Abstract
Despite a long-standing assertion that mammalian testes operate near hypoxia and increased testicular temperature causes frank hypoxia, we have preliminary evidence that changes are due to hyperthermia per se. The objective was to determine how variations in inspired oxygen concentration affected testicular blood flow, oxygen delivery and extraction, testicular temperature and lactate production. Eight rams were maintained under general anesthesia, with successive decreases in oxygen concentration in inspired air (100, 21 and 13%, respectively). As oxygen concentration decreased from 100 to 13%, there were increases in testicular blood flow (9.6 ± 1.7 vs 12.9 ± 1.9 ml/min/100 g of testis, P < 0.05; mean ± SEM) and conductance (normalized flow; 0.46 ± 0.07 to 1.28 ± 0.19 ml/min/mm Hg/100 g testis (P < 0.05). Increased testicular blood flow maintained oxygen delivery and increased testicular temperature by ~1 °C; this increase was correlated to increased testicular blood flow (r = 0.35, P < 0.0001). Furthermore, oxygen utilization increased concomitantly and there were no significant differences among oxygen concentrations in blood pH, HCO3− or base excess, and no effects of venous-arterial differences in lactate production. In conclusion, under acute hypoxic conditions, testes maintained oxygen delivery and uptake by increasing blood flow and oxygen extraction, with no evidence of anaerobic metabolism. However, additional studies are needed to determine longer-term responses and potential evidence of anaerobic metabolism at the molecular level.
Similar content being viewed by others
Introduction
Maintenance of testicular temperature 3–4 °C lower than the body core temperature is essential for production of morphologically normal and motile sperm in most mammals1,2,3. There is a long-standing paradigm that the testicular microenvironment functions on the brink of hypoxia4 and that with increasing testicular temperature, there is increased testicular metabolism and increased oxygen demands, but no change in testicular blood flow. Thus, decreases in percentage of morphologically normal and motile sperm that follow testicular hyperthermia are usually attributed to secondary effects of hypoxia and not directly to hyperthermia5,6.
With ischemic conditions due to compromised blood flow caused by obstruction of testicular vessels (e.g., varicocele and testicular torsion) or hypobaric hypoxia (e.g., reduced oxygen pressure at high altitudes), spermatogenesis and fertility were impaired, similar to changes after testicular warming7,8,9,10. Notwithstanding, these observations were not clear evidence that the pathogenesis of increased testicular temperature was due to hypoxia.
Markers of hypoxia have been detected after exposure to hyperthermia6,11, supporting the assertion that effects of testicular hyperthermia are due to hypoxia. However, in those studies, neither testicular blood flow nor oxygen delivery/utilization were measured. Although hyperemia was reported when testes not covered by the scrotum were exposed to increased temperatures12, this was not regarded as sufficient evidence to challenge the classical view that hypoxia mediates damage caused by testicular hyperthermia. In a previous preliminary study13, conscious rams breathed inspired air containing 85, 21 or 14% oxygen for 30 h. Half of the rams had an insulated scrotum (a well-established model to increase testicular temperature); in those rams, percentages of morphologically normal sperm and motile sperm were significantly decreased from ~2 to 5 wk after exposure. Furthermore, in that study, hyperoxia did not mitigate effects of scrotal insulation, nor did hypoxia cause subsequent decreases in morphologically normal or motile sperm. Based on that preliminary study, we inferred that hyperthermia per se, and not hypoxia, was the underlying cause of reductions in morphologically normal and motile sperm following testicular hyperthermia. However, neither testicular blood flow nor oxygen delivery were measured. Therefore, objectives of the current study were to determine how variations in oxygen concentrations in inspired air affected testicular blood flow, oxygen delivery and extraction, lactate production and testicular temperature.
Results
As oxygen content in inspired air decreased, there were significant increases in testicular blood flow (Fig. 1a) and conductance (Fig. 1b), accompanied by concurrent increases in intra-testicular temperature (Fig. 1c), although body temperature remained constant. Furthermore, testicular blood flow and intra-testicular temperature were correlated (r = 0.35, P < 0.0001; Fig. 1d).
