Abstract
Using a well-designed longitudinal cohort, we aimed to identify cytokines that were protective against malaria and to explore how they were influenced by genetic and immunological factors. 349 Mozambican pregnant women and their newborn babies were recruited and followed up for malaria outcomes until 24 months of age. Six Th1 cytokines in cord blood were screened for correlation with malaria incidence, of which IL-12 was selected for further analyses. We genotyped IL-12 polymorphisms in children/mothers and evaluated the genotype-phenotype associations and genetic effects on IL-12 levels. Maternal IL-12 concentrations were also investigated in relation to Plasmodium infections and cord blood IL-12 levels. Our data showed that high background IL-12 levels were prospectively associated with a low incidence of clinical malaria, while IL-12 production after parasite stimulation had the opposite effect on malaria incidence. IL-12 genotypes (IL-12b rs2288831/rs17860508) and the haplotype CGTTAGAG distribution were related to malaria susceptibility and background IL-12 levels. Maternal genotypes also exhibited an evident impact on host genotype-phenotype associations. Finally, a positive correlation in background IL-12 levels between maternal and cord blood was identified. Thus, cord blood background IL-12 concentrations are important for protecting children from clinical malaria, likely mediated by both genotypes (children&mothers) and maternal immunity.
Similar content being viewed by others
Introduction
Childhood malaria remains one of the leading causes of morbidity and mortality with 500, 000 deaths annually. According to the WHO World Malaria Report 20171, more than 90% of malaria infections occurred in sub-Saharan Africa, of which 90% of deaths were attributable to Plasmodium falciparum. In malaria endemic regions, children under five years of age are highly susceptible to clinical malaria, while infants up to six months are relatively resistant, although the exact mechanism remains unclarified2. The host response to the parasite infection varies from asymptomatic carriage to the classic symptoms of clinical episode (e.g. fever, chills, sweating, headache and muscle aches), or to even severe life-threatening complications such as severe anaemia, respiratory distress, hyperparasitemia and cerebral malaria.
The basic immunity features of Plasmodium infections are pro-inflammatory responses in the early stage followed by anti-inflammatory responses during disease progression3,4. Pro-inflammatory Th1-type cytokines (IL-1, IL-6, IL-12, IFN-γ and TNF) are thought to be critical for controlling the erythrocytic and hepatic stages of Plasmodium infection, but the excessive production of these cytokines might also predispose to severe pathology3,4,5. Anti-inflammatory Th2-type and modulatory cytokines (IL-10 and TGF-β) downregulate the Th1-type cytokine response, thereby preventing subjects from severe forms of malaria3,4,6. Numerous immuno-epidemiological studies conducted in malaria endemic areas have illustrated the complex and paradoxical relationships between inflammatory cytokines and clinical presentations of P. falciparum infection7,8,9,10,11,12,13. For example, an elevated expression of IL-1, IL-6, IL-12, IFN-γ and TNF was found in severe malaria and in hyperparasitemia, a primary clinical feature of severe disease7,8,9,10. On the other hand, other studies showed that reduced IL-12 and IFN-γ levels were associated with an increased risk of severe malarial anaemia in children11,12, while lower levels of IL-6 were correlated with hyperparasitemia9.
Due to dynamic changes of cytokine profiles during physiopathological processes, most of the published studies using cross-sectional designs are not convincing to infer causal relationships of cytokine responses with disease phenotypes. A longitudinal birth cohort of infants is therefore important for understanding naturally acquired immunity to malaria and the associated genetic regulatory mechanisms14,15,16.
We hypothesised that Th1 cytokines at birth are important for determining the susceptibility of young children to clinical malaria. Using our well-defined prospective cohort14,15,16, we preliminarily screened six candidate Th1 cytokines (IL-1, IL-6, IL-12, IFN-γ, TNF and TNF-β), and identified IL-12 as a promising molecule for malaria protection. IL-12 is a heterodimeric p70 protein composed of p35 and p40 subunits encoded by IL-12a and IL-12b genes respectively. We further hypothesised that IL-12 polymorphisms are associated with the disease protection during early life, through governing the functional expression of IL-12. Here we evaluated the associations of cord blood IL-12 concentrations, and IL-12 genotypes/haplotypes with malaria outcome. Maternal effects on childhood malaria have been reported17,18, thus we also explored the significance of maternal regulation of cord blood IL-12 expression in modifying the disease susceptibility in the infant.
