. 57, 2913–22 (2013).
Acknowledgements
This project has received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Sklodowska-Curie grant agreement N° 642609 and the Flemish Fund for Scientific Research (12Q8115N).
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: J.C.D., G.D.M., J.M. Performed the experiments: A.H., J.C., P.M. Analyzed the data: A.H., J.C., I.P., P.M. Contributed reagents or material: S.R. Wrote the paper and contributed to critical reading: A.H., J.C., P.M., J.C.D., S.R., G.D.M., J.M.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hefnawy, A., Cantizani, J., Peña, I. et al. Importance of secondary screening with clinical isolates for anti-leishmania drug discovery. Sci Rep 8, 11765 (2018). https://doi.org/10.1038/s41598-018-30040-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-30040-5
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.