(a) Testicular blood flow and (b) testicular conductance (mean ± SEM) in eight rams exposed to three concentrations of oxygen in inspired air. (c) Testicular and body temperatures over time (mean ± SEM). (d) Correlation between testicular temperature and testicular blood flow (r = 0.35, P < 0.0001). One-way analysis of variance for repeated measures, followed by a Dunnet’s t test, was used to compare, among groups, data recorded at 30 min. Pearson’s correlation analyses were used to determine linear correlations. *P ≤ 0.05; **P ≤ 0.01.
Testicular oxygen delivery was maintained throughout the entire experiment and not affected by reductions in oxygen concentration in inspired air (Fig. 2a). Furthermore, as oxygen concentrations decreased, there were increases in testicular metabolic rate (Fig. 2b) and oxygen extraction (Fig. 2c).
(a) Testicular oxygen delivery, (b) testicular metabolic rate and (c) testicular oxygen extraction (mean ± SEM) in eight rams exposed to three concentrations of oxygen in inspired air. One-way analysis of variance for repeated measures, followed by a Dunnet’s t test, was used to compare, among groups, data recorded at 30 min. *P ≤ 0.05; **P ≤ 0.01.
Consistent with our experimental design, there were large and significant differences among groups for testicular arterial and venous oxygen content (Fig. 3a) and arterial and venous PO2 (Fig. 3b). However, there were no significant differences among groups for PCO2 in either the testicular artery or vein.
Testicular arterial, venous, and A-V difference in (a) venous blood oxygen content, (b) PO2; and (c) lactate concentrations and net production (mean ± SEM) in eight rams exposed to three concentrations of oxygen in inspired air. One-way analysis of variance for repeated measures, followed by a Dunnet’s t test, was used to compare, among the three groups, data recorded at 30 min. *P ≤ 0.05; **P ≤ 0.01; ***P ≤ 0.001; ****P ≤ 0.0001.
Lactate concentrations in the testicular artery and the testicular vein were higher (P < 0.05) at 13% oxygen versus at 21 or 100%, but there was no significant difference among groups for venous-arterial differences in lactate concentrations (Fig. 3c). Furthermore, there were no significant differences among groups for arterial or venous pH, HCO3− or base excess, and no significant venous-arterial differences for pH, HCO3− or base excess.
Discussion
Although regulation of blood flow in response to varying oxygen concentrations in inspired air has been extensively studied in several organs3,14,15,16,17, this was apparently the first study to characterize effects of varying inspired-air oxygen concentrations on testicular blood flow, oxygen delivery, oxygen uptake, and temperature in rams. In this study, as oxygen concentrations in inspired air decreased from 100 to 13%, blood flow increased concurrently and sustained oxygen delivery to the testis. This increased blood flow increased testicular temperature by ~1 °C and concomitantly increased metabolism and oxygen utilization. There was a small (albeit significant) increase in venous lactate concentrations, but no significant increase in the venous-arterial difference. Therefore, under the acute conditions of this study, we concluded that there were no indications of a shift to anaerobic metabolism over a broad range of inspired-air oxygen concentrations.
In the present study, hypoxia (i.e., 13% oxygen) significantly increased the supply of blood to the testes, either measured as blood flow or as conductance (flow normalized by arterial pressure). Although testicular hypoxia is considered to cause male infertility18,19,20, repeated complete interruptions of blood flow to the testes (occlusion of testicular artery for 1-h intervals) did not cause long-term impairment of sperm production in rams21. Regardless, chronic exposure to severe intermittent hypoxia in male rats (5% oxygen in inspired air) reduced sperm motility and fertility22. Perhaps the degree and duration of testicular hypoxia affects the ability to compensate.
Testicular blood flow and testicular temperature were significantly correlated (r = 0.35) in the current study, similar to bulls23. Clearly, hypoxia-induced increases in blood flow increased testicular temperature and metabolism. Furthermore, rectal temperature remained constant, suggesting that increased blood flow to the testis was not a systemic response, consistent with a previous report23,24. Acute or chronic hypoxia decreased oxygen content in rat muscle, although blood flow was not altered25. In the human brain, hypoxia (14% for 18 min) increased oxygen metabolic rate and blood flow (compared to 21% oxygen26, consistent with the present study. In some organs, a reduced oxygen supply increased blood flow27,28 due to release of vasodilators (decreased oxygen impairs re-phosphorylation of adenosine diphosphate (ADP), which is subsequently degraded to adenosine, a compound that causes vasodilation15.