Results
Clinical and parasitological characteristics
General information on the children and their mothers included in this study is described in our previous publications14,15,16. Approximately 20% of the children were not successfully followed up or subjected to laboratory tests due to a variety of reasons such as parental withdrawal and insufficient blood collection. During the two-year follow-up, 108 children (108/326, 33.1%) had one or more malaria episodes. Twenty-three children (23/284, 8.1%) were diagnosed with anaemia at the endpoint of follow-up. Concurrently, 32 (32/284, 11.3%) and 101(101/256, 39.5%) children were identified as P. falciparum positive for parasitemia by microscopic method and qPCR assay, respectively. In terms of pregnancy infection, we found 27 (27/349, 7.7%) mothers presented with maternal parasitemia and 60 (60/277, 21.7%) mothers with placental infection, determined by microscopy and histology, respectively. Additionally 25 (25/254, 7.2%) newborns presented congenital infection, as detected by qPCR in filter papers, which was included as one of the confounding factors for adjustment in our analysis models.
Cord cytokine and malaria phenotypes
Using Poisson regression analysis and taking into account the effects of the confounding factors e.g. intervention, mother’s age, use of insecticide-treated mosquito nets (ITNs), use of indoor residual spraying (IRS) and congenital infection (parasites in cord), we investigated the association between the concentration of six Th1 cytokines secreted by cord blood cells in culture supernatants and the incidence of clinical malaria in the second year of life in young children (Table 1). We found that the background and stimulated/specific IL-12 levels had an opposite association with disease onset (Table 1). A high background IL-12 level in cord blood was prospectively associated with a low incidence of clinical malaria (p = 0.020) (Table 1). In contrast, a high IL-12 production or a high specific IL-12 response after P. falciparum antigen stimulation was significantly related to an increased risk of clinical malaria (p < 0.001) (Table 1). The stimulated form of IFN-γ also demonstrated a positive association with high morbidity of childhood malaria (p = 0.010) (Table 1).
Further, we tested the association of cord cytokine levels with other malaria related phenotypes including parasitemia and anaemia. The specific IL-12 response was marginally higher in 2 year old children who had microscopically confirmed parasitemia (p = 0.054), relative to those without parasitemia (Supplementary Figure 1a). After controlling the aforementioned confounders, the difference showed statistical significance (p = 0.044) (Supplementary Table 1). As for anaemia, the background IL-1 levels were significantly lower in children with anaemia (p = 0.024) (Supplementary Table 1), whereas such difference was not evident for IL-12 (Supplementary Figure 1b). Using the Pearson correlation analysis, we found that the Plasmodium-specific IL-12 response was positively associated with blood P. falciparum copy number (r = 0.150, p = 0.036, n = 196) quantified by qPCR assay in filter paper samples. The specific IL-12 response was not correlated with plasma haemoglobin concentration. Moreover, a correlation between IL-1 levels and plasma haemoglobin concentration was not detected.
Apart from the associations outlined above, we did not observe any other significant differences (Supplementary Table 1). As IL-12 proved promising in preventing childhood malaria, our subsequent studies were focused on this cytokine, while the other cytokines were thereafter excluded from further analysis.
Genotypes and haplotypes with malaria phenotypes
The distributions of the genotypes in young children and their mothers are summarized in Supplementary Table 2. Significant departure from the HWE was observed for children’s IL-12b rs2288831 (p = 0.025) and mothers’ IL-12b rs2546890 (p = 0.010) in the distribution of genotypes in the overall population. However, when we tested in the respective control groups (children without congenital infection and mothers without maternal parasitemia), such deviation was not significant for any of the examined single nucleotide polymorphisms (SNPs) in both children and mothers (p > 0.05).
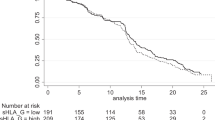
Out of the four IL-12 SNPs examined, the IL-12b rs2288831 and rs17860508 genotypes were found to be significantly associated with malaria incidence (p = 0.005 and p = 0.007 respectively) (Table 2). Children with allele C of IL-12b rs2288831 had a significantly lower incidence of malaria in the second year than those with allele T (CC vs CT, p = 0.003; CC vs TT, p = 0.001) (Fig. 1a). The GC allele of host IL-12b rs17860508 was associated with a high risk of clinical malaria occurrence compared to the TTAGAG allele (TTAGAG vs TTAGAG/GC, p = 0.004; TTAGAG vs GC, p = 0.002) (Fig. 1b). Similar effects were revealed for the maternal genotypes of IL-12b rs2288831 and rs17860508 and their association with clinical episodes of malaria (p < 0.001 and p = 0.005 respectively) (Table 2 and Fig. 1). Additionally a significant effect of the genotype distribution of maternal IL-12b rs2546890 on malaria incidence was identified (p = 0.008), with increasing risk from allele G to A (Table 2). After adjusting for the corresponding maternal SNPs, the effect of children’s IL-12b rs17860508 genotypes on malaria was decreased but remained significant (p = 0.023), while the significant effect of IL-12b rs2288831 disappeared (p = 0.929).
IL-12b Genotypes and Malaria Incidence: Incidence rate ratios were compared in host and maternal genotypes of IL-12b rs2288831 (a) and IL-12b rs17860508 (b). The homozygous genotypes CC and TTAGAG were used as reference allele for the two IL-12b polymorphisms respectively. Poisson regression analysis was used, controlling for intervention, mother’s age, parity, infant sex, use of insecticide-treated mosquito nets, use of indoor residual spraying, congenital infection. Values represent Mean (95% confidence interval).
A strong linkage was identified amongst IL-12b gene SNP rs2546890, rs2288831 and rs17860508 (Supplementary Figure 2), and the association of haplotypes with malaria episodes was subsequently investigated (Table 2). The host CGTTAGAG haplotype was significantly related to a decreased risk of malaria episodes during the first 2 years of life (High probability vs Low probability, p = 0.025; High probability vs Null, p = 0.013) (Fig. 2a), while newborns with a TGGC haplotype had an increased risk of malaria episodes (High probability vs Null, p = 0.006) (Fig. 2a). The haplotype TAGC did not alter the susceptibility to a clinical malaria episode.
Children IL-12b Haplotypes and Malaria Incidence/Cord Blood IL-12 Production: Incidence rate ratios were compared in children with different probabilities of carrying the haplotypes CGTTAGAG and TGGC using Poisson regression model, with high probability as reference haplotype (a). The cord blood background IL-12 levels were stratified by different probabilities of carrying host haplotypes CGTTAGAG and TGGC using linear regression model (b). All analyses are adjusted for the confounding factors. High: 100% probability; Low: 20–50% probability; Null: zero probability. Values represent Mean (95% confidence interval).
Nevertheless, analysing genetic effects of IL-12 on parasitemia and anaemia, we did not observe significant associations of either IL-12 genotype or haplotypes with these malaria related phenotypes (Supplementary Table 3).
Correlation of IL-12 genotypes/haplotypes with IL-12 concentrations
IL-12 levels were significantly different in the genotypes of IL-12b rs2288831 (p = 0.030) and rs17860508 (p = 0.036) (Supplementary Table 4). Specifically, the background IL-12 concentrations were lower in children with heterozygous CT for IL-12b rs2288831 than those with homozygous CC (p = 0.078) and TT (p = 0.012) (Fig. 3a). Likewise, children with TTAGAG or GC genotype had significantly or marginally higher levels of background IL-12 than those with heterozygous TTAGAG/GC, respectively (Fig. 3b). Apart from this, we did not observe any other significant effects of host genotype on IL-12 levels.
Cord Blood IL-12 Levels and Children IL-12b Polymorphisms: The cord blood background IL-12 levels and specific IL-12 production after P. falciparum schizont extract stimulation were stratified by children IL-12b genotypes of rs2288831 (a) and rs17860508 (b) using linear regression analysis with adjustment of the confounding effects. Values are Mean (SD).
The host CGTTAGAG haplotype had a significant effect on background IL-12 production (p = 0.018) (Supplementary Table 4). Low probability of CGTTAGAG haplotype was related to low background IL-12 levels and an increased risk of malaria episodes as outlined earlier (Fig. 2), consistent with the effects of the cord blood IL-12 levels on malaria outcome (Table 1).