Another consequence of induced hypoxia was increased oxygen extraction from arterial blood, from ~40% at 21% oxygen to ~60% at 13% oxygen (P < 0.01), thereby reducing oxygen content and PO2 in the testicular vein, although PCO2 remained unchanged. Observed effects were similar to those reported by Pittman15 and Hoffman29, indicating that under hypoxic conditions, the first physiological reflex was to open capillaries to increase available area for oxygen exchange, accounting for the observed increase in oxygen extraction. Interestingly, prolonged exposure to reduced oxygen concentrations (e.g., at high altitudes) may result in adaptation with no increase in extraction after long-term exposure, suggesting a more important role for increased extraction under acute exposures30.
Both hyperoxia and hypoxia can cause oxidative damage and lipid peroxidation11. Chronic exposure to hyperoxia reduced PO2, pH and increased PCO2 in old versus young rats, indicating that age affects tolerance to this condition31,32. Furthermore, hyperoxia increased the activity of radical oxygen species and may impair diaphragm contractility, potentially affecting body oxygenation20. Exposure to ~100% oxygen in inspired air decreased blood flow to the rat brain26,33, reduced (~8–30%) cardiac blood flow in humans34, and caused a 7% reduction in renal blood flow35, all of which were consistent with our finding that testicular blood flow was lowest at 100% oxygen.
Lactate is a well-defined marker of hypoxia36,37,38. In bulls, lactate concentrations in the rete testis were similar to those in the blood39, although for humans they can be slightly higher38. Lactate is produced in testes as a product of glucose metabolism by Sertoli cells40,41,42; increased concentrations were reported in pathological conditions in rats, including cryptorchidism43 and hypoxia44. Furthermore, a severe reduction in lactate was also associated with infertility45. In the present study, lactate concentrations in the testicular vein were increased (P < 0.05) when rams were exposed to 13% oxygen. However, venous-arterial differences were not significant among groups, nor were there significant venous-arterial differences in pH, HCO3− or base excess. Therefore, there was no evidence of reduced oxygen concentrations in inspired air causing anaerobic metabolism.
In the present study, only blood samples were collected and analyzed. Although retrieval of testicular biopsies was considered, it was expected that this would cause hemorrhage and inflammation that could invalidate the study. Furthermore, we did not sample tissues to detect angiogenesis, as these changes were not detected at 1 d after the onset of hypoxia in mice46, although they were detected at 5 d after the onset of hypoxia in rats47.
There are alternative approaches to detect a change from aerobic to anaerobic metabolism. Important examples are genes that contain the Hypoxia-Response Element (HRE) in their promoter region; hypoxia is associated with increased gene expression of those specific genes, including Hypoxia Induced Factor (HIF) I and II48,49. Furthermore, identification of thiobarbituric acid reactive substances (TBARS) and Reactive Species of oxygen (ROS) are important markers of tissue hypoxia and oxidative damage in the testes50,51. Unfortunately, in the present work, due to the experimental design and the potential for damage, testicular biopsies were not collected. Therefore, in future studies, recovery of testicular tissue and assessment of cellular and molecular evidence of tissue hypoxia should be done. In addition, more prolonged exposure to hypoxia in rams to determine long-term effects on testicular tissue, sperm and blood testosterone concentrations, are indicated.
Our experiment was designed to minimize the impact of anesthesia. Each ram was initially subjected to 100% oxygen, followed by two successive reductions in oxygen content in inspired air; therefore, each ram served as its own control. In addition, anesthetic depth was maintained at as constant a plane as possible throughout the experiment. Furthermore, adult animals were used, since the testicular vascular cone (TVC) undergoes development until puberty52,53 and is fundamental for thermoregulatory capabilities of the testes3. To our knowledge, there are no studies in pre-pubertal animals regarding testicular blood flow response to heat stress.