Impact of maternal immunity on cord blood IL-12 levels
The background levels of IL-12 in cord blood mononuclear cells were positively correlated with those in maternal peripheral blood mononuclear cells (PBMC) (r = 0.343, p < 0.001). However, there was no significant correlation between cord and maternal specific IL-12 production in response to antigen stimulation (r = 0.014, p = 0.845). Further analysis was performed to evaluate the impact of maternal malaria and congenital malaria on maternal and cord blood background IL-12 levels (Fig. 4). The background IL-12 concentrations in maternal peripheral blood were decreased in response to maternal parasitemia, although such change did not reach statistical significance (p = 0.060) (Fig. 4a). However, neither maternal nor cord blood background IL-12 levels differed in women with/without placental infection (Fig. 4b) or in newborns with/without congenital malaria (Fig. 4c)
Maternal/Cord Blood IL-12 Production and Prenatal Malaria Infection: The background IL-12 levels in maternal peripheral blood and cord blood were compared in positive/negative maternal parasitemia (a), positive/negative placental infection (b) and positive/negative cord blood infection (c). Differences between the two groups are compared using independent t test. Values are Mean (SD).
Discussion
Our study showed that children with a high background IL-12 expression in cord blood were highly resistant to the development of malaria episodes. We further established the relationships between host IL-12 polymorphisms and incidence of childhood malaria, which was dependent on maternal genotypes. IL-12 genotypes (IL-12b rs2288831 and rs17860508) and the haplotype CGTTAGAG distribution were related to the background IL-12 levels. In addition, we showed that the cord blood IL-12 levels were associated with the maternal IL-12 levels, which were affected by maternal malaria. Thus, we conclude that the background IL-12 levels in cord blood may be important for protecting young children from Plasmodium infection, likely mediated by the genotypes of children and mothers as well as maternal immunity.
Out of six Th1 pro-inflammatory cytokines investigated, we identified significant associations of IL-12 and IFN-γ at birth with the incidence of malaria infection in the first 2 years of life. Data from animal models of malaria indicated that an early response of both cytokines was essential for parasite clearance, but had to be maintained on a delicate balance to avoid inappropriate induction leading to malaria pathology4. Indeed, in the present study the relationship between these cytokines and disease phenotypes appears to be complex, particularly for IL-12. Specifically, we found that the background IL-12 levels were associated with protection of malaria onset, while Plasmodium-specific IL-12 production was associated with a high risk of malaria episodes, parasitemia and anaemia. However, given the double-edged effects of these cytokines, the contradictory associations are not so unexpected and are consistent with the previous reports19,20. Dodoo et al. demonstrated that the propensity of a person to secrete IL-12, IFN-γ, and TNF was associated with protection against parasitemia, clinical malaria, and anaemia19. On the contrary, the secretory IL-12 induced by the mitogen phytohemagglutinin or Mycobacterium tuberculosis antigen was negatively correlated to haemoglobin concentration19. Similarly, Riley et al. showed that IFN-γ production from PBMC in response to soluble exoantigens of P. falciparum was associated with increased risk of malaria symptoms20, supporting our findings that antigen-induced IFN-γ is a risk factor for increasing malaria susceptibility. Nevertheless, innate IFN-γ response to malaria antigens was reported to be stronger for live than for dead parasites and both γδ T cells and NK cells responded preferentially to live parasites21. These results raise the possibility that a protective IFN-γ response may derive from rapidly activated cell types rather than from memory T cells19. Thus, one of the limitations in the present study is that we investigated the cytokine production responding to schizont lysate, which may be different from live parasites19. However, an in vivo mouse study confirmed that infection with blood-stage lethal P. berghei NK65 induced IL-12 production, which was critically involved in the pathogenesis of liver injury via increasing IFN-γ22. Treatment of these infected mice with neutralizing monoclonal antibodies against IL-12 prolonged the survival and diminished liver injury22. Taken together, although further studies are required to ascertain the role of IL-12 production in response to the parasite infection, our data clearly demonstrated the importance of basal IL-12 levels in protecting children from Plasmodium infection. This finding has significant implications with respect to vaccine design strategy, e.g. up-regulating IL-12 expression in cells rather than directly supplying exogenous IL-12 to increase cellular resistance to infection.
The variation of cytokine production may be related to individual genetic differences19, affecting the outcome of Plasmodium infection. A functional promoter variant (rs17860508) in IL-12b, was found to have a dominant effect on cerebral malaria susceptibility in Tanzanian23 and Malian children24, and Thai population25, but not in Kenyan23 and Burkina Faso subjects26. In our cohort study, we found that heterozygous alleles of both IL-12b rs2288831 and rs17860508 were related to reduced expression of cord blood background IL-12 levels and a high risk of malaria episodes. These observations suggest that IL-12b polymorphisms, via regulation of baseline IL-12 production, influence the outcome of malaria infection. Nevertheless, our data showed that homozygous GC of IL-12b rs17860508 was associated with increased morbidity in 2-year-old Mozambican children, while others demonstrated that homozygosity for the CTCTAA allele affected susceptibility to cerebral malaria24,25. The apparent discrepancy may be explained by the different disease phenotypes observed (clinical episodes in the present study vs severe malaria in other studies23,24,25), particularly considering the different roles of cytokines in malaria progression, or due to the different ethnic groups studied.
Both homozygous alleles of TT and GC in IL-12b rs2288831 and rs17860508 were related to increased incidence of developing clinical malaria, compared to the homozygous alleles of CC and TTAGAG respectively. However, IL-12 levels were comparable between the two groups of homozygosity. We speculated that genetic variants were likely to form a regulatory haplotype to affect the function expression. As expected, construction of haplotypes for the three polymorphisms (IL-12b variants rs2546890, rs2288831 and rs17860508) revealed that carriage of the CGTTAGAG haplotype was associated with a reduced incidence of malaria episodes, while high probability of transmitting the TGGC haplotype was associated with increased susceptibility to the outcome of Plasmodium infection. Moreover, basal IL-12 concentrations were higher in children with the CGTTAGAG haplotype, confirming our hypothesis that the IL-12b haplotype exhibits a cis-regulatory effect on IL-12 expression, contributing to disease protection. However, the distribution of the TGGC haplotype was not related to the cord blood IL-12 levels, and thereby the protective mechanism could not be explained by modulating IL-12 expression. Additional mechanisms (e.g. epistatic effects) may exist, as evidenced by genetic interactions of IL-12 with IL-1027,28, haemoglobin C (Hbc)29 and toll-like receptor 4 (TLR4)30 in mediating IL-12 production or altering malaria related phenotypes.
Similar to the children’s genotypes, association of mothers’ genotypes with clinical malaria showed a similar pattern and consistent direction. Moreover, the impact of children’s genotypes on malaria episodes was attenuated markedly or disappeared, after adjusting for the corresponding maternal genotypes, suggesting a maternal genotype-dependent mechanism underlying host genotype-phenotype interactions. In addition, prenatal exposure to malaria is well documented to increase parasite density and severe malaria risk in offspring. Our data showed a positive correlation of background IL-12 levels between maternal and cord blood. Moreover, maternal malaria seemed to decrease the background IL-12 concentrations in the mother. As such, cord blood IL-12 levels may play a key role in transducing malaria signalling to modify infant susceptibility. It is speculated that owing to the passively acquired malarial antigens from maternal source, the fetal cell is primed and activated to produce the coordinative expression of Th1/Th2 phenotypes in fetal blood31.
In conclusion, we report for the first time that basal expression of IL-12 in cord blood cells confers protection from Plasmodium infection throughout early life. IL-12 genotype/haplotypes alter paediatric malaria susceptibility, which is in part associated with regulating IL-12 expression. Finally, we found that maternal genotype and IL-12 response were associated with the cord blood IL-12 levels and subsequent development of malaria disease in the offspring. It follows that interactions between maternal genetic factors and environment determine childhood malaria outcome, through altering the inherent expression of the cord blood IL-12.
Materials and methods
Participants
This study was part of the AgeMal project (ClinicalTrials.gov identifier NCT00231452) described previously15. The primary aim of this study was to investigate the effect of age of first exposure to malaria on the development of naturally acquired immunity in infants. In summary, the study was a three-arm randomized, double-blind, placebo-controlled trial carried out in a malaria endemic area (Manhiça district of Southern Mozambique) from August 2005 to July 2009. A total of 349 HIV-negative pregnant women and their newborn babies were recruited and followed up until two years of life after birth. The first exposure to P. falciparum was selectively controlled at varying postnatal stages (2 to 5 months, early exposure; 5 to 10 months, late exposure; or none, control) with monthly chemoprophylaxis with sulfadoxine-pyrimethamine and artesunate. However, such strategy did not affect outcomes of P. falciparum infection and antibody response14,15. Written informed consent was obtained from all mothers. The study was approved by the National Mozambican Ethics Review Committee, the Hospital Clinic of Barcelona Ethics Review Committee, and the Princess Margaret Hospital for Children Ethics Committee (1473/EP) in Perth. All experiments were performed in accordance with relevant guidelines and regulations of the Hospital Clinic of Barcelona and the School of Paediatrics and Child Health, the University of Western Australia.