In conclusion, under acute hypoxic conditions (13% oxygen in inspired air), the testis maintained oxygen delivery and uptake by increasing blood flow and oxygen extraction, with no indications of a shift to anaerobic metabolism. Similarly, in our previous study in conscious rams, exposure of control rams (no scrotal insulation) to 85, 21 and 14% oxygen for 30 h had no significant effect on semen quality13. Thus, we concluded that the testis compensated for decreased oxygen concentrations in inspired air, although this needs additional confirmation.
Materials and Methods
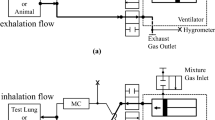
Eight crossbred rams (12–15 mo, 40–56 kg) were used. Rams were pre-medicated with 8 μg/kg dexmedetomidine (Dexdomitor (0.5 mg/ml, Zoetis, Parsippany-Troy Hills, NJ, USA) and 2 mg/kg of alfaloxone (Alfaxan 10 mg/ml, Jurox Pty Ltd, Rutherford, NSW Australia) administered IM. After approximately 15 min, anesthesia was induced with 2 mg/kg of alfaloxone administered IV. Thereafter, rams were intubated, anesthesia was maintained by inhalation of isoflurane (1.0–2.0%; Fresenius Kabi Animal Health, Richmond Hill, ON, Canada) and a constant volume ventilator (Harvard Apparatus – 12 breaths/min – 10 ml/kg stroke volume) was used throughout the study. To reduce the depth of anesthesia needed, epidural analgesia (0.07 mg/kg of xylazine (Rompun, 20 mg/kg, Bayer, Mississauga, ON, Canada) in ~4 mL of saline) and local anesthetic blocks (bupivacaine (Bupivacaine, 2.5 mg/ml, Hospira Inc., Lake Forest, IL, USA), ~2 ml/site SC) were performed at incision sites. All rams were maintained under general anesthesia throughout the procedure and euthanized (saturated potassium chloride given IV under deep anesthesia) at the end of the study. This study was reviewed and approved by the University of Calgary Health Sciences Animal Care Committee (AC16-0010) and all methods were conducted in accordance with the guidelines.
Each ram was exposed to three oxygen concentrations (100, 21 and 13% sequentially) in inspired air, by combining oxygen and nitrogen. Following reductions in oxygen concentration, rams were allowed ~20 min to adapt, and thereafter exposure was maintained for another 45 min, with measurements recorded at 30 min (temperature measured at 0, 15, 30 and 45 min). Oxygen concentrations were determined with an oxygen analyzer (MySign®O, Wilmar, MV, Germany).
All invasive procedures were performed under anesthesia. Testicular temperatures were measured by inserting a needle thermocouple (20-gauge × 2.5 cm23), through the scrotal skin (anterior aspect of testis) and into the testis. This thermocouple was inserted at the beginning of the intervention and remained in situ throughout the study. Standard ECG leads were attached (for cardiac monitoring). The right carotid artery was isolated and a 14-gauge polyvinyl catheter was placed for monitoring arterial pressure and determining arterial blood gases. The right jugular was isolated for intravenous administration of saline (5 ml/kg/h) and drug administration. An incision (~12 cm) was made between the right external inguinal ring and attachment of the scrotum to the body wall. The spermatic cord was identified and the testicular artery and vein isolated. A 20-gauge catheter was inserted in the left testicular vein (distal to the testis) for blood gas and lactate measurement. Blood samples were collected from the carotid artery and testicular vein to measure blood gases and lactate (Nova Biomedical, Stat Profile® pHOx Ultra®, Waltham, MA, USA). An ultrasonic flow probe (2SB1551; Transonic® Flowprobe, Ithaca, NY, USA) was placed around testicular artery to measure blood flow. Measurements were performed and recorded and arterial and venous blood samples collected at 30 min after the start of the monitored interval. Blood flow was obtained with specific software (Sonometrics Corp. System, London, ON, Canada) and data were further converted using custom software (CV Works, AccuDAQ Inc, Calgary, AB, Canada). Testicular perfusion and oxygenation were calculated as described (Table 1). In addition, for testicular vasculature, arterial-venous differences were calculated for oxygen content, PO2, PCO2, pH, HCO3− or base excess and venous-arterial differences were calculated for lactate.
One-way analysis of variance for repeated measures, followed by a Dunnet’s t-test, was used to compare, among the three groups, data recorded at 30 min. Pearson’s correlation analysis was used to determine linear correlations. All statistical analyses were performed with GraphPad Prism Version 6.0 (GraphPad Software Inc, La Jolla, CA, USA) and P < 0.05 was considered significant.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Freeman, S. The evolution of the scrotum: A new hypothesis. J. Theor. Biol. 145, 429–445 (1990).
Kastelic, J. P., Coulter, G. H. & Cook, R. B. Scrotal surface, subcutaneous, intratesticular, and intraepididymal temperatures in bulls. Theriogenology. 44, 147–152 (1995).
Kastelic, J. P., Rizzoto, G. & Thundathil, J. Review: Testicular vascular cone development and its association with scrotal thermoregulation, semen quality and sperm production in bulls. Animal 12, 133–141 (2018).
Bergh, A., Collin, O. & Lissbrant, E. Effects of acute graded reductions in testicular blood flow on testicular morphology in the adult rat. Biol. Reprod. 64, 13–20 (2001).
Hamilton, T. R. et al. Evaluation of lasting effects of heat stress on sperm profile and oxidative status of ram semen and epididymal sperm. Oxid. Med. Cell Longev. 2016, 1687657, https://doi.org/10.1155/2016/1687657 (2016).
Paul, C., Teng, S. & Saunders, P. T. K. A single, mild, transient scrotal heat stress causes hypoxia and oxidative stress in mouse testes, which induces germ cell death. Biol. Reprod. 80, 913–919 (2009).
Ates, U. et al. The effects of local and systemic growth hormone treatment on germ cell population and fertility in an experimental unilateral testicular torsion and orchiectomy model. J. Urol. 194, 1816–1822 (2015).
Damsgaard, J. et al. Varicocele is associated with impaired semen quality and reproductive hormone levels: a study of 7035 healthy young men from six European Countries. Eur. Urol. 70, 1019–1029 (2016).
Reyes, J. G. et al. The hypoxic testicle: physiology and pathophysiology. Oxid. Med. Cell. Longev. 2012, 929285, https://doi.org/10.1155/2012/929285 (2012).
Verratti, V. et al. Evidence that chronic hypoxia causes reversible impairment on male fertility. Asian. J. Androl. 10, 602–606 (2008).
Verratti, V. et al. Pampiniform plexus and oxidative stress during chronic hypoxia and hyperoxia. Int. J. Immunopathol. Pharmacol. 21, 353–357 (2008).
Mieusset, R., Sowerbutts, S. F., Zupp, J. L. & Setchell, B. P. Increased flow of testicular blood plasma during local heating of the testes of rams. J. Reprod. Fertil. 94, 345–352 (1992).
Kastelic, J. P., Wilde, R. E., Rizzoto, G. & Thundathil, J. C. Hyperthermia and not hypoxia may reduce sperm motility and morphology following testicular hyperthermia. Vet. Med. (Praha). 62(8), 437–442 (2017).
Hoiland, R. L., Bain, A. R., Rieger, M. G., Bailey, D. M. & Ainslie, P. N. Hypoxemia, oxygen content, and the regulation of cerebral blood flow. Am. J. Physiol. Regul. Integr. Comp. Physiol. 310, 398–413 (2016).
Pittman, R. N. The circulatory System and Oxygen Transport. In Regulation of Tissue Oxygenation (eds Grangers, D. N. & Granger, J. Williston) (Morgan & Claypool Life Sciences, 2011).
Segal, S. S. & Kurjiaka, D. T. Coordination of blood flow control in the resistance vasculature of skeletal muscle. Med. Sci. Sports. Exerc. 27, 1158–1164 (1995).
Steinback, C. D. & Poulin, M. J. Influence of hypoxia on cerebral blood flow regulation in humans. Adv. Exp. Med. Biol. 903, 131–144 (2016).
Gat, Y. et al. Azoospermia and Sertoli-cell-only syndrome: hypoxia in the sperm production site due to impairment in venous drainage of male reproductive system. Andrologia. 42, 314–321 (2010).