Cytokine measurement
Blood mononuclear cells were isolated from maternal and cord bloods using a lymphoprep gradient, and resuspended in complete RPMI medium. The fresh cells were stimulated with uninfected erythrocytes or P. falciparum schizont extract32. After 24 h culture, IL-1, IL-6, IL-12 (p70 heterodimer), IFN-γ, TNF and TNF-β levels were measured in the culture supernatants using the Bender MedSystems Human Th1/Th2 11plex FlowCytomix multiplex kit and analyzed on a FACS Canto II (Becton Dickinson, Franklin Lakes, NJ, USA)32,33. Cytokine concentrations (pg/ml) measured in this way represented background cytokines without stimulation (uninfected erythrocytes), or cytokine production in response to P. falciparum-specific stimulation. The secretory capacity of cytokines was further expressed by division of background cytokines from the corresponding stimulated cytokines (stimulated cytokine/background cytokine), defined as specific cytokine responses after malaria antigen stimulation.
Disease phenotypic definitions
As described previously15, newborns were followed up weekly (from birth to 10.5 months) or monthly (from 10.5 to 24 months) for malaria case detection and in case of illness, subjected to clinical assessments and blood smear. The case detection included taking axillary temperatures and recording any history of fever. A clinical malaria episode was defined as axillary temperature ≥37.5 °C, or a history of fever within the prior 24 h plus the presence of P. falciparum of any density diagnosed by microscopy. Since the interventions were conducted in the first year of life, a clinical episode of malaria infection during the second year of life was the main phenotype in our analysis. Two other phenotypes, namely anaemia and parasitemia, were also assessed at 24 months of age. Anaemia was defined as haemoglobin <8 g/dl. For childhood parasitemia except assessed by microscopy, qPCR was also used to determine cord blood or peripheral blood P. falciparum copy number in filter paper samples at birth and 24 months of age. Concerning maternal malaria, maternal parasitemia was determined in peripheral blood by microscopy and placental infection was assessed by histology. The laboratory test details were described in our recent paper32.
Genotyping
Genomic DNA from PBMC was purified using an automated DNA extraction instrument (Autopure LS; Qiagen, Hilden, Germany). We selected one SNP rs568408 in IL-12a gene 3′-UTR and three SNPS (IL-12b rs17860508, rs2546890, rs2288831) in IL-12b gene regions. Among these polymorphic markers, IL-12a rs568408, IL-12b rs17860508 and IL-12b rs2546890 were found to be related to malaria infections24,25, while IL-12b rs2288831 was shown to have a strong linkage disequilibrium with IL-12b rs1786050826. The four SNPs were genotyped by using the iPLEX assay on a MALDI-TOF MassARRAY platform (Sequenom, San Diego, CA, USA) in the Australian Genome Research Facility.
Data analysis
The allele and genotype distribution was examined for the Hardy Weinberg Equilibrium (https://regepi.bwh.harvard.edu/IIPGA2/Bioinformatics/) and compared using chi square test. Linkage disequilibrium analysis was performed using Haploview v4.2 software.
Log-transformation was used to normalize the distribution of cytokine values. The associations between cytokine concentrations and disease phenotypes (e.g. anaemia, parasitemia or prenatal malaria) or genotypes/haplotypes were analysed using independent sample t test or one-way ANOVA, respectively. Linear regression was used to verify the associations in children after adjusting for the potential confounders e.g. mother’s age, parity, infant sex, ITNs, IRS, and congenital infection since these factors were known to influence cord cytokine profile and childhood malaria susceptibility17,18,34,35. The variable of intervention group (early, late exposure and control) was fitted in the regression model as an additional adjustment for analysing cytokine association with the malaria disease phenotypes. Poisson regression was used to determine the risk of the incidence of clinical malaria in the second year of life and its association with cytokine production and genotypes/haplotypes of IL-12 with adjustment for the confounding factors outlined above. The Pearson correlation index was calculated to determine the association among different continuous variables using linear regression analysis.
SPSS (version 20.0: SPSS Inc., Chicago, IL, USA) was used for the statistical analyses. Data were presented as mean (95% CI or SD). Differences were accepted as significant at p < 0.05.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding authors on reasonable request.
References
World Health Organization. World Malaria Report http://www.who.int/malaria/publications/world_malaria_report/en/ (2017).
Doolan, D. L., Dobano, C. & Baird, J. K. Acquired immunity to malaria. Clin Microbiol Rev. 22, 13–36 (2009).