Okumura, A., Fuse, H., Kawauchi, Y., Mizuno, I. & Akashi, T. Changes in male reproductive function after high altitude mountaineering. High. Alt. Med. Biol. 4, 349–353 (2003).
Wang, X. et al. Hypoxia reduces testosterone synthesis in mouse Leydig cells by inhibiting NRF1-activated StAR expression. Oncotarget. 8, 16401–16413 (2017).
Van Vliet, J. et al. Reversible harmless interruption of testicular blood supply in the ram. J. Androl. 8, 108–115 (1987).
Torres, M. et al. Male fertility is reduced by chronic intermittent hypoxia mimicking sleep apnea in mice. Sleep. 37, 1757–1765 (2014).
Barros-Adwell, C. M. Q. et al. Arterial blood flow is the main source of testicular heat in bulls and higher ambient temperatures significantly increase testicular blood flow. Theriogenology 116, 12–16 (2018).
Maloney, S. K. & Mitchell, D. Regulation of ram scrotal temperature during heat exposure, cold exposure, fever and exercise. J. Physiol. 496, 421–430 (1996).
Marshall, J. M. & Davies, W. R. The effects of acute and chronic systemic hypoxia on muscle oxygen supply and oxygen consumption in the rat. Exp. Physiol. 84, 57–68 (1999).
Xu, F., Liu, P., Pascual, J. M., Xiao, G. & Lu, H. Effect of hypoxia and hyperoxia on cerebral blood flow, blood oxygenation, and oxidative metabolism. J. Cereb. Blood Flow Metab. 32, 1909–1918 (2012).
Kuwahira, I., Heisler, N., Piiper, J. & Gonzalez, N. C. Effect of chronic hypoxia on hemodynamics, organ blood flow and O2 supply in rats. Respir. Physiol. Neurobiol. 92, 227–238 (1993).
Zerbini, L. et al. Effect of acute hypoxia on muscle blood flow, VO(2)p, and HHb kinetics during leg extension exercise in older men. Eur. J. Appl. Physiol. 113, 1685–1694 (2013).
Hoffman, J. I. E. Regulation of myocardial blood flow and oxygen delivery during hypoxia. In Hypoxia, Metabolic Acidosis, and the Circulation, (ed. Arieff, A. I.) (Springer-Verlag New York, 1992).
Martin, D. S. et al. Systemic oxygen extraction during exercise at high altitude. Br. J. Anaesth. 114, 677–682 (2015).
Andrade, P. V. et al. Influence of hyperoxia and mechanical ventilation in lung inflammation and diaphragm function in aged versus adult rats. Inflammation. 37, 486–494 (2014).
Aljerian, K. & Haffor, A. S. Effects of hyperoxia exposure on free radicals accumulation in relation to ultrastructural pathological changes of diaphragm. J. Clin. Exp. Pathol. 5(5), 247–254 (2015).
Watson, N. A., Beards, S. C., Altaf, N., Kassner, A. & Jackson, A. The effect of hyperoxia on cerebral blood flow: a study in healthy volunteers using magnetic resonance phase-contrast angiography. Eur. J. Anaesth. 17, 152–159 (2000).
Farquhar, H. et al. Systematic review of studies of the effect of hyperoxia on coronary blood flow. Am. Heart J. 158, 371–377 (2009).
Jain, K. K. P. physiological and biochemical aspects of hyperbaric oxygenation. In Textbook of Hyperbaric Medicine (ed. Jain, K. K.) (Springer Nature, 2017).
Adeva-Andany, M. et al. Comprehensive review on lactate metabolism in human health. Mitochondrion 17, 76–100 (2014).
Chang, A. J., Ortega, F. E., Riegler, J., Madison, D. V. & Krasnow, M. A. Oxygen regulation of breathing through an olfactory receptor activated by lactate. Nature. 527, 240–244 (2015).
Lee, D. C. et al. A lactate-induced response to hypoxia. Cell. 161, 595–609 (2015).
Voglmayr, J. K., Larsen, L. H. & White, I. G. Metabolism of spermatozoa and composition of fluid collected from the rete testis of living bulls. J. Reprod. Fertil. 21, 449–460 (1970).