Malaguarnera, L. & Musumeci, S. The immune response to Plasmodium falciparum malaria. Lancet Infect Dis. 2, 472–478 (2002).
Angulo, I. & Fresno, M. Cytokines in the pathogenesis of and protection against malaria. Clin Diagn Lab Immunol. 9, 1145–1152 (2002).
Day, N. P. et al. The prognostic and pathophysiologic role of pro- and antiinflammatory cytokines in severe malaria. J Infect Dis. 180, 1288–1297 (1999).
Omer, F. M., Kurtzhals, J. A. & Riley, E. M. Maintaining the immunological balance in parasitic infections: a role for TGF-beta? Parasitol Today. 16, 18–23 (2000).
Phawong, C. et al. Haplotypes of IL12B promoter polymorphisms condition susceptibility to severe malaria and functional changes in cytokine levels in Thai adults. Immunogenetics. 62, 345–356 (2010).
Kern, P., Hemmer, C. J., Van Damme, J., Gruss, H. J. & Dietrich, M. Elevated tumor necrosis factor alpha and interleukin-6 serum levels as markers for complicated Plasmodium falciparum malaria. Am J Med. 87, 139–143 (1989).
Lyke, K. E. et al. Serum levels of the proinflammatory cytokines interleukin-1 beta (IL-1beta), IL-6, IL-8, IL-10, tumor necrosis factor alpha, and IL-12(p70) in Malian children with severe Plasmodium falciparum malaria and matched uncomplicated malaria or healthy controls. Infect Immun. 72, 5630–5637 (2004).
Rockett, K. A., Awburn, M. M., Rockett, E. J. & Clark, I. A. Tumor necrosis factor and interleukin-1 synergy in the context of malaria pathology. Am J Trop Med Hyg. 50, 735–742 (1994).
Malaguarnera, L. et al. Increased levels of interleukin-12 in Plasmodium falciparum malaria: correlation with the severity of disease. Parasite Immunol. 24, 387–389 (2002).
Chaisavaneeyakorn, S. et al. Relationship between plasma Interleukin-12 (IL-12) and IL-18 levels and severe malarial anaemia in an area of holoendemicity in western Kenya. Clin Diagn Lab Immunol. 10, 362–366 (2003).
Perera, M. K. et al. Association of high plasma TNF-alpha levels and TNF-alpha/IL-10 ratios with TNF2 allele in severe P. falciparum malaria patients in Sri Lanka. Pathog Glob Health. 107, 21–29 (2013).
Nhabomba, A. J. et al. Impact of age of first exposure to Plasmodium falciparum on antibody responses to malaria in children: a randomized, controlled trial in Mozambique. Malar J. 13, 121 (2014).
Guinovart, C. et al. The role of age and exposure to Plasmodium falciparum in the rate of acquisition of naturally acquired immunity: a randomized controlled trial. PLoS One. 7, e32362 (2012).
Zhang, G. et al. Interleukin-10 (IL-10) polymorphisms are associated with IL-10 production and clinical malaria in young children. Infect Immun. 80, 2316–2322 (2012).
Schwarz, N. G. et al. Placental malaria increases malaria risk in the first 30 months of life. Clin Infect Dis. 47, 1017–1025 (2008).
Mutabingwa, T. K. et al. Maternal malaria and gravidity interact to modify infant susceptibility to malaria. PLoS Med. 2, e407 (2005).
Dodoo, D. et al. Absolute levels and ratios of proinflammatory and anti-inflammatory cytokine production in vitro predict clinical immunity to Plasmodium falciparum malaria. J Infect Dis. 185, 971–979 (2002).
Riley, E. M. et al. Immune response to soluble exoantigens of Plasmodium falciparum may contribute to both pathogenesis and protection in clinical malaria: evidence from a longitudinal, prospective study of semi-immune African children. Eur J Immunol. 21, 1019–1025 (1991).
Waterfall, M., Black, A. & Riley, E. Gammadelta+T cells preferentially respond to live rather than killed malaria parasites. Infect Immun. 66, 2393–2398 (1998).
Yoshimoto, T. et al. A pathogenic role of IL-12 in blood-stage murine malaria lethal strain Plasmodium berghei NK65 infection. J Immunol. 160, 5500–5505 (1998).
Morahan, G. et al. A promoter polymorphism in the gene encoding interleukin-12p40 (IL12B) is associated with mortality from cerebral malaria and with reduced nitric oxide production. Genes Immun. 3, 414–418 (2002).