Bodansky, O. Neoplasms of the testis. In Biochemistry of Human Cancer (ed. Bodansky, O.). (Academic Press, 1975).
Erkkila, K., Aito, H., Aalto, K., Pentikainen, V. & Dunkel, L. Lactate inhibits germ cell apoptosis in the human testis. Mol. Hum. Reprod. 8, 109–117 (2002).
Regueira, M. et al. Novel molecular mechanisms involved in hormonal regulation of lactate production in Sertoli cells. Reproduction (Cambridge, England). 150, 311–321 (2015).
Harkonen, M. & Kormano, M. Energy metabolism of the normal and cryptorchid rat testis. J. Reprod. Fertil. 25, 29–39 (1971).
Shevantaeva, O. N. & Kosyuga, Y. I. Effect of acute hypobaric hypoxia on spermatogenesis and lactate concentration in testicular tissue of male albino rats. Bull. Exp. Biol. Med. 141, 20–22 (2006).
Alves, M. G. et al. Testicular lactate content is compromised in men with Klinefelter Syndrome. Mol. Reprod. Dev. 83, 208–216 (2016).
Madrid, E. et al. Effect of normobaric hypoxia on the testis in a murine model. Andrologia 45, 332–338 (2013).
Farías, J. G., Bustos-Obregón, E. & Reyes, J. G. Increase in testicular temperature and vascularization induced by hypobaric hypoxia in rats. J. Androl. 26, 693–697 (2005).
Loboda, A., Jozkowicz, A. & Dulak, J. HIF-1 and HIF-2 transcription factors–similar but not identical. Molecules and Cells 29, 435–442 (2010).
Lin, C. A. & Tsai, S. J. Hypoxia may play a role in steroidogenesis in the testes of infertile men. Biology of Reproduction 83, 523–523 (2010).
Cvetkovic, T. et al. Oxidant and antioxidant status in experimental. International Journal of Fertility & Sterility 9, 121–128 (2015).
Zepeda, A. et al. Blueberry extracts protect testis from hypobaric hypoxia induced oxidative stress in rats. Oxidative Medicine and Cellular Longevity 2012, https://doi.org/10.1155/2012/975870 (2012).
Cook, R. B., Coulter, G. H. & Kastelic, J. P. The testicular vascular cone, scrotal thermoregulation, and their relationship to sperm production and seminal quality in beef bulls. Theriogenology 41, 653–671 (2004).
Brito, L. F., Barth, A. D., Wilde, R. E. & Kastelic, J. P. Testicular vascular cone development and its association with scrotal temperature, semen quality, and sperm production in beef bulls. Anim. Reprod. Sci. 134, 135–140 (2012).
Caulkett, N. A., Duke, T. & Cribb, P. H. Cardiopulmonary effects of metomidine: ketamine in domestic sheep (Ovis ovis) maintained in sternal recumbency. J. Zoo Wildl. Med. 27(2), 217–226 (1996).
Semeniuk, L. M., Belenkie, I. & Tyberg, J. V. Acute effects of toborinone on vascular capacitance and conductance in experimental heart failure. Circulation. 59, 58–63 (1998).
Acknowledgements
We appreciate the efforts of the animal care staff for maintaining and transporting the rams.
Author information
Authors and Affiliations
Contributions
G.R. was involved in all aspects, from developing the experimental design to writing the manuscript. C.H. provided technical support during data collection. J.V.T., N.A.C., J.C.T. and J.P.K. provided technical support throughout the study, from experimental design to anesthetic protocols and data collection. All authors were involved in writing and preparation of figures. Furthermore, the final version was reviewed by all authors.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rizzoto, G., Hall, C., Tyberg, J.V. et al. Increased testicular blood flow maintains oxygen delivery and avoids testicular hypoxia in response to reduced oxygen content in inspired air. Sci Rep 8, 10905 (2018). https://doi.org/10.1038/s41598-018-29248-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-29248-2
This article is cited by
-
Association between body condition score, testicular haemodynamics and echogenicity, nitric oxide levels, and total antioxidant capacity in rams
Irish Veterinary Journal (2023)
-
Exogenous gonadotropin-releasing hormone counteracts the adverse effect of scrotal insulation on testicular functions in bucks
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.