Marquet, S. et al. A functional promoter variant in IL12B predisposes to cerebral malaria. Hum Mol Genet. 17, 2190–2195 (2008).
Naka, I. et al. A replication study of the association between the IL12B promoter allele CTCTAA and susceptibility to cerebral malaria in Thai population. Malar J. 8, 290 (2009).
Barbier, M., Atkinson, A., Fumoux, F. & Rihet, P. IL12B polymorphisms are linked but not associated with Plasmodium falciparum parasitemia: a familial study in Burkina Faso. Genes Immun. 9, 405–411 (2008).
Peng, J. C. et al. IL10 and IL12B polymorphisms each influence IL-12p70 secretion by dendritic cells in response to LPS. Immunol Cell Biol. 84, 227–232 (2006).
Yilmaz, V., Yentur, S. P. & Saruhan-Direskeneli, G. IL-12 and IL-10 polymorphisms and their effects on cytokine production. Cytokine. 30, 188–194 (2005).
Atkinson, A., Barbier, M., Afridi, S., Fumoux, F. & Rihet, P. Evidence for epistasis between hemoglobin C and immune genes in human P. falciparum malaria: a family study in Burkina Faso. Genes Immun. 12, 481–489 (2011).
Basu, M. et al. Gene-gene interaction and functional impact of polymorphisms on innate immune genes in controlling Plasmodium falciparum blood infection level. PLoS One. 7, e46441 (2012).
Tse, D. B. & Young, B. K. Co-ordinate expression of Th1/Th2 phenotypes in maternal and fetal blood: evidence for a transplacental nexus. J Perinat Med. 40, 165–170 (2012).
Dobano, C. et al. High production of pro-inflammatory cytokines by maternal blood mononuclear cells is associated with reduced maternal malaria but increased cord blood infection. Malar J. 17, 177 (2018).
Berthoud, T. K. et al. Comparison of commercial kits to measure cytokine responses to Plasmodium falciparum by multiplex microsphere suspension array technology. Malar J. 10, 115 (2011).
Klein, S. L. & Flanagan, K. L. Sex differences in immune responses. Nat Rev Immunol. 16, 626–638 (2016).
Fievet, N. et al. Plasmodium falciparum exposure in utero, maternal age and parity influence the innate activation of foetal antigen presenting cells. Malar J. 8, 251 (2009).
Acknowledgements
The work was supported by a EU Framework Program 6 STREP project (Malaria Age Exposure, project reference no. 18902), the Instituto de Salud Carlos III (Ayuda de incentivación a la participación en proyectos del Espacio Europeo de Investigación), the Spanish Ministerio de Educación y Ciencia (project reference no. A107190024). G.Z. was supported by the BrightSpark Foundation, C.D. was supported by a Ramón y Cajal grant from the Spanish Ministerio de Ciencia e Innovación (RYC-2008-02631), C.G. by a grant from the Spanish Ministry of Health (Contrato post-Formación Sanitaria Especializada, Fondo de Investigaciones Sanitarias, Instituto de Salud Carlos III, reference no. CM04/00028), and A.M. by a Miguel Servet grant from the Instituto de Salud Carlos III (CP-04/00220). The Manhiça Health Research Centre receives core funding from the Spanish Agency for International Cooperation and Development (AECID). ISGlobal is a member of the CERCA Programme, Generalitat de Catalunya. We thank all children and their families for their participation in the study, the field workers, field supervisors, laboratory staff, and other staff at CISM for their work during the study, and Laura Puyol and Sònia Tomás for their support to the study.
Author information
Authors and Affiliations
Contributions
Y.S., R.A., P.N.L., C.D. and G.Z. conceived and designed the study. R.A., M.N.M., A.N., A. B., C.G., P.L.A. and C.D. involved the recruitment and sample collection. R.A., T.K.B., L.Q., A.M., C.G., P.L.A. and C.D. performed phenotypic study and cytokine measurement. S.K.K., S.M., I.A.L. and G.Z. performed genotyping study. Y.S., J.G. and G.Z. performed statistical analysis. Y.S., C.D. and G.Z. prepared the manuscript. R.A., J.G. and T.K.B. contributed to manuscript revision. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Song, Y., Aguilar, R., Guo, J. et al. Cord Blood IL-12 Confers Protection to Clinical Malaria in Early Childhood Life. Sci Rep 8, 10860 (2018). https://doi.org/10.1038/s41598-018-29179-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-29179-y
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.